J Korean Neurosurg Soc.
2017 Sep;60(5):567-576. 10.3340/jkns.2017.0404.001.
A Lower T1 Slope as a Predictor of Subsidence in Anterior Cervical Discectomy and Fusion with Stand-Alone Cages
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea. md6576@naver.com
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 3Department of Neurosurgery, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2457964
- DOI: http://doi.org/10.3340/jkns.2017.0404.001
Abstract
OBJECTIVE
Preoperative parameters including the T1 slope (T1S) and C2-C7 sagittal vertical axis (SVA) have been recognized as predictors of kyphosis after laminoplasty, which is accompanied by posterior neck muscle damage. The importance of preoperative parameters has been under-estimated in anterior cervical discectomy and fusion (ACDF) because there is no posterior neck muscle damage. We aimed to determine whether postoperative subsidence and pseudarthrosis could be predicted according to specific parameters on preoperative plain radiographs.
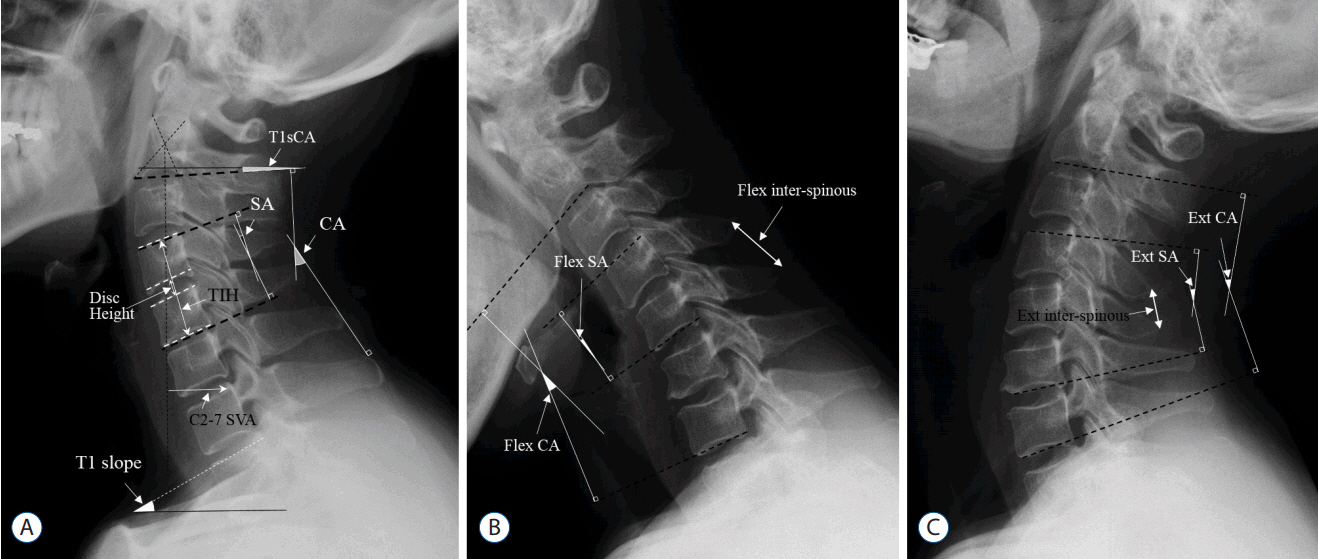
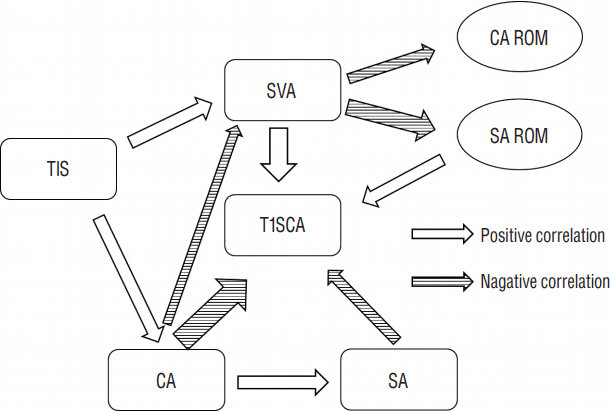
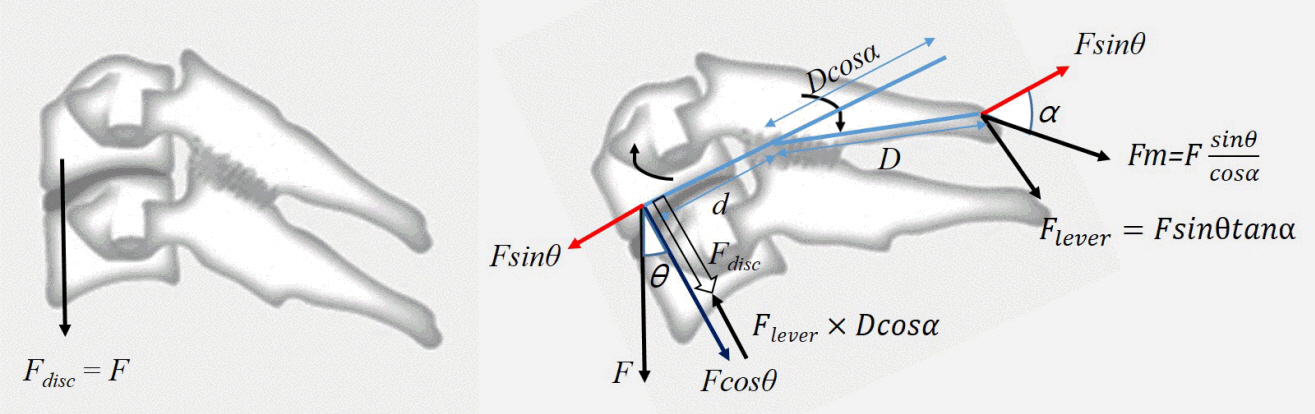
METHODS
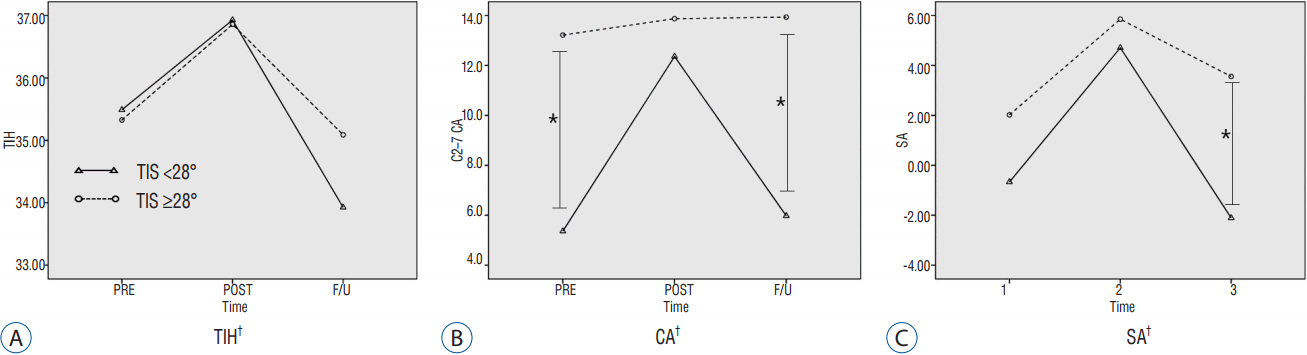
We retrospectively analyzed 41 consecutive patients (male: female, 22: 19; mean age, 51.15±9.25 years) who underwent ACDF with a stand-alone polyether-ether-ketone (PEEK) cage (>1 year follow-up). Parameters including SVA, T1S, segmental angle and range of motion (ROM), C2-C7 cervical angle and ROM, and segmental inter-spinous distance were measured on preoperative plain radiographs. Risk factors of subsidence and pseudarthrosis were determined using multivariate logistic regression.
RESULTS
Fifty-five segments (27 single-segment and 14 two-segment fusions) were included. The subsidence and pseudarthrosis rates based on the number of segments were 36.4% and 29.1%, respectively. Demographic data and fusion level were unrelated to subsidence. A greater T1S was associated with a lower risk of subsidence (p=0.017, odds ratio=0.206). A cutoff value of T1S<28° significantly predicted subsidence (sensitivity: 70%, specificity: 68.6%). There were no preoperative predictors of pseudarthrosis except old age.
CONCLUSION
A lower T1S (T1S<28°) could be a risk factor of subsidence following ACDF. Surgeons need to be aware of this risk factor and should consider various supportive procedures to reduce the subsidence rates for such cases.
MeSH Terms
Figure
Cited by 1 articles
-
Risk Factors of Allogenous Bone Graft Collapse in Two-Level Anterior Cervical Discectomy and Fusion
Joon-Bum Woo, Dong-Wuk Son, Su-Hun Lee, Jun-Seok Lee, Sang Weon Lee, Geun Sung Song
J Korean Neurosurg Soc. 2019;62(4):450-457. doi: 10.3340/jkns.2019.0008.
Reference
-
References
1. Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976). 38(22 Suppl 1):S149–S160. 2013.2. Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 16:1395–1400. 2007.
Article3. Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 58:502–508. discussion 502–508. 2006.
Article4. Brenke C, Dostal M, Scharf J, Weiss C, Schmieder K, Barth M. Influence of cervical bone mineral density on cage subsidence in patients following stand-alone anterior cervical discectomy and fusion. Eur Spine J. 24:2832–2840. 2015.
Article5. Cho JH, Ha JK, Kim DG, Song KY, Kim YT, Hwang CJ, et al. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine (Phila Pa 1976). 39:E1575–E1581. 2014.
Article6. Francke EI, Demetropoulos CK, Agabegi SS, Truumees E, Herkowitz HN. Distractive force relative to initial graft compression in an in vivo anterior cervical discectomy and fusion model. Spine (Phila Pa 1976). 35:526–530. 2010.
Article7. Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 15:1017–1022. 2008.
Article8. Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 12:513–516. 2003.
Article9. Gillis CC, Kaszuba MC, Traynelis VC. Cervical radiographic parameters in 1- and 2-level anterior cervical discectomy and fusion. J Neurosurg Spine. 25:421–429. 2016.
Article10. Gum JL, Glassman SD, Douglas LR, Carreon LY. Correlation between cervical spine sagittal alignment and clinical outcome after anterior cervical discectomy and fusion. Am J Orthop (Belle Mead NJ). 41:E81–E84. 2012.11. Harrison DD, Troyanovich SJ, Harrison DE, Janik TJ, Murphy DJ. A normal sagittal spinal configuration: a desirable clinical outcome. J Manipulative Physiol Ther. 19:398–405. 1996.12. Huang DN, Yu M, Xu NF, Li M, Wang SB, Sun Y, et al. The relationship between changes of cervical sagittal alignment after anterior cervical discectomy and fusion and spino-pelvic sagittal alignment under roussouly classification: a four-year follow-up study. BMC Musculoskelet Disord. 18:87. 2017.
Article13. Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Relationship between T1 slope and cervical alignment following multilevel posterior cervical fusion surgery: impact of T1 slope minus cervical lordosis. Spine (Phila Pa 1976). 41:E396–E402. 2016.14. Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 12:50–56. 1999.
Article15. Kim B, Yoon DH, Ha Y, Yi S, Shin DA, Lee CK, et al. Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J. 16:219–225. 2016.
Article16. Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976). 38:E992–E997. 2013.
Article17. Kim WB, Hyun SJ, Choi H, Kim KJ, Jahng TA, Kim HJ. Long-term follow-up results of anterior cervical inter-body fusion with stand-alone cages. J Korean Neurosurg Soc. 59:385–391. 2016.
Article18. Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 10:994–998. 2010.
Article19. Kwon WK, Kim PS, Ahn SY, Song JY, Kim JH, Park YK, et al. Analysis of associating factors with C2–7 sagittal vertical axis after two-level anterior cervical fusion: comparison between plate augmentation and stand-alone cages. Spine (Phila Pa 1976). 42:318–325. 2017.
Article20. Lee YS, Kim YB, Park SW. Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine (Phila Pa 1976). 39:1280–1287. 2014.
Article21. Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, et al. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine (Phila Pa 1976). 26:951–956. 2001.
Article22. Lin S, Zhou F, Sun Y, Chen Z, Zhang F, Pan S. The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J. 24:127–135. 2015.
Article23. Nolan JP Jr, Sherk HH. Biomechanical evaluation of the extensor musculature of the cervical spine. Spine (Phila Pa 1976). 13:9–11. 1988.
Article24. Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 166:23–28. 1958.
Article25. Park JY, Choi KY, Moon BJ, Hur H, Jang JW, Lee JK. Subsidence after single-level anterior cervical fusion with a stand-alone cage. J Clin Neurosci. 33:83–88. 2016.
Article26. Sakai K, Yoshii T, Hirai T, Arai Y, Torigoe I, Tomori M, et al. Cervical sagittal imbalance is a predictor of kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Spine (Phila Pa 1976). 41:299–305. 2016.
Article27. Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 4:447–453. 2006.
Article28. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 40-A:607–624. 1958.
Article29. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 76:Suppl 1. S14–S21. discussion S21. 2015.
Article30. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 71:662–669. discussion 669. 2012.
Article31. Thomé C, Leheta O, Krauss JK, Zevgaridis D. A prospective randomized comparison of rectangular titanium cage fusion and iliac crest autograft fusion in patients undergoing anterior cervical discectomy. J Neurosurg Spine. 4:1–9. 2006.
Article32. Tomé-Bermejo F, Morales-Valencia JA, Moreno-Pérez J, Marfil-Pérez J, Díaz-Dominguez E, Piñera AR, et al. Long-term changes in sagittal alignment and its clinical implications after cervical interbody fusion cage subsidence for degenerative cervical disc disease. A prospective study with standalone lordotic tantalum cages. Clin Spine Surg. 2016; [Epub ahead of print].33. Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 3:16–23. 2011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Two Different Cervical Interbody Fusion Cages in One Level Stand-alone ACDF: Carbon Fiber Composite Frame Cage Versus Polyetheretherketone Cage
- Anterior Cervical Discectomy and Fusion Using a Stand-Alone Polyetheretherketone Cage Packed with Local Autobone : Assessment of Bone Fusion and Subsidence
- Stand-Alone Cages for Anterior Cervical Fusion: Are There No Problems?
- How Subsidence Affects Clinical and Radiological Outcomes after Stand-Alone Anterior Cervical Discectomy and Fusion on Patients with Degenerative Cervical Disease? A Long-Term Follow-Up Study
- Stand-Alone Cervical Cages in 2-Level Anterior Interbody Fusion in Cervical Spondylotic Myelopathy: Results from a Minimum 2-Year Follow-up