Obstet Gynecol Sci.
2019 Sep;62(5):329-334. 10.5468/ogs.2019.62.5.329.
Polycystic ovarian morphology is associated with primary dysmenorrhea in young Korean women
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Severance Hospital, CHA University School of Medicine, Seoul, Korea. garfieldzz@yuhs.ac
- 2Institute of Women's Life Medical Science, CHA University School of Medicine, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 4Fertility Center of CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea.
- KMID: 2456828
- DOI: http://doi.org/10.5468/ogs.2019.62.5.329
Abstract
OBJECTIVE
This study was aimed at identifying a correlation between polycystic ovarian morphology (PCOM) and the severity of primary dysmenorrhea in young Korean women.
METHODS
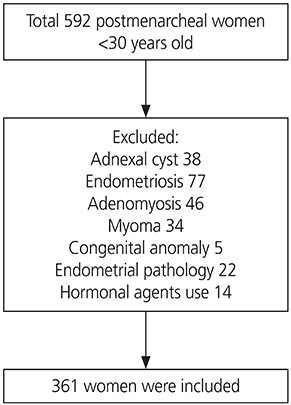
A total of 592 patients who visited a tertiary hospital from March 2008 to March 2015 for dysmenorrhea were examined. After excluding those with secondary causes of menstrual pain (for example, myoma, adenomyosis, endometriosis, and pelvic inflammatory disease), 361 women were recruited and retrospectively analyzed. Severe dysmenorrhea was defined as a visual analog scale (VAS) score ≥6.
RESULTS
The mean patient age was 23.0±4.0 years, the average menstrual cycle length was 34.4±23.7 days, and the average pain intensity was VAS 6.7±0.1 at baseline. PCOM was assessed by ultrasound in 54 women (15%). Patients with severe menstrual pain were more likely to have irregular menstrual cycles (P=0.03) and heavy menstrual flow (P=0.01) than those with mild menstrual pain. After adjusting for weight, height, menstrual cycle interval, and menstrual flow in the logistic regression analysis, PCOM (odds ratio [OR], 2.26; 95% confidence interval [CI], 1.05-4.97; P=0.04) and heavy menstrual flow (OR, 1.85; 95% CI, 1.05-3.28; P=0.04) were found to be significant independent factors influencing pain.
CONCLUSION
Our study shows that PCOM may have a correlation with the severity of primary dysmenorrhea. Since PCOM may play a role in the development of menstrual pain, patients with PCOM should be under active surveillance with resources for prompt pain management readily available. It may also be necessary to further investigate the molecular mechanisms of pain development in primary dysmenorrhea.
MeSH Terms
Figure
Reference
-
1. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015; 21:762–778.
Article2. Campbell MA, McGrath PJ. Use of medication by adolescents for the management of menstrual discomfort. Arch Pediatr Adolesc Med. 1997; 151:905–913.
Article3. Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004; 19:41–47.4. Polson DW, Adams J, Wadsworth J, Franks S. Polycystic ovaries--a common finding in normal women. Lancet. 1988; 1:870–872.
Article5. Rosenfield RL. The polycystic ovary morphology-polycystic ovary syndrome spectrum. J Pediatr Adolesc Gynecol. 2015; 28:412–419.
Article6. Youngster M, Ward VL, Blood EA, Barnewolt CE, Emans SJ, Divasta AD. Utility of ultrasound in the diagnosis of polycystic ovary syndrome in adolescents. Fertil Steril. 2014; 102:1432–1438.
Article7. Codner E, Villarroel C, Eyzaguirre FC, López P, Merino PM, Pérez-Bravo F, et al. Polycystic ovarian morphology in postmenarchal adolescents. Fertil Steril. 2011; 95:702–706.e1-2.
Article8. Dewailly D, Lujan ME, Carmina E, Cedars MI, Laven J, Norman RJ, et al. Definition and significance of polycystic ovarian morphology: a task force report from the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2014; 20:334–352.
Article9. Clayton RN, Ogden V, Hodgkinson J, Worswick L, Rodin DA, Dyer S, et al. How common are polycystic ovaries in normal women and what is their significance for the fertility of the population? Clin Endocrinol (Oxf). 1992; 37:127–134.
Article10. Fritz MA, Speroff L. Clinical gynecologic endocrinology and infertility. 8th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2011.11. Tomás-Rodríguez MI, Palazón-Bru A, Martínez-St John DR, Navarro-Cremades F, Toledo-Marhuenda JV, Gil-Guillén VF. Factors associated with increased pain in primary dysmenorrhea: analysis using a multivariate ordered logistic regression model. J Pediatr Adolesc Gynecol. 2017; 30:199–202.
Article12. Tena G, Moran C, Romero R, Moran S. Ovarian morphology and endocrine function in polycystic ovary syndrome. Arch Gynecol Obstet. 2011; 284:1443–1448.
Article13. Fukui Y, Taguchi A, Adachi K, Sato M, Kawata A, Tanikawa M, et al. Polycystic ovarian morphology may be a positive prognostic factor in patients with endometrial cancer who achieved complete remission after fertility-sparing therapy with progestin. Asian Pac J Cancer Prev. 2017; 18:3111–3116.14. Brincat M, Galea R, Buhagiar A. Polycystic ovaries and endometriosis: a possible connection. Br J Obstet Gynaecol. 1994; 101:346–348.
Article15. Creatsas G, Deligeoroglou E, Zachari A, Loutradis D, Papadimitriou T, Miras K, et al. Prostaglandins: PGF2 alpha, PGE2, 6-keto-PGF1 alpha and TXB2 serum levels in dysmenorrheic adolescents before, during and after treatment with oral contraceptives. Eur J Obstet Gynecol Reprod Biol. 1990; 36:292–298.16. Lee LC, Tu CH, Chen LF, Shen HD, Chao HT, Lin MW, et al. Association of brain-derived neurotrophic factor gene Val66Met polymorphism with primary dysmenorrhea. PLoS One. 2014; 9:e112766.
Article17. Akdemir N, Cinemre H, Bilir C, Akin O, Akdemir R. Increased serum asymmetric dimethylarginine levels in primary dysmenorrhea. Gynecol Obstet Invest. 2010; 69:153–156.
Article18. Bakshi N, Morris CR. The role of the arginine metabolome in pain: implications for sickle cell disease. J Pain Res. 2016; 9:167–175.19. Akdemir N, Cinemre FB, Bostancı MS, Cinemre H, Ünal O, Ozden S, et al. The correlation of serum asymmetric dimethylarginine and anti-Müllerian hormone in primary dysmenorrhea. Kaohsiung J Med Sci. 2016; 32:414–419.
Article20. Villarroel C, Merino PM, López P, Eyzaguirre FC, Van Velzen A, Iñiguez G, et al. Polycystic ovarian morphology in adolescents with regular menstrual cycles is associated with elevated anti-Mullerian hormone. Hum Reprod. 2011; 26:2861–2868.
Article21. López Bernal A, Buckley S, Rees CM, Marshall JM. Meclofenamate inhibits prostaglandin E binding and adenylyl cyclase activation in human myometrium. J Endocrinol. 1991; 129:439–445.22. Mäkäräinen L, Ylikorkala O. Primary and myoma-associated menorrhagia: role of prostaglandins and effects of ibuprofen. Br J Obstet Gynaecol. 1986; 93:974–978.23. Rees MC, DiMarzo V, Tippins JR, Morris HR, Turnbull AC. Leukotriene release by endometrium and myometrium throughout the menstrual cycle in dysmenorrhoea and menorrhagia. J Endocrinol. 1987; 113:291–295.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of combined oral contraceptives on polycystic ovarian morphology-related parameters in Korean women with polycystic ovary syndrome
- Differentiation between polycystic ovary syndrome and polycystic ovarian morphology by means of an anti-Müllerian hormone cutoff value
- Stellate Ganglion Block for the Treatment of Primary Dysmenorrhea
- Association between polycystic ovarian morphology and insulin resistance in women with polycystic ovary syndrome
- Clinical use of oral contraceptives