Clin Endosc.
2019 Jul;52(4):382-386. 10.5946/ce.2018.198.
A Case of Concurrent Ampullary Adenoma and Gangliocytic Paraganglioma at the Minor Papilla Treated with Endoscopic Resection
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dhpark@amc.seoul.kr
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2455638
- DOI: http://doi.org/10.5946/ce.2018.198
Abstract
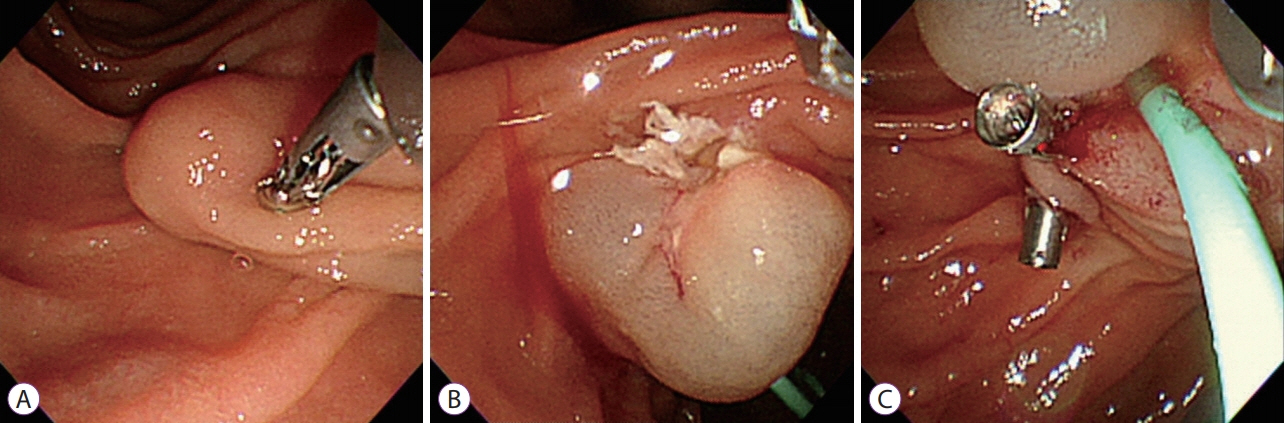
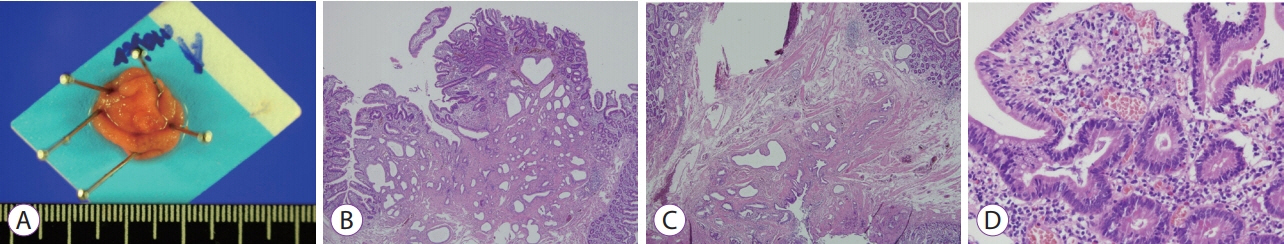
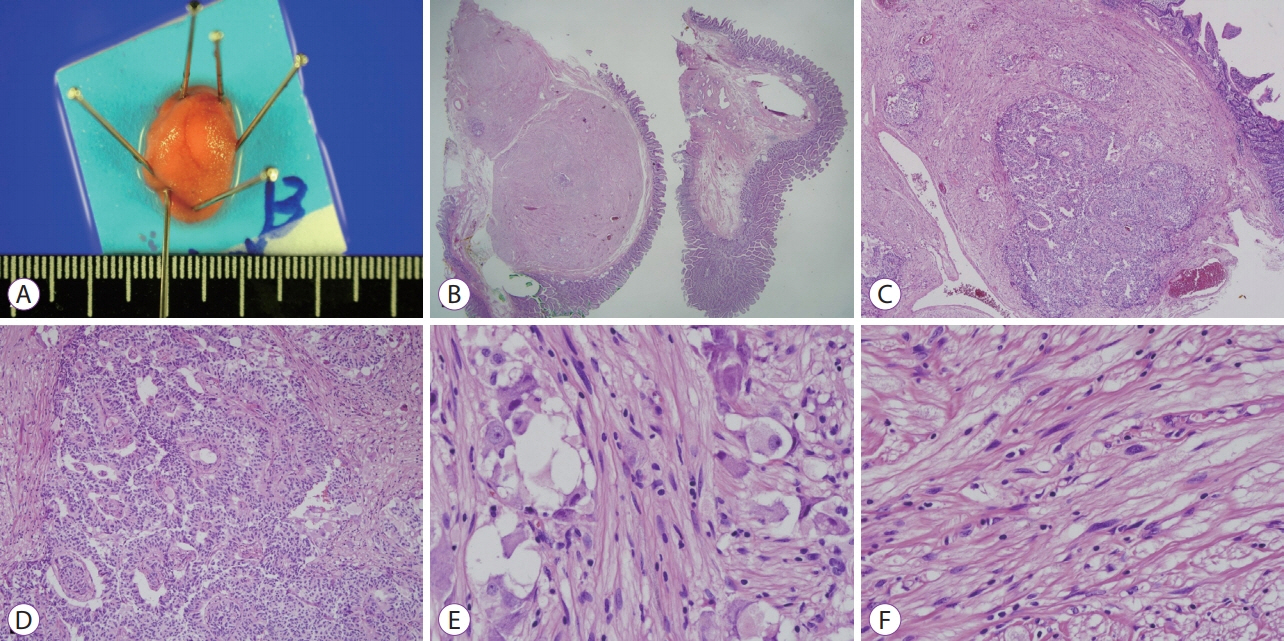
- A gangliocytic paraganglioma is a benign tumor of the digestive system with a very low incidence. The tumor is histopathologically characterized by a triphasic pattern consisting of epithelioid, ganglion, and spindle-shaped Schwann cells. In most cases, it occurs in the second portion of the duodenum near the ampulla of Vater. We report a case of a gangliocytic paraganglioma occurring at the minor duodenal papilla (a rare location) with a concurrent adenoma of the ampulla of Vater. Both lesions were treated simultaneously using endoscopic resection. Additionally, we have presented a literature review.
MeSH Terms
Figure
Reference
-
1. Burke AP, Helwig EB. Gangliocytic paraganglioma. Am J Clin Pathol. 1989; 92:1–9.
Article2. Okubo Y, Wakayama M, Nemoto T, et al. Literature survey on epidemiology and pathology of gangliocytic paraganglioma. BMC Cancer. 2011; 11:187.
Article3. Mann CM, Bramhall SR, Buckels JA, Taniere P. An unusual case of duodenal obstruction-gangliocytic paraganglioma. J Hepatobiliary Pancreat Surg. 2009; 16:562–565.
Article4. Park SJ, Kim DH, Lim H, et al. Endoscopic resection as a possible radical treatment for duodenal gangliocytic paraganglioma: a report of four cases. Korean J Gastroenterol. 2014; 63:114–119.
Article5. Reed RJ, Caroca PJ Jr, Harkin JC. Gangliocytic paraganglioma. Am J Surg Pathol. 1977; 1:207–216.
Article6. Perrone T, Sibley RK, Rosai J. Duodenal gangliocytic paraganglioma. An immunohistochemical and ultrastructural study and a hypothesis concerning its origin. Am J Surg Pathol. 1985; 9:31–41.7. Matsubayashi H, Ishiwatari H, Matsui T, et al. Gangliocytic paraganglioma of the minor papilla of the duodenum. Intern Med. 2017; 56:1029–1035.
Article8. Choi YH, Park DH, Kim SJ, et al. Two cases of endoscopic resection of submucosal tumor of the minor papilla. Korean J Gastrointest Endosc. 2007; 34:164–169.9. Loew BJ, Lukens FJ, Navarro F, Roy M, Mattia A, Howell DA. Successful endoscopic resection of a gangliocytic paraganglioma of the minor papilla in a patient with pancreas divisum and pancreatitis (with video). Gastrointest Endosc. 2007; 65:547–550.10. Nakamura T, Ozawa T, Kitagawa M, et al. Endoscopic resection of gangliocytic paraganglioma of the minor duodenal papilla: case report and review. Gastrointest Endosc. 2002; 55:270–273.
Article11. Witkiewicz A, Galler A, Yeo CJ, Gross SD. Gangliocytic paraganglioma: case report and review of the literature. J Gastrointest Surg. 2007; 11:1351–1354.
Article12. Bucher P, Mathe Z, Buhler L, et al. Paraganglioma of the ampulla of Vater: a potentially malignant neoplasm. Scand J Gastroenterol. 2004; 39:291–295.
Article13. Romano G, Agrusa A, Galia M, et al. Whipple’s pancreaticoduodenectomy: surgical technique and perioperative clinical outcomes in a single center. Int J Surg. 2015; 21 Suppl 1:S68–S71.
Article14. Barret M, Rahmi G, Duong van Huyen JP, Landi B, Cellier C, Berger A. Duodenal gangliocytic paraganglioma with lymph node metastasis and an 8-year follow-up: a case report. Eur J Gastroenterol Hepatol. 2012; 24:90–94.15. Culver EL, McIntyre AS. Sporadic duodenal polyps: classification, investigation, and management. Endoscopy. 2011; 43:144–155.
Article16. Sakamoto H, Kitano M, Kudo M. Diagnosis of subepithelial tumors in the upper gastrointestinal tract by endoscopic ultrasonography. World J Radiol. 2010; 2:289–297.
Article17. Kim JH. The diagnosis of subepithelial lesions in the upper gastrointestinal tract. Korean J Helicobacter Up Gastrointest Res. 2011; 11:71–74.
Article18. Smithline AE, Hawes RH, Kopecky KK, Cummings OW, Kumar S. Gangliocytic paraganglioma, a rare cause of upper gastrointestinal bleeding. Endoscopic ultrasound findings presented. Dig Dis Sci. 1993; 38:173–177.19. Hu W, Gao S, Chen D, et al. Duodenal gangliocytic paraganglioma with lymph node metastases: a case report and review of literature. Int J Clin Exp Pathol. 2016; 9:4756–4760.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Periampullary Gangliocytic Paraganglioma Successfully Treated by Endoscopic Mucosal Resection
- A case of juxtapapillary gangliocytic paraganglioma treated with endoscopic resection
- A Gangliocytic Paraganglioma Presenting as a Submucosal Tumor in the Ampulla
- Two Cases of Endoscopic Resection of Submucosal Tumor of the Minor Papilla
- Pancreatic and Biliary Strictures Associated with Cholangitis and Bile Reflux Following Endoscopic Papillectomy of Ampullary Adenoma