Ann Surg Treat Res.
2019 Aug;97(2):103-111. 10.4174/astr.2019.97.2.103.
Early versus late surgical management for complicated appendicitis in adults: a multicenter propensity score matching study
- Affiliations
-
- 1Department of Surgery, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwasung, Korea.
- 2Department of Surgery, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. snyoon@hallym.or.kr
- KMID: 2455984
- DOI: http://doi.org/10.4174/astr.2019.97.2.103
Abstract
- PURPOSE
Surgeons may be uncertain about the optimal timing of appendectomy to decrease complications, especially for complicated appendicitis. The aim of the study was to compare clinical outcomes between early and late surgery for complicated appendicitis.
METHODS
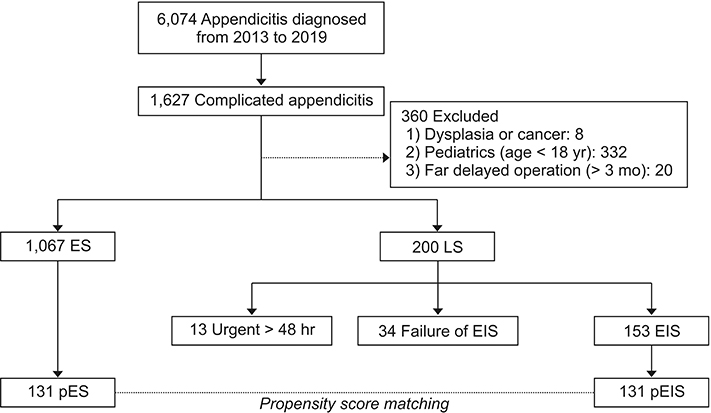
A prospectively maintained database of complicated appendicitis was queried. Elective interval surgery (EIS) group and early surgery (ES) were matched with propensity score and marked with a prefix "˜p.' Patient characteristics and surgical outcomes were compared.
RESULTS
The propensity score-matched EIS group had a lower chance to underwent ileo-cecectomy or right hemicolectomy (1.5% vs. 6.9%, P = 0.031), a tendency of lower rate of postoperative complication (6.9% vs. 13.7%, P = 0.067), a lower rate of wound infection (1.5% vs. 8.4%, P = 0.010), and shorter postoperative hospital stay (3.72 days vs. 5.82 days, P < 0.001) than the propensity score-matched ES group. Multivariate analysis showed that delayed surgery for more than 48 hours or urgent surgery due to failure of EIS and open conversion were independent risk factors for postoperative complications (P = 0.001 and P = 0.025, respectively). In subgroup analysis, high American Society of Anesthesiologists physical status classification and distant abscess or generalized ascites in initial CT increased the risk of failure of EIS.
CONCLUSION
EIS can be a useful option for selected adult patients with complicated appendicitis.
MeSH Terms
Figure
Reference
-
1. Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat 13. 1998; (139):1–119.2. Karp MP, Caldarola VA, Cooney DR, Allen JE, Jewett TC Jr. The avoidable excesses in the management of perforated appendicitis in children. J Pediatr Surg. 1986; 21:506–510.
Article3. Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007; 246:741–748.4. Ingraham AM, Cohen ME, Bilimoria KY, Ko CY, Hall BL, Russell TR, et al. Effect of delay to operation on outcomes in adults with acute appendicitis. Arch Surg. 2010; 145:886–892.
Article5. Kim M, Kim SJ, Cho HJ. Effect of surgical timing and outcomes for appendicitis severity. Ann Surg Treat Res. 2016; 91:85–89.
Article6. Friedell ML, Perez-Izquierdo M. Is there a role for interval appendectomy in the management of acute appendicitis? Am Surg. 2000; 66:1158–1162.7. Lai HW, Loong CC, Wu CW, Lui WY. Watchful waiting versus interval appendectomy for patients who recovered from acute appendicitis with tumor formation: a cost-effectiveness analysis. J Chin Med Assoc. 2005; 68:431–434.
Article8. Bufo AJ, Shah RS, Li MH, Cyr NA, Hollabaugh RS, Hixson SD, et al. Interval appendectomy for perforated appendicitis in children. J Laparoendosc Adv Surg Tech A. 1998; 8:209–214.
Article9. Blakely ML, Williams R, Dassinger MS, Eubanks JW 3rd, Fischer P, Huang EY, et al. Early vs interval appendectomy for children with perforated appendicitis. Arch Surg. 2011; 146:660–665.
Article10. Myers AL, Williams RF, Giles K, Waters TM, Eubanks JW 3rd, Hixson SD, et al. Hospital cost analysis of a prospective, randomized trial of early vs interval appendectomy for perforated appendicitis in children. J Am Coll Surg. 2012; 214:427–434.
Article11. St Peter SD, Aguayo P, Fraser JD, Keckler SJ, Sharp SW, Leys CM, et al. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010; 45:236–240.12. Bates DB, Fernandez MB, Ponchiardi C, von Plato M, Teich JP, Narsule C, et al. Surgical management in acute diverticulitis and its association with multi-detector CT, modified Hinchey classification, and clinical parameters. Abdom Radiol (NY). 2018; 43:2060–2065.
Article13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.14. Seal A. Appendicitis: a historical review. Can J Surg. 1981; 24:427–433.15. Blomqvist PG, Andersson RE, Granath F, Lambe MP, Ekbom AR. Mortality after appendectomy in Sweden, 1987-1996. Ann Surg. 2001; 233:455–460.
Article16. Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010; 34:2026–2040.
Article17. Yardeni D, Hirschl RB, Drongowski RA, Teitelbaum DH, Geiger JD, Coran AG. Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night? J Pediatr Surg. 2004; 39:464–469.
Article18. Surana R, Quinn F, Puri P. Is it necessary to perform appendicectomy in the middle of the night in children? BMJ. 1993; 306:1168.
Article19. Hansson J, Korner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009; 96:473–481.
Article20. Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006; 30:1033–1037.
Article21. Willemsen PJ, Hoorntje LE, Eddes EH, Ploeg RJ. The need for interval appendectomy after resolution of an appendiceal mass questioned. Dig Surg. 2002; 19:216–220.
Article22. Puapong D, Lee SL, Haigh PI, Kaminski A, Liu IL, Applebaum H. Routine interval appendectomy in children is not indicated. J Pediatr Surg. 2007; 42:1500–1503.
Article23. Quartey B. Interval appendectomy in adults: a necessary evil? J Emerg Trauma Shock. 2012; 5:213–216.
Article24. Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH. Is there truly an oncologic indication for interval appendectomy? Am J Surg. 2015; 209:442–446.
Article25. Chen CC, Ting CT, Tsai MJ, Hsu WC, Chen PC, Lee MD, et al. Appendectomy timing: Will delayed surgery increase the complications? J Chin Med Assoc. 2015; 78:395–399.
Article26. United Kingdom National Surgical Research Collaborative. Bhangu A. Safety of short, in-hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta-analysis. Ann Surg. 2014; 259:894–903.27. Saluja S, Sun T, Mao J, Steigman SA, Oh PS, Yeo HL, et al. Early versus late surgical management of complicated appendicitis in children: a statewide database analysis with one-year follow-up. J Pediatr Surg. 2018; 53:1339–1344.
Article28. Krajewski S, Brown J, Phang PT, Raval M, Brown CJ. Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg. 2011; 54:43–53.
Article29. Hashizume N, Iinuma Y, Hirayama Y, Nitta K, Iida H, Shiotani M, et al. Contrast-enhanced multidetector-row computed tomography can predict pathological findings of acute appendicitis in children. Acute Med Surg. 2015; 3:21–25.
Article30. Kim HC, Yang DM, Lee CM, Jin W, Nam DH, Song JY, et al. Acute appendicitis: relationships between CT-determined severities and serum white blood cell counts and C-reactive protein levels. Br J Radiol. 2011; 84:1115–1120.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety of appendectomy during pregnancy in the totally laparoscopic age
- Applications of propensity score matching: a case series of articles published in Annals of Coloproctology
- Diagnostic Efficacy of the Alvarado Score according to Age in Acute Appendicitis
- Optimal drain management following complicated laparoscopic cholecystectomy for acute cholecystitis: a propensity-matched comparative study
- Impact of the Endoscopic Submucosal Dissection on Early Postoperative Outcome after Additional Gastric Resections for Early Gastric Cancer