Korean Circ J.
2019 Sep;49(9):818-828. 10.4070/kcj.2019.0245.
Clinical Significance and Therapeutic Implication of Nocturnal Hypertension: Relationship between Nighttime Blood Pressure and Quality of Sleep
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Chungbuk National University, Cheongju, Korea. mccho@cbnu.ac.kr
- KMID: 2455787
- DOI: http://doi.org/10.4070/kcj.2019.0245
Abstract
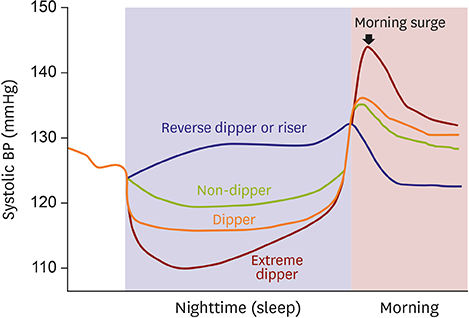
- Recent global hypertension guidelines recommend an early, strict and 24-hour blood pressure (BP) control for the prevention of target organ damage and cardiovascular events. Out-of-office BP measurement such as ambulatory BP monitoring and home BP monitoring is now widely utilized to rule out white-coat hypertension, to detect masked hypertension, to evaluate the effects of antihypertensive medication, to analyze diurnal BP variation, and to increase drug adherence. Nocturnal hypertension has been neglected in the management of hypertension despite of its clinical significance. Nighttime BP and non-dipping patterns of BP are stronger risk predictors for the future cardiovascular mortality and morbidity than clinic or daytime BP. In addition to ambulatory or home daytime BP and 24-hour mean BP, nocturnal BP should be a new therapeutic target for the optimal treatment of hypertension to improve prognosis in hypertensive patients. This review will provide an overview of epidemiology, characteristics, and pathophysiology of nocturnal hypertension and clinical significance, therapeutic implication and future perspectives of nocturnal hypertension will be discussed.
MeSH Terms
Figure
Reference
-
1. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016; 134:441–450.2. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006; 367:1747–1757.
Article3. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018; 138:e484–594.4. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104.5. Korean Society Hypertension (KSH). Hypertension Epidemiology Research Working Group. Kim HC, Cho MC. Korea hypertension fact sheet 2018. Clin Hypertens. 2018; 24:13.
Article6. Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. 2013; 61:278–283.7. Asayama K, Fujiwara T, Hoshide S, et al. Nocturnal blood pressure measured by home devices: evidence and perspective for clinical application. J Hypertens. 2019; 37:905–916.8. Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011; 57:3–10.
Article9. Fan HQ, Li Y, Thijs L, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010; 28:2036–2045.
Article10. Head GA. The importance and prognostic value of nocturnal blood pressure assessments using inexpensive domestic devices. J Hypertens. 2017; 35:463–465.
Article11. Kario K. Nocturnal hypertension: new technology and evidence. Hypertension. 2018; 71:997–1009.12. Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008; 51:55–61.
Article13. Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007; 49:1235–1241.14. ABC-H Investigators, Roush GC, Fagard RH, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014; 32:2332–2340.
Article15. Yano Y, Kario K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertens Res. 2012; 35:695–701.
Article16. O'Brien E, Sheridan J, O'Malley K. Dippers and non-dippers. Lancet. 1988; 2:397.17. Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001; 38:852–857.
Article18. Boggia J, Thijs L, Hansen TW, et al. Ambulatory blood pressure monitoring in 9357 subjects from 11 populations highlights missed opportunities for cardiovascular prevention in women. Hypertension. 2011; 57:397–405.
Article19. Ohkubo T, Hozawa A, Yamaguchi J, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002; 20:2183–2189.20. Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007; 370:1219–1229.
Article21. Lee HY, Shin J, Kim GH, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019; 25:20.
Article22. Li Y, Staessen JA, Lu L, Li LH, Wang GL, Wang JG. Is isolated nocturnal hypertension a novel clinical entity? Findings from a Chinese population study. Hypertension. 2007; 50:333–339.23. Thomas SJ, Booth JN 3rd, Bromfield SG, et al. Clinic and ambulatory blood pressure in a population-based sample of African Americans: the Jackson Heart Study. J Am Soc Hypertens. 2017; 11:204–212.e5.
Article24. Melgarejo JD, Maestre GE, Thijs L, et al. Prevalence, treatment, and control rates of conventional and ambulatory hypertension across 10 populations in 3 continents. Hypertension. 2017; 70:50–58.
Article25. Sakhuja S, Booth JN 3rd, Lloyd-Jones DM, et al. Health behaviors, nocturnal hypertension, and non-dipping blood pressure: the coronary artery risk development in young adults and Jackson Heart Study. Am J Hypertens. 2019; 32:759–768.
Article26. de la Sierra A, Gorostidi M, Banegas JR, Segura J, de la Cruz JJ, Ruilope LM. Nocturnal hypertension or nondipping: which is better associated with the cardiovascular risk profile? Am J Hypertens. 2014; 27:680–687.
Article27. Hoshide S, Kario K, de la Sierra A, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study. Hypertension. 2015; 66:750–756.28. Hosohata K, Kikuya M, Ohkubo T, et al. Reproducibility of nocturnal blood pressure assessed by self-measurement of blood pressure at home. Hypertens Res. 2007; 30:707–712.
Article29. Ushio H, Ishigami T, Araki N, et al. Utility and feasibility of a new programmable home blood pressure monitoring device for the assessment of nighttime blood pressure. Clin Exp Nephrol. 2009; 13:480–485.
Article30. Ishikawa J, Hoshide S, Eguchi K, et al. Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension. 2012; 60:921–928.
Article31. Kario K, Tomitani N, Kanegae H, et al. Comparative effects of an angiotensin II receptor blocker (ARB)/diuretic vs. ARB/calcium-channel blocker combination on uncontrolled nocturnal hypertension evaluated by information and communication technology-based nocturnal home blood pressure monitoring- the NOCTURNE study. Circ J. 2017; 81:948–957.32. Andreadis EA, Agaliotis G, Kollias A, Kolyvas G, Achimastos A, Stergiou GS. Night-time home versus ambulatory blood pressure in determining target organ damage. J Hypertens. 2016; 34:438–444.
Article33. Lindroos AS, Johansson JK, Puukka PJ, et al. The association between home vs. ambulatory night-time blood pressure and end-organ damage in the general population. J Hypertens. 2016; 34:1730–1737.
Article34. Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens (Greenwich). 2019; 21:853–858.
Article35. Kollias A, Ntineri A, Stergiou GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis. J Hypertens. 2017; 35:442–452.36. Carek AM, Conant J, Joshi A, Kang H, Inan OT. SeismoWatch: wearable cuffless blood pressure monitoring using pulse transit time. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2017; 1:40.37. Chen A. Samsung's Galaxy Watch is supposed to measure blood pressure? But how accurate will it be? [Internet]. New York (NY): Vox Media;2019. cited 2019 Aug 2. Available from: https://www.theverge.com/2019/2/25/18236373/samsung-galaxy-watch-blood-pressure-monitoring-health-fda.38. Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997; 96:1859–1862.
Article39. Kimura G. Kidney and circadian blood pressure rhythm. Hypertension. 2008; 51:827–828.
Article40. Kario K. Systemic hemodynamic atherothrombotic syndrome and resonance hypothesis of blood pressure variability: triggering cardiovascular events. Korean Circ J. 2016; 46:456–467.
Article41. Wang C, Zhang J, Liu X, et al. Reversed dipper blood-pressure pattern is closely related to severe renal and cardiovascular damage in patients with chronic kidney disease. PLoS One. 2013; 8:e55419.
Article42. Liu M, Takahashi H, Morita Y, et al. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol Dial Transplant. 2003; 18:563–569.
Article43. Legramante JM, Galante A. Sleep and hypertension: a challenge for the autonomic regulation of the cardiovascular system. Circulation. 2005; 112:786–788.44. Lombardi F, Parati G. An update on: cardiovascular and respiratory changes during sleep in normal and hypertensive subjects. Cardiovasc Res. 2000; 45:200–211.
Article45. Pepin JL, Borel AL, Tamisier R, Baguet JP, Levy P, Dauvilliers Y. Hypertension and sleep: overview of a tight relationship. Sleep Med Rev. 2014; 18:509–519.
Article46. Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012; 307:2169–2176.
Article47. Baguet JP, Hammer L, Lévy P, et al. Night-time and diastolic hypertension are common and underestimated conditions in newly diagnosed apnoeic patients. J Hypertens. 2005; 23:521–527.
Article48. Haentjens P, Van Meerhaeghe A, Moscariello A, et al. The impact of continuous positive airway pressure on blood pressure in patients with obstructive sleep apnea syndrome: evidence from a meta-analysis of placebo-controlled randomized trials. Arch Intern Med. 2007; 167:757–764.49. Turnbull F. Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003; 362:1527–1535.50. Hoshide S, Ishikawa J, Eguchi K, Ojima T, Shimada K, Kario K. Masked nocturnal hypertension and target organ damage in hypertensives with well-controlled self-measured home blood pressure. Hypertens Res. 2007; 30:143–149.
Article51. Komori T, Eguchi K, Tomizawa H, et al. Factors associated with incident ischemic stroke in hospitalized heart failure patients: a pilot study. Hypertens Res. 2008; 31:289–294.
Article52. Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005; 111:1777–1783.
Article53. Salvetti M, Muiesan ML, Rizzoni D, et al. Night time blood pressure and cardiovascular structure in a middle-aged general population in northern Italy: the Vobarno Study. J Hum Hypertens. 2001; 15:879–885.
Article54. Shin J, Xu E, Lim YH, et al. Relationship between nocturnal blood pressure and 24-h urinary sodium excretion in a rural population in Korea. Clin Hypertens. 2014; 20:9.
Article55. Lim YH, Enkhdorj R, Kim BK, Kim SG, Kim JH, Shin J. Correlation between proximal abdominal aortic stiffness measured by ultrasound and brachial-ankle pulse wave velocity. Korean Circ J. 2013; 43:391–399.
Article56. Kario K. Essential manual of 24-hour blood pressure management from morning to nocturnal hypertension. London: Wiley-Blackwell;2015.57. Heart Outcomes Prevention Evaluation Study Investigators. Yusuf S, Sleight P, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000; 342:145–153.
Article58. Svensson P, de Faire U, Sleight P, Yusuf S, Ostergren J. Comparative effects of ramipril on ambulatory and office blood pressures: a HOPE Substudy. Hypertension. 2001; 38:E28–32.
Article59. Hermida RC, Ayala DE. Chronotherapy with the angiotensin-converting enzyme inhibitor ramipril in essential hypertension: improved blood pressure control with bedtime dosing. Hypertension. 2009; 54:40–46.60. Pareek AK, Messerli FH, Chandurkar NB, et al. Efficacy of low-dose chlorthalidone and hydrochlorothiazide as assessed by 24-h ambulatory blood pressure monitoring. J Am Coll Cardiol. 2016; 67:379–389.61. Kario K. Proposal of a new strategy for ambulatory blood pressure profile-based management of resistant hypertension in the era of renal denervation. Hypertens Res. 2013; 36:478–484.
Article62. Imaizumi Y, Eguchi K, Murakami T, Arakawa K, Tsuchihashi T, Kario K. High salt intake is independently associated with hypertensive target organ damage. J Clin Hypertens (Greenwich). 2016; 18:315–321.
Article63. Yasuda G, Hasegawa K, Kuji T, et al. Effects of doxazosin on ambulatory blood pressure and sympathetic nervous activity in hypertensive Type 2 diabetic patients with overt nephropathy. Diabet Med. 2005; 22:1394–1400.
Article64. Bisognano JD, Bakris G, Nadim MK, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled Rheos Pivotal Trial. J Am Coll Cardiol. 2011; 58:765–773.65. Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009; 373:1275–1281.
Article66. Kario K, Bhatt DL, Kandzari DE, et al. Impact of renal denervation on patients with obstructive sleep apnea and resistant hypertension: insights from the SYMPLICITY HTN-3 trial. Circ J. 2016; 80:1404–1412.67. Hermida RC, Hermida RC. Ambulatory blood pressure monitoring in the prediction of cardiovascular events and effects of chronotherapy: rationale and design of the MAPEC study. Chronobiol Int. 2007; 24:749–775.
Article68. Mahabala C, Kamath P, Bhaskaran U, Pai ND, Pai AU. Antihypertensive therapy: nocturnal dippers and nondippers. Do we treat them differently? Vasc Health Risk Manag. 2013; 9:125–133.
Article69. Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010; 27:1629–1651.
Article70. Gorostidi M. Effect of Olmesartan-based therapy on therapeutic indicators obtain through out-of-office blood pressure. Cardiol Ther. 2015; 4:19–30.71. Hermida RC, Ayala DE, Fernández JR, Calvo C. Comparison of the efficacy of morning versus evening administration of telmisartan in essential hypertension. Hypertension. 2007; 50:715–722.
Article72. Tofé Povedano S, García De La Villa B. 24-Hour and night time blood pressures in type 2 diabetic hypertensive patients following morning or evening administration of Olmesartan. J Clin Hypertens (Greenwich). 2009; 11:426–431.73. Matsui Y, Eguchi K, O'Rourke MF, et al. Differential effects between a calcium channel blocker and a diuretic when used in combination with angiotensin II receptor blocker on central aortic pressure in hypertensive patients. Hypertension. 2009; 54:716–723.
Article74. Hermida RC, Ayala DE, Fernández JR, Calvo C. Chronotherapy improves blood pressure control and reverts the nondipper pattern in patients with resistant hypertension. Hypertension. 2008; 51:69–76.
Article75. Kario K, Okada K, Kato M, et al. 24-hour blood pressure-lowering effect of an SGLT-2 inhibitor in patients with diabetes and uncontrolled nocturnal hypertension: results from the randomized, placebo-controlled SACRA Study. Circulation. 2018; 139:2089–2097.76. American Diabetes Association. 8. Cardiovascular disease and risk management. Diabetes Care. 2016; 39:Suppl 1. S60–S71.77. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of Medical Care in Diabetes-2019. Diabetes Care. 2019; 42:S103–S123.78. McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371:993–1004.
Article79. Bavishi C, Messerli FH, Kadosh B, Ruilope LM, Kario K. Role of neprilysin inhibitor combinations in hypertension: insights from hypertension and heart failure trials. Eur Heart J. 2015; 36:1967–1973.
Article80. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med. 2015; 373:2117–2128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study of 24 Hour Ambulatory Blood Pressure Monitoring in Acute Stroke Patients
- Clinical Significance of Nighttime Blood Pressure
- Nocturnal dip in patients with cerebrovascular disease occurring during sleep: prospective assessment by using Ambulatory Blood Pressure Monitoring
- The Role of Endothelin-1 in Obstructive Sleep Apnea Syndrome and Pulmonary Hypertension
- Clinical and life style factors related to the nighttime blood pressure, nighttime dipping and their phenotypes in Korean hypertensive patients