Ann Surg Treat Res.
2019 Sep;97(3):113-118. 10.4174/astr.2019.97.3.113.
Trends in contralateral prophylactic mastectomy rate according to clinicopathologic and socioeconomic status
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. imgenius2@gmail.com
- 2Hereditary Cancer Clinic of Cancer Prevention Center, Yonsei Cancer Center, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Cancer Prevention Center, Yonsei Cancer Center, Seoul, Korea.
- 4Institute of Women's Life Medical Science, Women's Cancer Clinic, Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 6Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2455970
- DOI: http://doi.org/10.4174/astr.2019.97.3.113
Abstract
- PURPOSE
There has been an increasing trend in the use of contralateral prophylactic mastectomy (CPM) among women diagnosed with unilateral breast cancer or mutations in BRCA1 or BRCA2 to reduce the occurrence of contralateral breast cancer. This study aimed to examine trends in the CPM rate according to clinicopathologic and socioeconomic status at a single institution in Korea.
METHODS
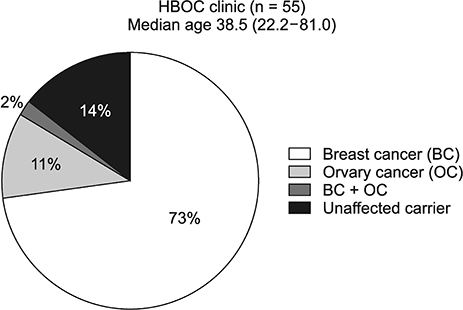
This study included 128 patients with mutations in BRCA1 or BRCA2. Patients were divided into a CPM group (n = 8) and a non-CPM group (n = 120) between May 2013 and March 2016. The main outcome variables, including epidemiology, clinical features, socioeconomic status, and tumor characteristics, were analyzed.
RESULTS
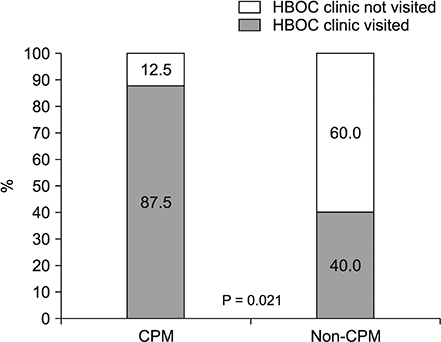
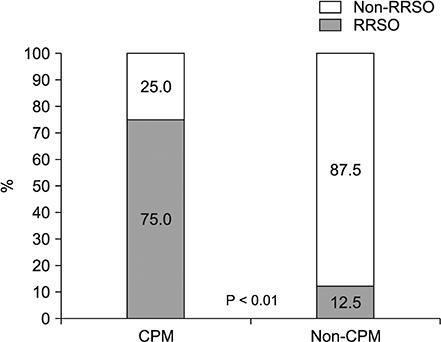
A total of 8 CPMs were performed among 128 patients. All CPM patients were married. The proportion of professional working women was higher in the CPM group (P = 0.049). Most patients who underwent CPM graduated college, compared to less than a third of the non-CPM group (P = 0.013). The CPM group had a higher rate of visits to the Hereditary Breast and Ovarian Cancer (HBOC) clinic (P = 0.021). The risk-reducing salpingo-oophorectomy (RRSO) rate was significantly higher in the CPM group (P < 0.01).
CONCLUSION
CPM rates were significantly different according to socioeconomic status. The CPM rate tends to increase in highly educated and professional working women. The socioeconomic status of patients is an important factor in the decision to participate in the HBOC clinic and undergo CPM or RRSO.
Keyword
MeSH Terms
Figure
Reference
-
1. Baptiste DF, MacGeorge EL, Venetis MK, Mouton A, Friley LB, Pastor R, et al. Motivations for contralateral prophylactic mastectomy as a function of socioeconomic status. BMC Womens Health. 2017; 17:10.
Article2. Morrow W. Prophylactic mastectomy of the contralateral breast. Breast. 2011; 20 Suppl 3:S108–S110.
Article3. Evans DG, Wisely J, Clancy T, Lalloo F, Wilson M, Johnson R, et al. Longer term effects of the Angelina Jolie effect: increased risk-reducing mastectomy rates in BRCA carriers and other high-risk women. Breast Cancer Res. 2015; 17:143.
Article4. Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003; 72:1117–1130.
Article5. Han SA, Park SK, Ahn SH, Son BH, Lee MH, Choi DH, et al. The breast and ovarian cancer risks in Korea due to inherited mutations in BRCA1 and BRCA2: a preliminary report. J Breast Cancer. 2009; 12:92–99.
Article6. Han SA, Kim SW, Kang E, Park SK, Ahn SH, Lee MH, et al. The prevalence of BRCA mutations among familial breast cancer patients in Korea: results of the Korean Hereditary Breast Cancer study. Fam Cancer. 2013; 12:75–81.7. Son BH, Ahn SH, Kim SW, Kang E, Park SK, Lee MH, et al. Prevalence of BRCA1 and BRCA2 mutations in non-familial breast cancer patients with high risks in Korea: the Korean Hereditary Breast Cancer (KOHBRA) Study. Breast Cancer Res Treat. 2012; 133:1143–1152.
Article8. Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Myers JL, Arnold PG. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999; 340:77–84.
Article9. Meijers-Heijboer H, van Geel B, van Putten WL, Henzen-Logmans SC, Seynaeve C, Menke-Pluymers MB, et al. Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2001; 345:159–164.10. Boughey JC, Hoskin TL, Degnim AC, Sellers TA, Johnson JL, Kasner MJ, et al. Contralateral prophylactic mastectomy is associated with a survival advantage in high-risk women with a personal history of breast cancer. Ann Surg Oncol. 2010; 17:2702–2709.
Article11. Grimmer L, Liederbach E, Velasco J, Pesce C, Wang CH, Yao K. Variation in contralateral prophylactic mastectomy rates according to racial groups in young women with breast cancer, 1998 to 2011: a report from the National Cancer Data Base. J Am Coll Surg. 2015; 221:187–196.
Article12. Khan SA. Contralateral prophylactic mastectomy: what do we know and what do our patients know? J Clin Oncol. 2011; 29:2132–2135.
Article13. Rendle KA, Halley MC, May SG, Frosch DL. Redefining risk and benefit: understanding the decision to undergo contralateral prophylactic mastectomy. Qual Health Res. 2015; 25:1251–1259.14. Rosenberg SM, Tracy MS, Meyer ME, Sepucha K, Gelber S, Hirshfield-Bartek J, et al. Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Ann Intern Med. 2013; 159:373–381.15. Yi M, Hunt KK, Arun BK, Bedrosian I, Barrera AG, Do KA, et al. Factors affecting the decision of breast cancer patients to undergo contralateral prophylactic mastectomy. Cancer Prev Res (Phila). 2010; 3:1026–1034.
Article16. Yakoub D, Avisar E, Koru-Sengul T, Miao F, Tannenbaum SL, Byrne MM, et al. Factors associated with contralateral preventive mastectomy. Breast Cancer (Dove Med Press). 2015; 7:1–8.
Article17. Yao K, Stewart AK, Winchester DJ, Winchester DP. Trends in contralateral prophylactic mastectomy for unilateral cancer: a report from the National Cancer Data Base, 1998–2007. Ann Surg Oncol. 2010; 17:2554–2562.
Article18. Education & socioeconomic status [Internet]. Washington, DC: American Psychological Association;2012. cited 2018 Aug 19. Available from: https://www.apa.org/pi/ses/resources/publications/factsheet-education.pdf.19. Disability & socioeconomic status [Internet]. Washington, DC: American Psychological Association;2017. cited 2018 Aug 19. Available from: https://www.apa.org/pi/ses/resources/publications/factsheet-disability.pdf.20. van Sprundel TC, Schmidt MK, Rookus MA, Brohet R, van Asperen CJ, Rutgers EJ, et al. Risk reduction of contralateral breast cancer and survival after contralateral prophylactic mastectomy in BRCA1 or BRCA2 mutation carriers. Br J Cancer. 2005; 93:287–292.
Article21. Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer. Ann Surg. 2017; 265:581–589.
Article22. Alaofi RK, Nassif MO, Al-Hajeili MR. Prophylactic mastectomy for the prevention of breast cancer: review of the literature. Avicenna J Med. 2018; 8:67–77.
Article23. Frost MH, Hoskin TL, Hartmann LC, Degnim AC, Johnson JL, Boughey JC. Contralateral prophylactic mastectomy: long-term consistency of satisfaction and adverse effects and the significance of informed decision-making, quality of life, and personality traits. Ann Surg Oncol. 2011; 18:3110–3116.
Article24. Ward EP, Unkart JT, Bryant A, Murphy J, Blair SL. Influence of distance to hospital and insurance status on the rates of contralateral prophylactic mastectomy, a National Cancer Data Base study. Ann Surg Oncol. 2017; 24:3038–3047.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perceptions of Prophylactic Mastectomy in Korea
- Association Between Socioeconomic Status and All-Cause Mortality After Breast Cancer Surgery: Nationwide Retrospective Cohort Study
- Socioeconomic inequalities in health status in Korea
- Experience with Bilateral Risk-Reducing Mastectomy for an Unaffected BRCA Mutation Carrier
- Interference of Detection Rate of Lumbar Disc Herniation by Socioeconomic Status