Obstet Gynecol Sci.
2019 Sep;62(5):344-351. 10.5468/ogs.2019.62.5.344.
Scheduled injection of ramosetron for prevention of nausea and vomiting following single-port access total laparoscopic hysterectomy: a prospective randomized study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Yonsei University Wonju College of Medicine, Wonju, Korea. sanaram@yonsei.ac.kr
- 2Department of Obstetrics and Gynecology, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- KMID: 2456830
- DOI: http://doi.org/10.5468/ogs.2019.62.5.344
Abstract
OBJECTIVE
The purpose of this study was to evaluate the effectiveness of scheduled ramosetron injections for controlling postoperative nausea and vomiting (PONV) after single-port access total laparoscopic hysterectomy (SPA-TLH).
METHODS
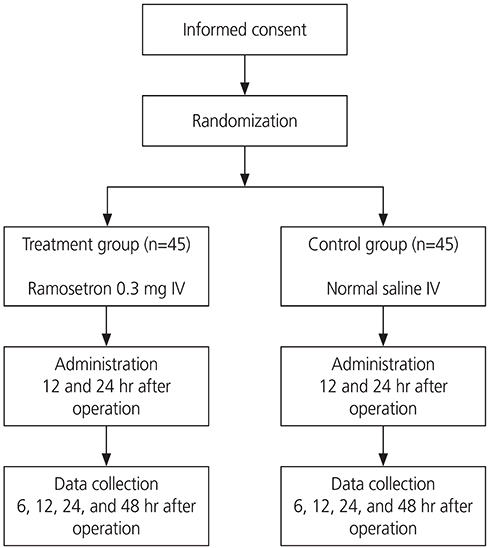
Ninety patients who underwent SPA-TLH at the Korean National Health Insurance Service Ilsan Hospital between June 2013 and July 2014 were enrolled in this prospective, randomized, double-blinded, placebo-controlled study. The patients were divided into 2 groups as follows: the ramosetron group (0.3 mg intravenously [IV]; n=45) and the placebo group (normal saline IV; n=45). Both groups received their respective injections 12 and 24 hours post surgery. The incidence and severity of PONV (numerical rating scale, 0-10), and the use of rescue antiemetics post surgery were evaluated.
RESULTS
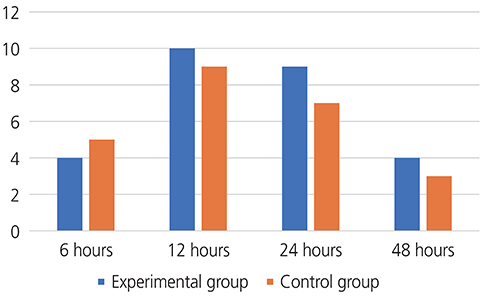
Demographic and perioperative statistically significant differences were not observed between the 2 groups. The incidence of PONV in the ramosetron and placebo groups was 46.7% and 51.1%, respectively (P=0.51). We found significant differences in the severity of PONV between the 24- to 48-hour postoperative periods in both groups (ramosetron group, P=0.04 and placebo group, P=0.03). The use of rescue antiemetics was significantly lower in the ramosetron group than in the placebo group (P=0.02).
CONCLUSION
After general anesthesia, scheduled injections of ramosetron 12 and 24 hours after SPA-TLH reduced the severity of PONV and the use of rescue antiemetics. Administration of ramosetron can be considered not only immediately after SPA-TLH but also during the first 24-hour recovery period. TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT 02011659
MeSH Terms
Figure
Reference
-
1. Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. 1999; 89:652–658.
Article2. Gan TJ, Meyer T, Apfel CC, Chung F, Davis PJ, Eubanks S, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003; 97:62–71.
Article3. Rowbotham D. Recognising risk factors. Nurs Times. 1995; 91:44–46.4. Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology. 2003; 98:46–52.
Article5. Jacobson TZ, Davis CJ. Safe laparoscopy: is it possible? Curr Opin Obstet Gynecol. 2004; 16:283–288.
Article6. Korolija D, Sauerland S, Wood-Dauphinée S, Abbou CC, Eypasch E, Caballero MG, et al. Evaluation of quality of life after laparoscopic surgery: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2004; 18:879–897.
Article7. Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, et al. Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc. 2010; 24:2248–2252.
Article8. Song T, Cho J, Kim TJ, Kim IR, Hahm TS, Kim BG, et al. Cosmetic outcomes of laparoendoscopic single-site hysterectomy compared with multi-port surgery: randomized controlled trial. J Minim Invasive Gynecol. 2013; 20:460–467.
Article9. Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992; 77:162–184.10. Fijihara A, Akuzawa S, Miyata K, Miyake A. Ramosetron hydrochloride: affinity for cloned human 5-HT3 receptor antagonistic and anti-emetic effect in ferret. Clin Rep. 1996; 30:1955–1964.11. Lee D, Kim JY, Shin JW, Ku CH, Park YS, Kwak HJ. The effect of oral and IV ramosetron on postoperative nausea and vomiting in patients undergoing gynecological laparoscopy with total intravenous anesthesia. J Anesth. 2009; 23:46–50.
Article12. Lee SY, Shin YS, Kim JH, Choi YH, Ko YK. Effect of timing of ramosetron administration on incidence of postoperative nausea and vomiting in patients undergoing laparoscopic gynecological surgery. Korean J Anesthesiol. 2009; 56:663–668.
Article13. Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010; 203:26.e1–26.e6.
Article14. Kim SH, Jin CH, Hwang IT, Park JS, Shin JH, Kim DW, et al. Postoperative outcomes of natural orifice transluminal endoscopic surgery-assisted vaginal hysterectomy and conventional laparoscopic-assisted vaginal hysterectomy: a comparative study. Obstet Gynecol Sci. 2018; 61:261–266.
Article15. Gan TJ. Postoperative nausea and vomiting--can it be eliminated? JAMA. 2002; 287:1233–1236.
Article16. Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999; 91:693–700.17. Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006; 102:1884–1898.
Article18. Ali SZ, Taguchi A, Holtmann B, Kurz A. Effect of supplemental pre-operative fluid on postoperative nausea and vomiting. Anaesthesia. 2003; 58:780–784.
Article19. Kim SI, Kim SC, Baek YH, Ok SY, Kim SH. Comparison of ramosetron with ondansetron for prevention of postoperative nausea and vomiting in patients undergoing gynaecological surgery. Br J Anaesth. 2009; 103:549–553.
Article20. Mihara T, Tojo K, Uchimoto K, Morita S, Goto T. Reevaluation of the effectiveness of ramosetron for preventing postoperative nausea and vomiting: a systematic review and meta-analysis. Anesth Analg. 2013; 117:329–339.21. Kim MS, Park JH, Choi YS, Park SH, Shin S. Efficacy of palonosetron vs. ramosetron for the prevention of postoperative nausea and vomiting: a meta-analysis of randomized controlled trials. Yonsei Med J. 2017; 58:848–858.
Article22. Tang J, Wang B, White PF, Watcha MF, Qi J, Wender RH. The effect of timing of ondansetron administration on its efficacy, cost-effectiveness, and cost-benefit as a prophylactic antiemetic in the ambulatory setting. Anesth Analg. 1998; 86:274–282.
Article23. Sun R, Klein KW, White PF. The effect of timing of ondansetron administration in outpatients undergoing otolaryngologic surgery. Anesth Analg. 1997; 84:331–336.
Article24. Cruz NI, Portilla P, Vela RE. Timing of ondansetron administration to prevent postoperative nausea and vomiting. P R Health Sci J. 2008; 27:43–47.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy and Safety of Ramosetron Injection for Nausea and Vomiting in Colorectal-Cancer Patients Undergoing a Laparoscopic Colectomy: A Randomized, Double-Blind, Comparative Study
- Single port transumbilical total laparoscopic hysterectomy (TLH): initial experience in Korea
- Techniques of gynecologic single-port access laparoscopic surgery
- Transumbilical single port total laparoscopic hysterectomy
- Efficacy of Ramosetron for the Prevention of Nausea and Vomiting after Thyroidectomy