J Korean Soc Radiol.
2019 Jul;80(4):631-642. 10.3348/jksr.2019.80.4.631.
Recent Advances in Ureteral Stents
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jhshin@amc.seoul.kr
- KMID: 2457443
- DOI: http://doi.org/10.3348/jksr.2019.80.4.631
Abstract
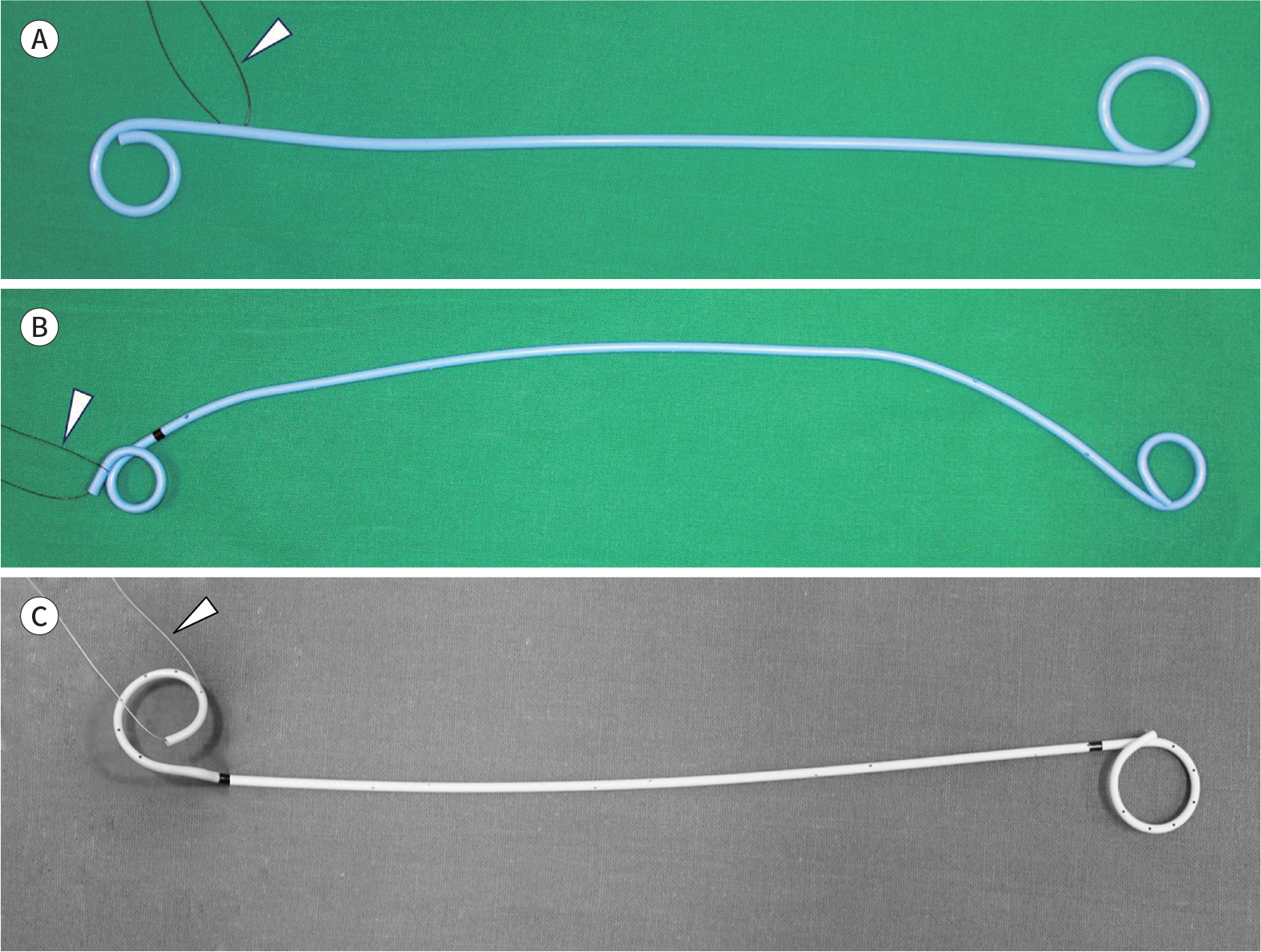
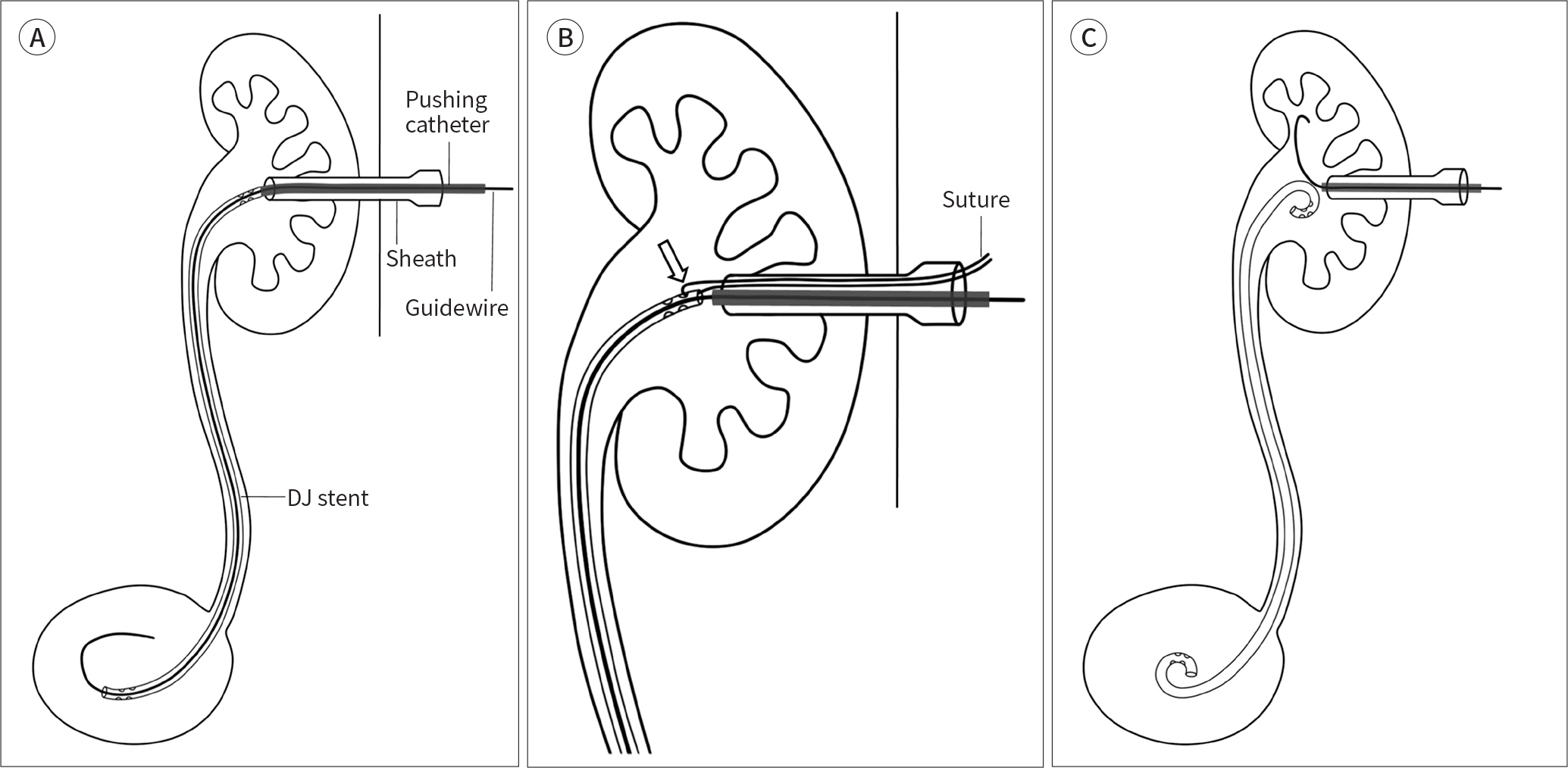
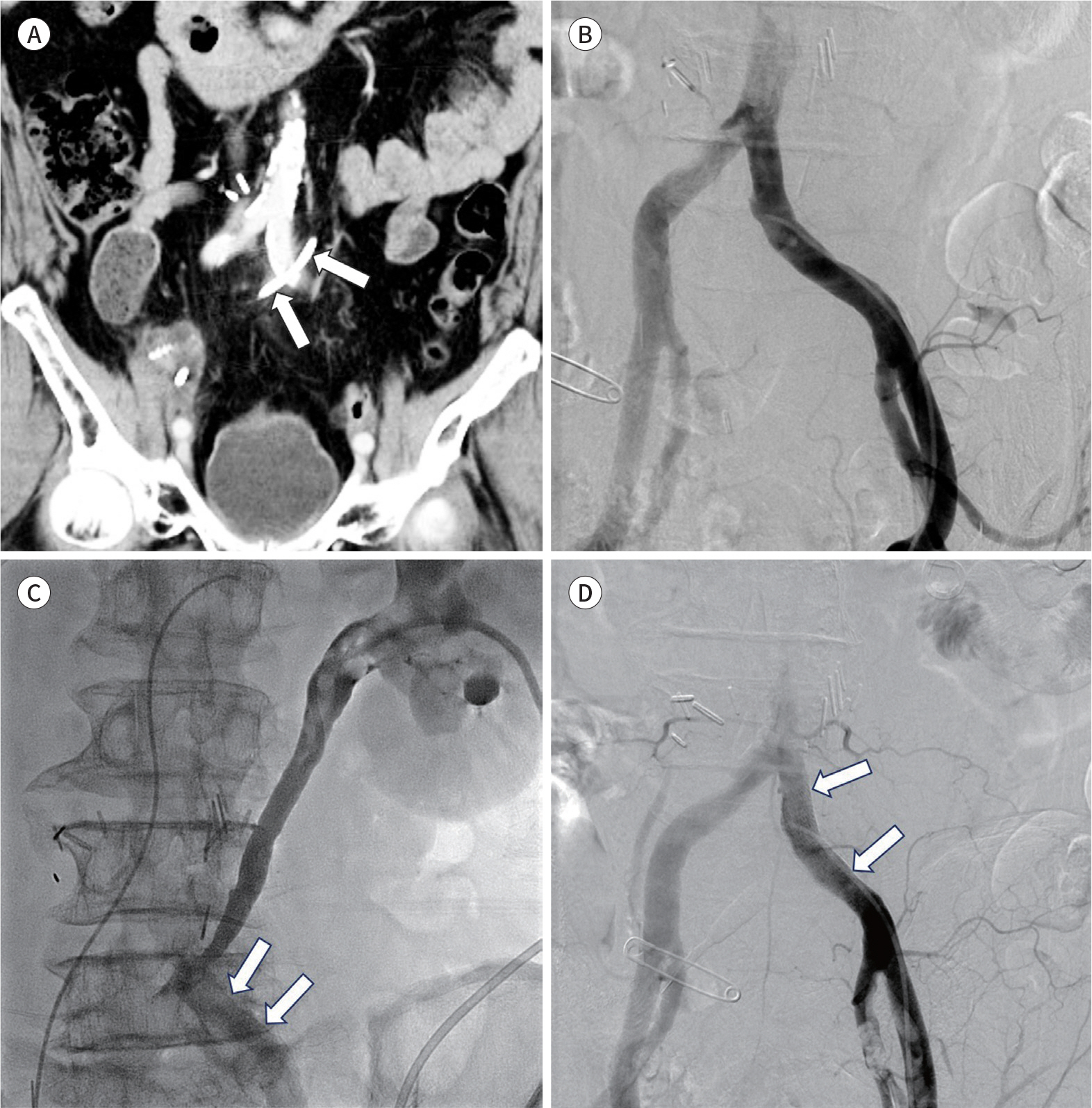
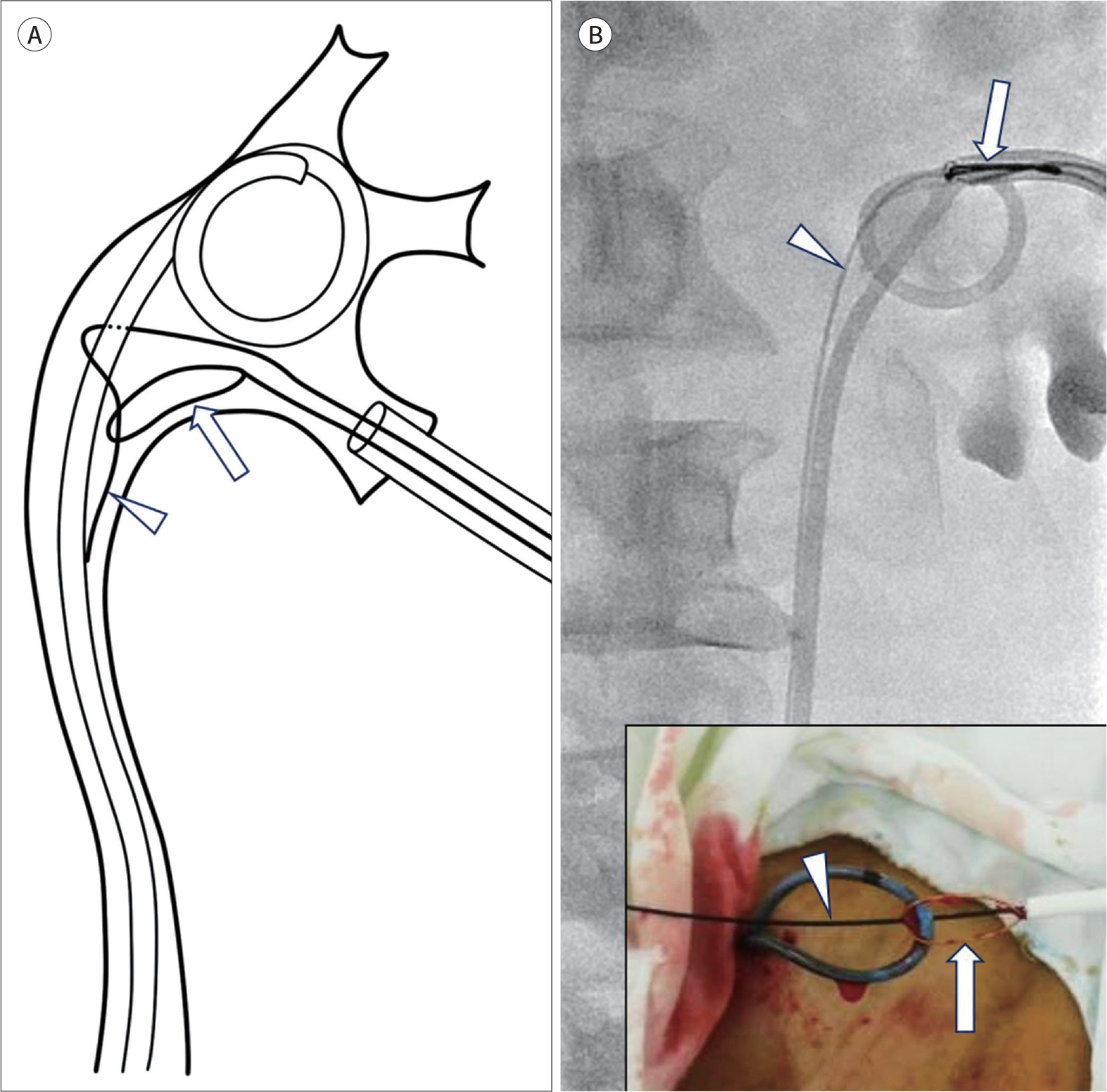
- A ureteral stent is widely used to drain ureteral obstructions, which allows urine to bypass the obstruction. The double J stent, a representative ureteral stent, has undergone many advancements in material and design recently. In addition, indications of double J stent insertion have been broadly expanded to improve urinary obstruction before and after extracorporeal shock wave lithotripsy and to maintain ureteral patency after a ureteral surgery or treatment of a ureteral fistula. The recently developed metallic ureteral stents showed excellent long-term patency in patients with malignant ureteral strictures. Therefore, metallic stents could be an alternative to double J stents in select patients. In this review article, we describe the materials, designs, indications, details of the antegrade ureteral stenting procedure, and outcomes of the double J stent and metallic stent procedures.
MeSH Terms
Figure
Reference
-
References
1. Mosayyebi A, Manes C, Carugo D, Somani BK. Advances in ureteral stent design and materials.Curr Urol Rep. 2018; 19:35.2. Zimskind PD, Fetter TR, Wilkerson JL. Clinical use of longterm indwelling silicone rubber ureteral splints inserted cystoscopically. J Urol. 1967; 97:840–844.
Article3. Finney RP. Experience with new double J ureteral catheter stent. J Urol. 1978; 120:678–681.
Article4. Kim JW, Hong B, Shin JH, Park J, Kim JH, Gwon DI, et al. A prospective randomized comparison of a covered metallic ureteral stent and a double-J stent for malignant ureteral obstruction. Korean J Radiol. 2018; 19:606–612.
Article5. Kim JH, Song K, Jo MK, Park JW. Palliative care of malignant ureteral obstruction with polytetrafluoroethylene membrane-covered self-expandable metallic stents: initial experience.Korean J Urol. 2012; 53:625–631.6. Chow PM, Chiang IN, Chen CY, Huang KH, Hsu JS, Wang SM, et al. Malignant ureteral obstruction: functional duration of metallic versus polymeric ureteral stents. PLoS One. 2015; 10:e0135566.
Article7. Asakawa J, Iguchi T, Tamada S, Ninomiya N, Kato M, Yamasaki T, et al. Treatment outcomes of ureteral stenting for malignant extrinsic ureteral obstruction: a comparison between polymeric and metallic stents. Cancer Manag Res. 2018; 10:2977–2982.
Article8. Dyer RB, Chen MY, Zagoria RJ, Regan JD, Hood CG, Kavanagh PV. Complications of ureteral stent placement. Radiographics. 2002; 22:1005–1022.
Article9. Al-Aown A, Kyriazis I, Kallidonis P, Kraniotis P, Rigopoulos C, Karnabatidis D, et al. Ureteral stents: new ideas, new designs. Ther Adv Urol. 2010; 2:85–92.
Article10. Youn SY, Oh JS, Lee HG, Choi BG, Chun HJ, Kim EH. Primary and secondary percutaneous ureteral stent placement: comparison of stent patency and clinical outcome. Cardiovasc Intervent Radiol. 2018; 41:130–136.
Article11. Patel U, Abubacker MZ. Ureteral stent placement without postprocedural nephrostomy tube: experience in 41 patients. Radiology. 2004; 230:435–442.
Article12. Watson GM, Patel U. Primary antegrade ureteric stenting: prospective experience and cost-effectiveness analysis in 50 ureters. Cl/iin Radiol. 2001; 56:568–574.
Article13. Van der Meer RW, Weltings S, Van Erkel AR, Roshani H, Elzevier HW, Van Dijk LC, et al. Antegrade ureteral stenting is a good alternative for the retrograde approach.Curr Urol. 2017; 10:87–91.14. Chung SY, Stein RJ, Landsittel D, Davies BJ, Cuellar DC, Hrebinko RL, et al. 15-year experience with the management of extrinsic ureteral obstruction with indwelling ureteral stents.J Urol. 2004; 172:592–595.15. Yossepowitch O, Lifshitz DA, Dekel Y, Gross M, Keidar DM, Neuman M, et al. Predicting the success of retrograde stenting for managing ureteral obstruction.J Urol. 2001; 166:1746–1749.16. Fine H, Gordon RL, Lebensart PD. Extracorporeal shock wave lithotripsy and stents: fluoroscopic observations and a hypothesis on the mechanisms of stent function. Urol Radiol. 1989; 11:37–41.
Article17. Watson G. Problems with double-J stents and nephrostomy tubes.J Endourol. 1997; 11:413–417.18. Saltzman B. Ureteral stents. Indications, variations, and complications.Urol Clin North Am. 1988; 15:481–491.
Article19. Matsuura H, Arase S, Hori Y. Ureteral stents for malignant extrinsic ureteral obstruction: outcomes and factors predicting stent failure.Int J Clin Oncol. 2019; 24:306–312.20. Chung HH, Kim MD, Won JY, Won JH, Cho SB, Seo TS, et al. Multicenter experience of the newly designed covered metallic ureteral stent for malignant ureteral occlusion: comparison with double J stent insertion. Cardiovasc Intervent Radiol. 2014; 37:463–470.
Article21. Lange D, Bidnur S, Hoag N, Chew BH. Ureteral stent-associated complications–where we are and where we are going.Nat Rev Urol. 2015; 12:17–25.22. Kawahara T, Ito H, Terao H, Yoshida M, Matsuzaki J. Ureteral stent encrustation, incrustation, and coloring: morbidity related to indwelling times.J Endourol. 2012; 26:178–182.23. Docimo SG, Dewolf WC. High failure rate of indwelling ureteral stents in patients with extrinsic obstruction: experience at 2 institutions. J Urol. 1989; 142:277–279.
Article24. Bergqvist D, Pärsson H, Sherif A. Arterio-ureteral fistula–a systematic review. Eur J Vasc Endovasc Surg. 2001; 22:191–196.25. Pillai AK, Anderson ME, Reddick MA, Sutphin PD, Kalva SP. Ureteroarterial fistula: diagnosis and management.A JR Am J Roentgenol. 2015; 204:W592–W598.26. Muraoka N, Sakai T, Kimura H, Kosaka N, Itoh H, Tanase K, et al. Endovascular treatment for an iliac artery-ureteral fistula with a covered stent. J Vasc Interv Radiol. 2006; 17:1681–1685.
Article27. Eisner BH, McGovern FJ. Management of ureteroiliac artery fistula.Semin Intervent Radiol. 2007; 24:117–118.28. Horikawa M, Saito H, Hokotate H, Mori T. Treatment of ureteroarterial fistula with an endoureteral stent graft. J Vasc Interv Radiol. 2012; 23:1241–1243.
Article29. LeRoy AJ, Williams HJ Jr, Segura JW, Patterson DE, Benson RC Jr. Indwelling ureteral stents: percutaneous management of complications. Radiology. 1986; 158:219–222.
Article30. Shin JH, Yoon HK, Ko GY, Sung KB, Song HY, Choi E, et al. Percutaneous antegrade removal of double J ureteral stents via a 9-F nephrostomy route. J Vasc Interv Radiol. 2007; 18:1156–1161.
Article31. Breen DJ, Cowan NC. Fluoroscopically-guided retrieval of ureteric stents.Clin Radiol. 1995; 50:860–863.32. Yeung EY, Carmody E, Thurston W, Ho CS. Percutaneous fluoroscopically guided removal of dysfunctioning ureteral stents.Radiology. 1994; 190:145–148.33. Liang HL, Yang TL, Huang JS, Lin YH, Chou CP, Chen MC, et al. Antegrade retrieval of ureteral stents through an 8-French percutaneous nephrostomy route. AJR Am J Roentgenol. 2008; 191:1530–1535.
Article34. Park SW, Cha IH, Hong SJ, Yi JG, Jeon HJ, Park JH, et al. Fluoroscopy-guided transurethral removal and exchange of ureteral stents in female patients: technical notes. J Vasc Interv Radiol. 2007; 18:251–256.
Article35. McCarthy E, Kavanagh J, McKernan S, O'Mahony N, McEniff N, Ryan JM, et al. Fluoroscopically guided transurethral removal and/or replacement of ureteric stents in women. Acta Radiol. 2015; 56:635–640.
Article36. Pedro RN, Hendlin K, Kriedberg C, Monga M. Wire-based ureteral stents: impact on tensile strength and compression. Urology. 2007; 70:1057–1059.
Article37. Lugmayr HF, Pauer W. Wallstents for the treatment of extrinsic malignant ureteral obstruction: midterm results. Radiology. 1996; 198:105–108.
Article38. Flueckiger F, Lammer J, Klein GE, Hausegger K, Lederer A, Szolar D, et al. Malignant ureteral obstruction: preliminary results of treatment with metallic self-expandable stents.Radiology. 1993; 186:169–173.39. Chung KJ, Park BH, Park B, Lee JH, Kim WJ, Baek M, et al. Efficacy and safety of a novel, double-layered, coated, self-expandable metallic mesh stent (UventaTM) in malignant ureteral obstructions.J Endourol. 2013; 27:930–935.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous placement of ureteral stent
- Recent Advances in Gastrointestinal Stent Development
- Antegrade Ureteral Stenting in Ureteral Obstruction
- Adverse Effects of Ureteral Stent and Development of the Antireflux Ureteral Stent
- Removal of Migrated Thermo-Expandable Ureteral Stent (Memokath): Open Procedure 1 Case