Korean J Radiol.
2016 Oct;17(5):801-810. 10.3348/kjr.2016.17.5.801.
Stent-Assisted Coil Embolization of Vertebrobasilar Dissecting Aneurysms: Procedural Outcomes and Factors for Recanalization
- Affiliations
-
- 1Department of Neurosurgery, Hallym University College of Medicine, Chuncheon 24253, Korea.
- 2Department of Radiology, Seoul National University College of Medicine, Seoul National University Hospital, Seoul 03080, Korea. aronnn@naver.com
- 3Department of Neurosurgery, Jeju National University College of Medicine, Jeju National University Hospital, Jeju 63241, Korea.
- 4Department of Neurology, Konkuk University Hospital, Konkuk University School of Medicine, Seoul 05030, Korea.
- 5Department of Neurosurgery, Seoul National University College of Medicine, Seoul National University Hospital, Seoul 03080, Korea.
- 6Department of Neurosurgery, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam 13620, Korea.
- KMID: 2458074
- DOI: http://doi.org/10.3348/kjr.2016.17.5.801
Abstract
OBJECTIVE
Outcomes of stent-assisted coil embolization (SACE) have not been well established in the setting of vertebrobasilar dissecting aneurysms (VBDAs) due to the low percentage of cases that need treatment and the array of available therapeutic options. Herein, we presented clinical and radiographic results of SACE in patients with VBDAs.
MATERIALS AND METHODS
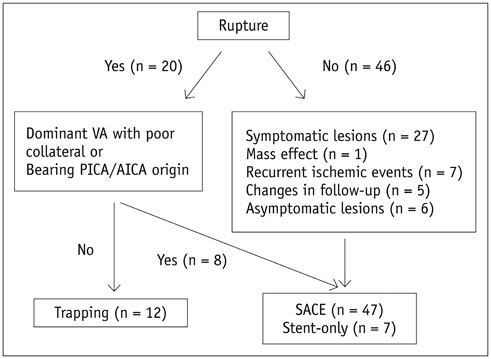
A total of 47 patients (M:F, 30:17; mean age ± SD, 53.7 ± 12.6 years), with a VBDA who underwent SACE between 2008 and 2014 at two institutions were evaluated retrospectively. Medical records and radiologic data were analyzed to assess the outcome of SACE procedures. Cox proportional hazards regression analysis was conducted to determine the factors that were associated with aneurysmal recanalization after SACE.
RESULTS
Stent-assisted coil embolization technically succeeded in all patients. Three cerebellar infarctions occurred on postembolization day 1, week 2, and month 2, but no other procedure-related complications developed. Immediately following SACE, 25 aneurysms (53.2%) showed no contrast filling into the aneurysmal sac. During a mean follow-up of 20.2 months, 37 lesions (78.7%) appeared completely occluded, whereas 10 lesions showed recanalization, 5 of which required additional embolization. Overall recanalization rate was 12.64% per lesion-year, and mean postoperative time to recanalization was 18 months (range, 3-36 months). In multivariable analysis, major branch involvement (hazard ratio [HR]: 7.28; p = 0.013) and the presence of residual sac filling (HR: 8.49, p = 0.044) were identified as statistically significant independent predictors of recanalization. No bleeding was encountered in follow-up monitoring.
CONCLUSION
Stent-assisted coil embolization appears feasible and safe for treatment of VBDAs. Long-term results were acceptable in a majority of patients studied, despite a relatively high rate of incomplete occlusion immediately after SACE. Major branch involvement and coiled aneurysms with residual sac filling may predispose to recanalization.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Intracranial Mirror Aneurysms: Anatomic Characteristics and Treatment Options
Hyun Ho Choi, Young Dae Cho, Dong Hyun Yoo, Jeongjun Lee, Jong Hyeon Mun, Sang Joon An, Hyun-Seung Kang, Won-Sang Cho, Jeong Eun Kim, Moon Hee Han
Korean J Radiol. 2018;19(5):849-858. doi: 10.3348/kjr.2018.19.5.849.
Reference
-
1. Kim BM, Kim SH, Kim DI, Shin YS, Suh SH, Kim DJ, et al. Outcomes and prognostic factors of intracranial unruptured vertebrobasilar artery dissection. Neurology. 2011; 76:1735–1741.2. Ahn JY, Han IB, Kim TG, Yoon PH, Lee YJ, Lee BH, et al. Endovascular treatment of intracranial vertebral artery dissections with stent placement or stent-assisted coiling. AJNR Am J Neuroradiol. 2006; 27:1514–1520.3. Lylyk P, Cohen JE, Ceratto R, Ferrario A, Miranda C. Combined endovascular treatment of dissecting vertebral artery aneurysms by using stents and coils. J Neurosurg. 2001; 94:427–432.4. Lv X, Jiang C, Li Y, Wu Z. Clinical outcomes of ruptured and unruptured vertebral artery-posterior inferior cerebellar artery complex dissecting aneurysms after endovascular embolization. AJNR Am J Neuroradiol. 2010; 31:1232–1235.5. Shin GW, Jeong HW. Endovascular treatment of intracranial vertebral artery dissecting aneurysms: follow up angiographic and clinical results of endovascular treatment in serial cases. Neurointervention. 2015; 10:14–21.6. Debette S, Grond-Ginsbach C, Bodenant M, Kloss M, Engelter S, Metso T, et al. Differential features of carotid and vertebral artery dissections: the CADISP study. Neurology. 2011; 77:1174–1181.7. Kim BM, Shin YS, Kim SH, Suh SH, Ihn YK, Kim DI, et al. Incidence and risk factors of recurrence after endovascular treatment of intracranial vertebrobasilar dissecting aneurysms. Stroke. 2011; 42:2425–2430.8. Park SI, Kim BM, Kim DI, Shin YS, Suh SH, Chung EC, et al. Clinical and angiographic follow-up of stent-only therapy for acute intracranial vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2009; 30:1351–1356.9. Kobayashi N, Murayama Y, Yuki I, Ishibashi T, Ebara M, Arakawa H, et al. Natural course of dissecting vertebrobasilar artery aneurysms without stroke. AJNR Am J Neuroradiol. 2014; 35:1371–1375.10. Jeon P, Kim BM, Kim DI, Park SI, Kim KH, Kim DJ, et al. Reconstructive endovascular treatment of fusiform or ultrawide-neck circumferential aneurysms with multiple overlapping enterprise stents and coiling. AJNR Am J Neuroradiol. 2012; 33:965–971.11. Cho YD, Lee WJ, Kim KM, Kang HS, Kim JE, Han MH. Stent-assisted coil embolization of posterior communicating artery aneurysms. AJNR Am J Neuroradiol. 2013; 34:2171–2176.12. Kang HS, Han MH, Kwon BJ, Jung C, Kim JE, Kwon OK, et al. Is clopidogrel premedication useful to reduce thromboembolic events during coil embolization for unruptured intracranial aneurysms? Neurosurgery. 2010; 67:1371–1376. discussion 1376.13. Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003; 34:1398–1403.14. Cho YD, Han MH, Ahn JH, Jung SC, Kim CH, Kang HS, et al. Simultaneous endovascular treatment of ruptured cerebral aneurysms and vasospasm. Korean J Radiol. 2015; 16:180–187.15. Cho YD, Rhim JK, Kang HS, Park JJ, Jeon JP, Kim JE, et al. Use of triple microcatheters for endovascular treatment of wide-necked intracranial aneurysms: a single center experience. Korean J Radiol. 2015; 16:1109–1118.16. Cho YD, Rhim JK, Park JJ, Jeon JS, Yoo RE, Kang HS, et al. Microcatheter looping to facilitate aneurysm selection in coil embolization of paraclinoid aneurysms. Korean J Radiol. 2015; 16:899–905.17. Cho YD, Lee JY, Seo JH, Lee SJ, Kang HS, Kim JE, et al. Does stent implantation improve the result of repeat embolization in recanalized aneurysms? Neurosurgery. 2012; 71:2 Suppl Operative. ons253–ons259. discussion ons259.18. Wakhloo AK, Mandell J, Gounis MJ, Brooks C, Linfante I, Winer J, et al. Stent-assisted reconstructive endovascular repair of cranial fusiform atherosclerotic and dissecting aneurysms: long-term clinical and angiographic follow-up. Stroke. 2008; 39:3288–3296.19. Suh SH, Kim BM, Chung TS, Kim DI, Kim DJ, Hong CK, et al. Reconstructive endovascular treatment of intracranial fusiform aneurysms: a 1-stage procedure with stent and balloon. AJNR Am J Neuroradiol. 2010; 31:155–160.20. Dabus G, Lin E, Linfante I. Endovascular treatment of fusiform intracranial vertebral artery aneurysms using reconstructive techniques. J Neurointerv Surg. 2014; 6:589–594.21. Suh SH, Kim BM, Park SI, Kim DI, Shin YS, Kim EJ, et al. Stent-assisted coil embolization followed by a stent-within-a-stent technique for ruptured dissecting aneurysms of the intracranial vertebrobasilar artery. Clinical article. J Neurosurg. 2009; 111:48–52.22. Zhao KJ, Zhao R, Huang QH, Xu Y, Hong B, Fang YB, et al. The interaction between stent(s) implantation, PICA involvement, and immediate occlusion degree affect symptomatic intracranial spontaneous vertebral artery dissection aneurysm (sis-VADA) recurrence after reconstructive treatment with stent(s)-assisted coiling. Eur Radiol. 2014; 24:2088–2096.23. Ro A, Kageyama N. Pathomorphometry of ruptured intracranial vertebral arterial dissection: adventitial rupture, dilated lesion, intimal tear, and medial defect. J Neurosurg. 2013; 119:221–227.24. Fiorella D, Albuquerque FC, Masaryk TJ, Rasmussen PA, McDougall CG. Balloon-in-stent technique for the constructive endovascular treatment of "ultra-wide necked" circumferential aneurysms. Neurosurgery. 2005; 57:1218–1227. discussion 1218-1227.25. Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg. 2003; 98:959–966.26. Mizutani T, Miki Y, Kojima H, Suzuki H. Proposed classification of nonatherosclerotic cerebral fusiform and dissecting aneurysms. Neurosurgery. 1999; 45:253–259. discussion 259-260.27. Mizutani T, Kojima H, Asamoto S, Miki Y. Pathological mechanism and three-dimensional structure of cerebral dissecting aneurysms. J Neurosurg. 2001; 94:712–717.28. Ng P, Khangure MS, Phatouros CC, Bynevelt M, ApSimon H, McAuliffe W. Endovascular treatment of intracranial aneurysms with Guglielmi detachable coils: analysis of midterm angiographic and clinical outcomes. Stroke. 2002; 33:210–217.29. Mizutani T. Natural course of intracranial arterial dissections. J Neurosurg. 2011; 114:1037–1044.30. Nakiri GS, Santos AC, Abud TG, Aragon DC, Colli BO, Abud DG. A comparison between magnetic resonance angiography at 3 Teslas (time-of-flight and contrast-enhanced) and flat-panel digital subtraction angiography in the assessment of embolized brain aneurysms. Clinics (Sao Paulo). 2011; 66:641–648.31. Ferré JC, Carsin-Nicol B, Morandi X, Carsin M, de Kersaint-Gilly A, Gauvrit JY, et al. Time-of-flight MR angiography at 3T versus digital subtraction angiography in the imaging follow-up of 51 intracranial aneurysms treated with coils. Eur J Radiol. 2009; 72:365–369.32. Jeon JP, Cho YD, Rhim JK, Park JJ, Cho WS, Kang HS, et al. Effect of stenting on progressive occlusion of small unruptured saccular intracranial aneurysms with residual sac immediately after coil embolization: a propensity score analysis. J Neurointerv Surg. 2015; 10. 27. [Epub]. DOI: 10.1136/neurintsurg-2015-011947.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of Stent-assisted Coil Embolization of Wide-necked Intracranial Aneurysms Using the Solitaire(TM) AB Neurovascular Remodeling Device
- Endovascular Treatment of Intracranial Vertebral Artery Dissecting Aneurysms: Follow up Angiographic and Clinical Results of Endovascular Treatment in Serial Cases
- A Complicated Case of Endovascular Stent Assisted Coil Embolization of an Aneurysm
- Comparison of Stent-Assisted Coil Embolization Versus Coil Embolization Alone for Ruptured Cerebral Aneurysms with Mild Symptoms: A Single-Clinic Experience
- Subarachnoid Hemorrhage from a Dissecting Aneurysm of the Posterior Cerebral Artery in a Child : Rebleeding after Stent-Assisted Coiling Followed by Stent-Within-Stent Technique