J Korean Neurosurg Soc.
2019 Sep;62(5):594-602. 10.3340/jkns.2019.0086.
Percutaneous Vertebroplasty versus Conservative Treatment Using a Transdermal Fentanyl Patch for Osteoporotic Vertebral Compression Fractures
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jhpark@amc.seoul.kr
- 2Department of Neurosurgery, Inje Universiry Ilsan Paik Hospital, Neuroscience & Radiosurgery hybrid Research Center, Inje Universiry College of Medicine, Ilsan, Korea.
- 3Department of Orthopaedic Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 2457950
- DOI: http://doi.org/10.3340/jkns.2019.0086
Abstract
OBJECTIVE
Although surgical intervention, such as percutaneous vertebroplasty (PVP), is the standard treatment for osteoporotic vertebral compression fractures (OVCFs), its effectiveness and safety are unclear. Therefore, this study compared the safety and efficacy of conservative treatment with that of PVP for acute OVCFs.
METHODS
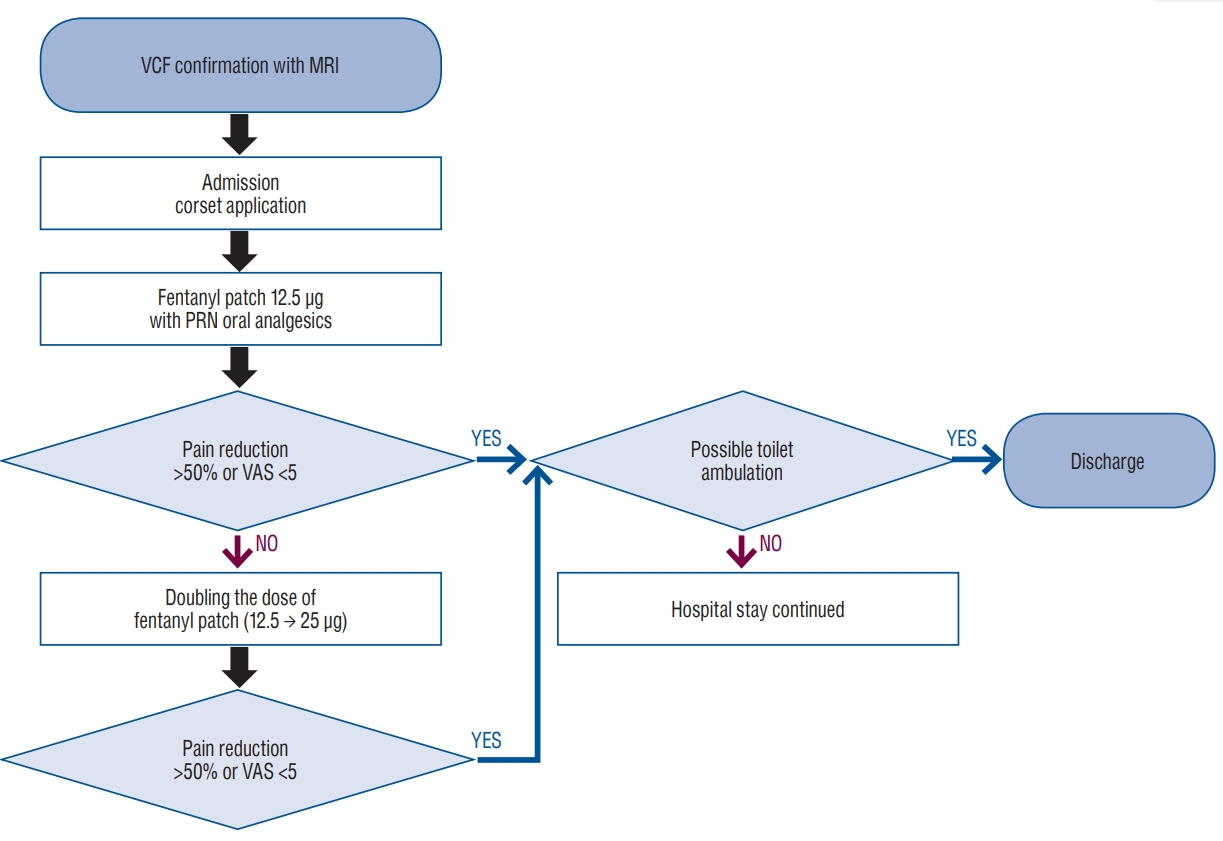
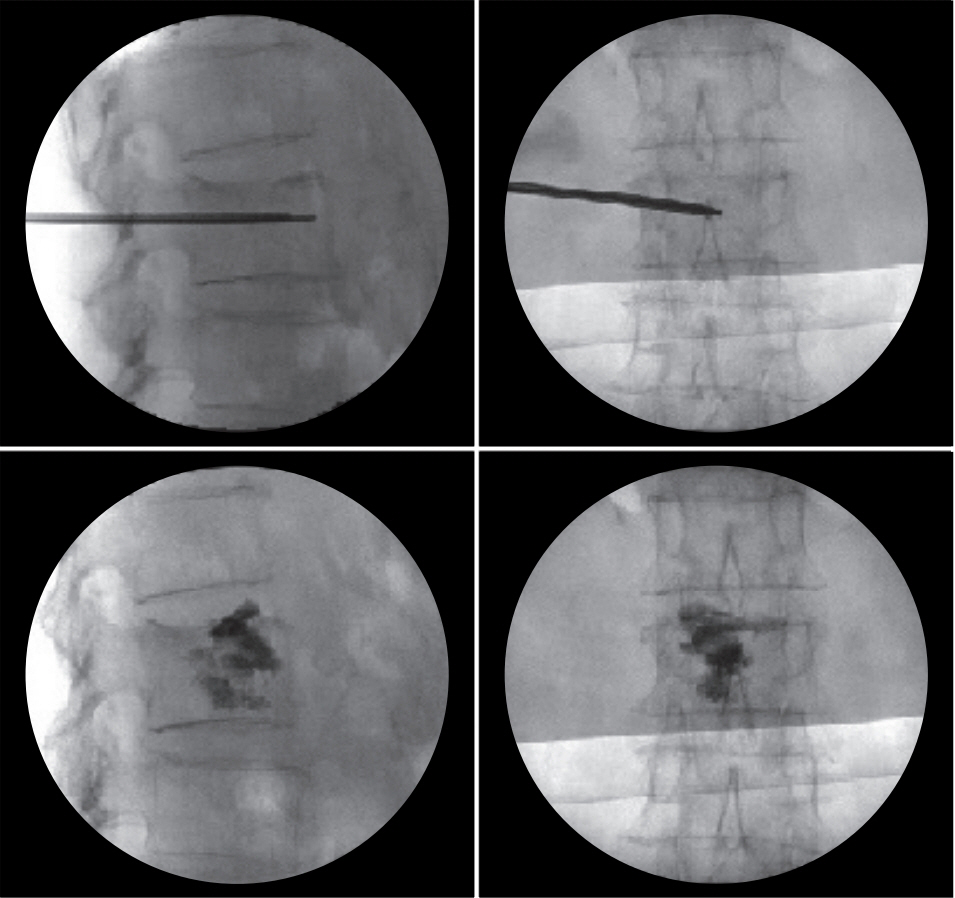
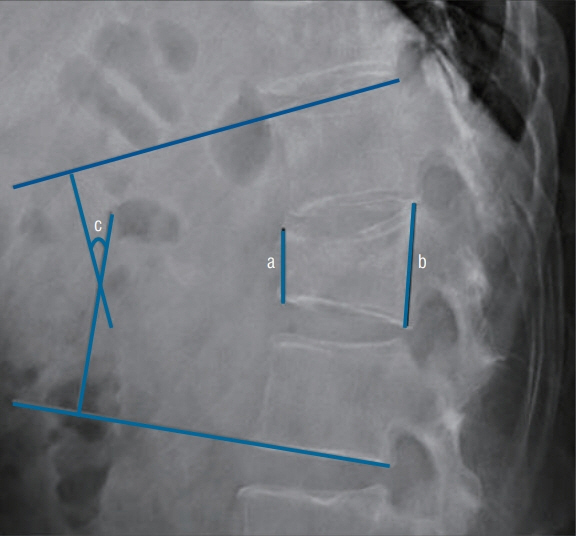
Patients with single-level OVCFs who were treated conservatively with a transdermal fentanyl patch (TFP) or with PVP between March 2013 and December 2017 and followed-up for more than 1 year were retrospectively evaluated. Patients with pathologic fractures, fractures of more than two columns, or a history of PVP were excluded. Clinical outcomes (visual analog scale [VAS] scores) and radiographic factors were evaluated, including changes in the compression rate of the corresponding vertebral body at onset and after 12 months, sagittal Cobb angle at onset and after 6 and 12 months, and the incidence of adjacent compression fractures.
RESULTS
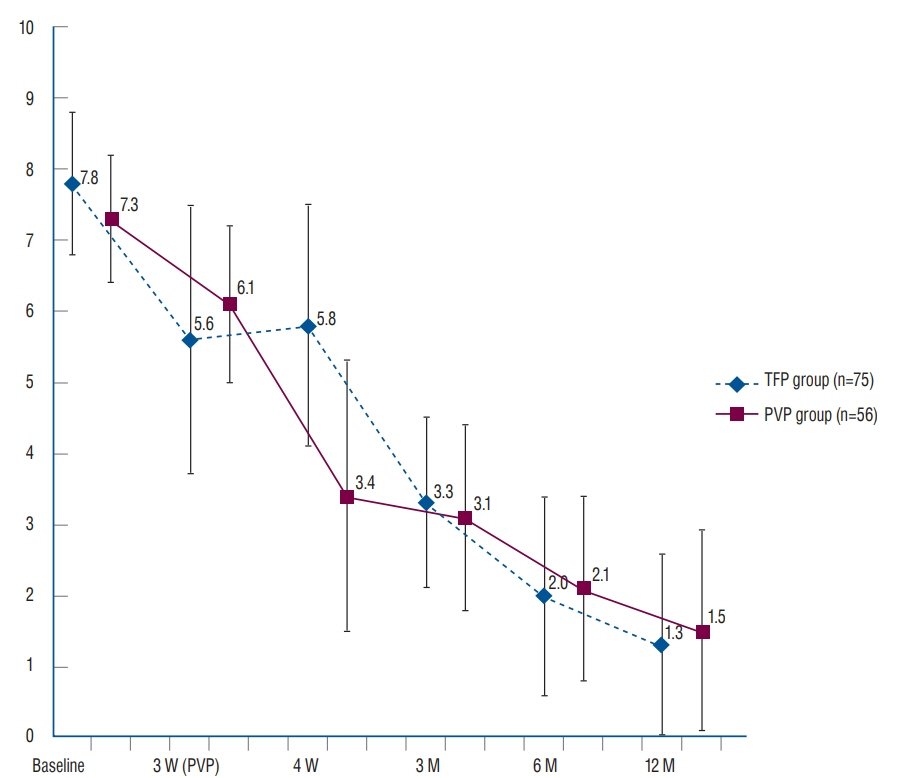
Of the 131 patients evaluated, 75 were treated conservatively using TFPs and 56 underwent PVP. We divided the patients into TFP and PVP groups. Their baseline characteristics (including sex, level of fracture, and bone mineral density T-scores) were similar, but the TFP group was significantly younger. The overall VAS score for pain showed a greater decrease during the first month (1 week after PVP) in the PVP group but remained similar in the two groups thereafter. The compression rate after 12 months increased in the TFP group but decreased in the PVP group. Five patients in the PVP group, but none in the TFP group, experienced adjacent compression fractures within 12 months.
CONCLUSION
We compared clinical and radiological outcomes between the TFP and PVP groups. The immediate pain reduction effect was superior in the PVP group, but the final clinical outcome was similar. Although the PVP group had a better-preserved compression rate than the TFP group for 1 year, the development of adjacent fractures was significantly higher. Although TFPs seemed to be beneficial in reducing the failure rate of conservative treatment, the possibility of side effects (22.6%, 17 out of 75 patients, in this study) should be carefully monitored.
MeSH Terms
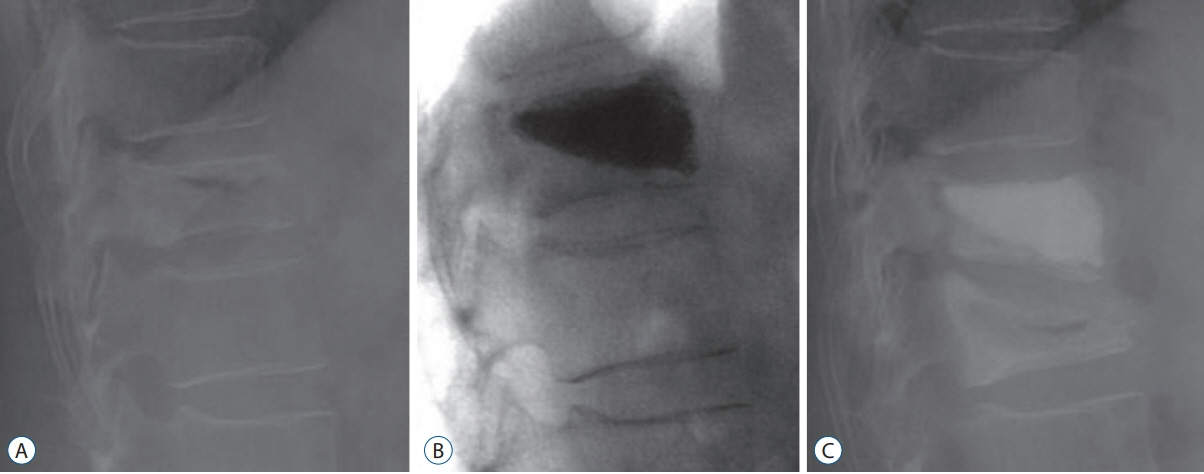
Figure
Reference
-
References
1. Anselmetti GC, Bernard J, Blattert T, Court C, Fagan D, Fransen H, et al. Criteria for the appropriate treatment of osteoporotic vertebral compression fractures. Pain Physician. 16:E519–E530. 2013.2. Choi JH, Kang HD, Park JH, Gu BS, Jung SK, Oh SH. The efficacy of fentanyl transdermal patch as the first-line medicine for the conservative treatment of osteoporotic compression fracture. Korean J Neurotrauma. 13:130–136. 2017.
Article3. Cui R, Zhou L, Li Z, Li Q, Qi Z, Zhang J. Assessment risk of osteoporosis in Chinese people: relationship among body mass index, serum lipid profiles, blood glucose, and bone mineral density. Clin Interv Aging. 11:887–895. 2016.4. Grond S, Radbruch L, Lehmann KA. Clinical pharmacokinetics of transdermal opioids: focus on transdermal fentanyl. Clin Pharmacokinet. 38:59–89. 2000.5. Han S, Wan S, Ning L, Tong Y, Zhang J, Fan S. Percutaneous vertebroplasty versus balloon kyphoplasty for treatment of osteoporotic vertebral compression fracture: a meta-analysis of randomised and nonrandomised controlled trials. Int Orthop. 35:1349–1358. 2011.
Article6. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 17:1726–1733. 2006.
Article7. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 361:569–579. 2009.
Article8. Kamano H, Hiwatashi A, Kobayashi N, Fuwa S, Takahashi O, Saida Y, et al. New vertebral compression fractures after prophylactic vertebroplasty in osteoporotic patients. AJR Am J Roentgenol. 197:451–456. 2011.
Article9. Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 376:1085–1092. 2010.
Article10. Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. Spine J. 12:998–1005. 2012.
Article11. Li HM, Zhang RJ, Gao H, Jia CY, Zhang JX, Dong FL, et al. New vertebral fractures after osteoporotic vertebral compression fracture between balloon kyphoplasty and nonsurgical treatment PRISMA. Medicine (Baltimore). 97:e12666. 2018.
Article12. Lin H, Bao LH, Zhu XF, Qian C, Chen X, Han ZB. Analysis of recurrent fracture of a new vertebral body after percutaneous vertebroplasty in patients with osteoporosis. Orthop Surg. 2:119–123. 2010.
Article13. Lin WC, Cheng TT, Lee YC, Wang TN, Cheng YF, Lui CC, et al. New vertebral osteoporotic compression fractures after percutaneous vertebroplasty: retrospective analysis of risk factors. J Vasc Interv Radiol. 19(2 Pt 1):225–231. 2008.
Article14. Movrin I. Adjacent level fracture after osteoporotic vertebral compression fracture: a nonrandomized prospective study comparing balloon kyphoplasty with conservative therapy. Wien Klin Wochenschr. 124:304–311. 2012.
Article15. Nieuwenhuijse MJ, Putter H, van Erkel AR, Dijkstra PD. New vertebral fractures after percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures: a clustered analysis and the relevance of intradiskal cement leakage. Radiology. 266:862–870. 2013.
Article16. Papanastassiou ID, Filis A, Gerochristou MA, Vrionis FD. Controversial issues in kyphoplasty and vertebroplasty in osteoporotic vertebral fractures. Biomed Res Int. 2014:934206. 2014.
Article17. Park JH, Kim JH, Yun SC, Roh SW, Rhim SC, Kim CJ, et al. Evaluation of efficacy and safety of fentanyl transdermal patch (Durogesic D-TRANS) in chronic pain. Acta Neurochir (Wien). 153:181–190. 2011.
Article18. Pflugmacher R, Schroeder RJ, Klostermann CK. Incidence of adjacent vertebral fractures in patients treated with balloon kyphoplasty: two years’ prospective follow-up. Acta Radiol. 47:830–840. 2006.
Article19. Rousing R, Hansen KL, Andersen MO, Jespersen SM, Thomsen K, Lauritsen JM. Twelve-months follow-up in forty-nine patients with acute/ semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine (Phila Pa 1976). 35:478–482. 2010.
Article20. Rzewuska M, Ferreira M, McLachlan AJ, Machado GC, Maher CG. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J. 24:702–714. 2015.
Article21. Silverman SL. The clinical consequences of vertebral compression fracture. Bone 13 Suppl. 2:S27–S31. 1992.
Article22. Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 226:119–124. 2003.
Article23. Voormolen MH, Lohle PN, Juttmann JR, van der Graaf Y, Fransen H, Lampmann LE. The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol. 17:71–76. 2006.
Article24. Xie L, Zhao ZG, Zhang SJ, Hu YB. Percutaneous vertebroplasty versus conservative treatment for osteoporotic vertebral compression fractures: an updated meta-analysis of prospective randomized controlled trials. Int J Surg. 47:25–32. 2017.
Article25. Yang EZ, Xu JG, Huang GZ, Xiao WZ, Liu XK, Zeng BF, et al. Percutaneous vertebroplasty versus conservative treatment in aged patients with acute osteoporotic vertebral compression fractures: a prospective randomized controlled clinical study. Spine (Phila Pa 1976). 41:653–660. 2016.
Article26. Yi HJ, Jeong JH, Im SB, Lee JK. Percutaneous vertebroplasty versus conservative treatment for one level thoracolumbar osteoporotic compression fracture: results of an over 2-year follow-up. Pain Physician. 19:E743–E750. 2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of Fentanyl Transdermal Patch as the First-Line Medicine for the Conservative Treatment of Osteoporotic Compression Fracture
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures
- Percutaneous Vertebroplasty for Pregnancy-Associated Osteoporotic Vertebral Compression Fractures
- Complication of the Augmented Vertebral Body after Percutaneous Vertebroplasty in Patients with Osteoporotic Compression Fracture: Hammer Effect: Preliminary Report
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture