J Korean Orthop Assoc.
2019 Aug;54(4):353-360. 10.4055/jkoa.2019.54.4.353.
Clinical Results of Subtotal Fasciectomy for Treatment of Dupuytren Contracture
- Affiliations
-
- 1Department of Orthopedic Surgery, The Catholic University of Korea, Yeouido St. Mary's Hospital, Seoul, Korea. simba0415@catholic.ac.kr
- KMID: 2455504
- DOI: http://doi.org/10.4055/jkoa.2019.54.4.353
Abstract
- PURPOSE
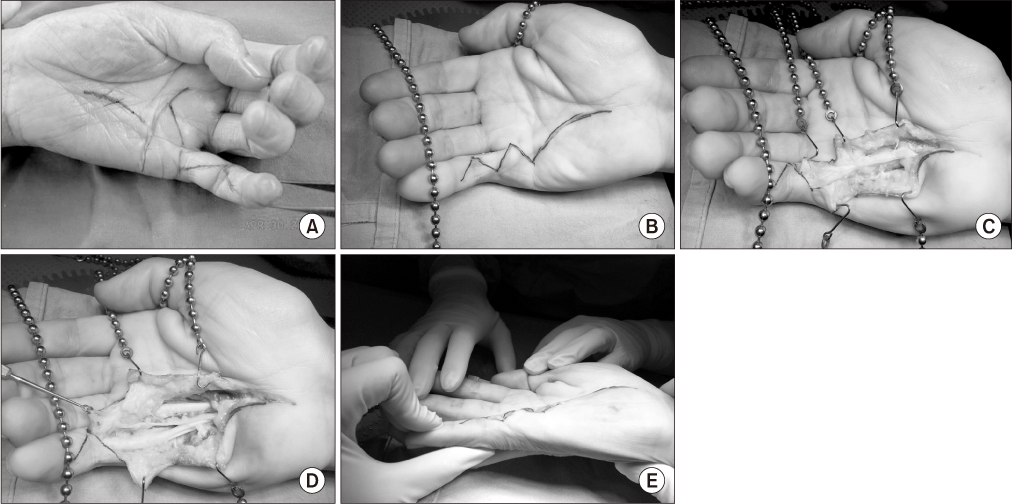
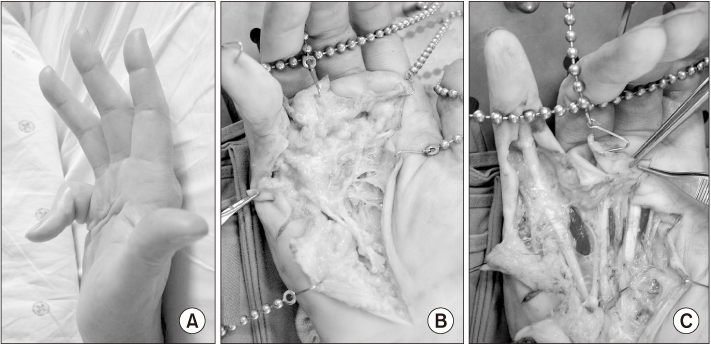
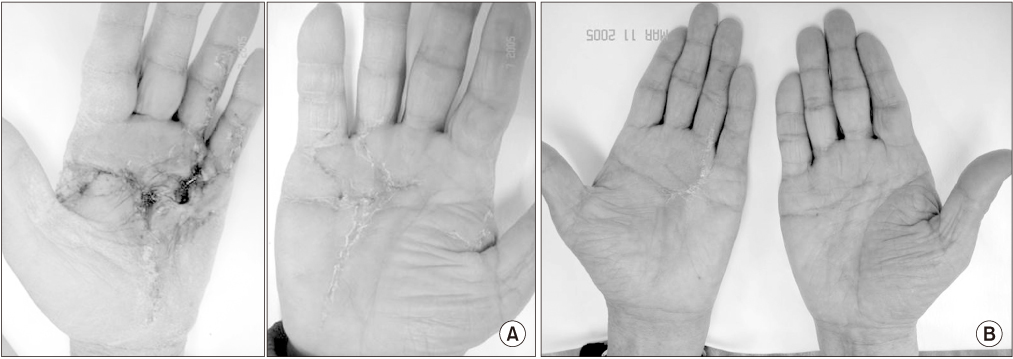
In the treatment of Dupuytren's contracture, the aim of optical treatment is to lower the recurrence rate and reduce complications. This paper reports the results of subtotal fasciectomy in Dupuytren's contracture, extending the excision of palmar fascial structures from the diseased to normal appearing adjacent fascial structure.
MATERIALS AND METHODS
From 2007 to 2017, 45 patients with Dupuytren's contracture treated by subtotal fasciectomy were reviewed retrospectively. The mean follow-up period was 45.9 months. Ninety-two digits were involved (index: 2, middle: 10, ring: 44, little: 36). The predisposing factors and affected joint were reviewed and the preoperative and postoperative contracture was measured. For clinical results, quick disabilities of the arm, shoulder, and hand (quick DASH) were used. Complications, including wound or skin problems, nerve injuries, hematoma, and complex regional pain syndrome, were assessed.
RESULTS
Preoperative flexion contracture was 43.2° in the proximal interphalangeal joint and 32.9° in the metacarpophalangeal joint. In nine cases, patients had residual contracture of 9.7° (range, 5°-20°) on average and if the total number of cases were included, the mean residual contracture was 2.3° on average. The quick DASH score at the 12 months follow-up was 12.4. The overall complication rate was 26.6%.
CONCLUSION
Subtotal fasciectomy can be a good surgical treatment option for Dupuytren's contracture with a low recurrence and low complication rate compared to other open procedures.
Keyword
MeSH Terms
Figure
Reference
-
1. Al-Qattan MM. Factors in the pathogenesis of Dupuytren's contracture. J Hand Surg Am. 2006; 31:1527–1534.
Article2. Hindocha S, McGrouther DA, Bayat A. Epidemiological evaluation of Dupuytren's disease incidence and prevalence rates in relation to etiology. Hand. 2009; 4:256–269.
Article3. Lanting R, Broekstra DC, Werker PM, van den Heuvel ER. A systematic review and meta-analysis on the prevalence of Dupuytren disease in the general population of Western countries. Plast Reconstr Surg. 2014; 133:593–603.
Article4. Saboeiro AP, Porkorny JJ, Shehadi SI, Virgo KS, Johnson FE. Racial distribution of Dupuytren's disease in Department of Veterans Affairs patients. Plast Reconstr Surg. 2000; 106:71–75.
Article5. Rayan GM. Nonoperative treatment of Dupuytren's disease. J Hand Surg Am. 2008; 33:1208–1210.
Article6. Badalamente MA, Hurst LC. Development of collagenase treatment for Dupuytren disease. Hand Clin. 2018; 34:345–349.
Article7. Slater RR Jr. Dupuytren disease: is collagenase better than needling?: commentary on an article by Joakim Strömberg, MD, et al.: “Percutaneous needle fasciotomy versus collagenase treatment for Dupuytren contracture. A randomized controlled trial with a two-year follow-up”. J Bone Joint Surg Am. 2018; 100:e91.8. Sanjuan-Cerveró R, Carrera-Hueso FJ, Vazquez-Ferreiro P, Ramon-Barrios MA. Efficacy and adverse effects of collagenase use in the treatment of Dupuytren's disease: a meta-analysis. Bone Joint J. 2018; 100:73–80.9. McMillan C, Yeung C, Binhammer P. Variation in treatment recommendations for Dupuytren disease. J Hand Surg Am. 2017; 42:963–970.e6.
Article10. Costas B, Coleman S, Kaufman G, James R, Cohen B, Gaston RG. Efficacy and safety of collagenase clostridium histolyticum for Dupuytren disease nodules: a randomized controlled trial. BMC Musculoskelet Disord. 2017; 18:374.
Article11. Badalamente MA, Hurst LC. Enzyme injection as nonsurgical treatment of Dupuytren's disease. J Hand Surg Am. 2000; 25:629–636.
Article12. Dias JJ, Aziz S. Fasciectomy for Dupuytren contracture. Hand Clin. 2018; 34:351–366.
Article13. Tubiana R. Surgical management. In : Tubiana R, editor. The hand. Paris: Saunders;1999. p. 480.14. Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren's contracture. N Engl J Med. 2009; 361:968–979.
Article15. Felici N, Marcoccio I, Giunta R, et al. Dupuytren contracture recurrence project: reaching consensus on a definition of recurrence. Handchir Mikrochir Plast Chir. 2014; 46:350–354.
Article16. Elliot D. Pre-1900 literature on Dupuytren's disease. Hand Clin. 1999; 15:175–181.17. Hueston JT. Recurrent Dupuytren's contracture. Plast Reconstr Surg. 1963; 31:66–69.
Article18. McFarlane RM, Jamieson WG. Dupuytren's contracture. The management of one hundred patients. J Bone Joint Surg Am. 1966; 48:1095–1105.19. McFarlane RM, Flint MH, Cheung H. Epidemiology of surgical patients. In : McFarlane RM, McGrouther DA, Flint MH, editors. Dupuytren's disease: biology and treatment. Edinburgh: Churchill Livingstone;1990. p. 201–215.20. Boyer MI, Gelberman RH. Complications of the operative treatment of Dupuytren's disease. Hand Clin. 1999; 15:161–166. viii.
Article21. Eberlin KR, Mudgal CS. Complications of treatment for Dupuytren disease. Hand Clin. 2018; 34:387–394.
Article22. van Rijssen AL, Gerbrandy FS, Ter Linden H, Klip H, Werker PM. A comparison of the direct outcomes of percutaneous needle fasciotomy and limited fasciectomy for Dupuytren's disease: a 6-week follow-up study. J Hand Surg Am. 2006; 31:717–725.
Article23. van Rijssen AL, ter Linden H, Werker PM. Five-year results of a randomized clinical trial on treatment in Dupuytren's disease: percutaneous needle fasciotomy versus limited fasciectomy. Plast Reconstr Surg. 2012; 129:469–477.24. Hovius SER, Zhou C. Advances in minimally invasive treatment of dupuytren disease. Hand Clin. 2018; 34:417–426.
Article25. Kaplan FTD, Crosby NE. Treatment of recurrent Dupuytren disease. Hand Clin. 2018; 34:403–415.
Article26. Herrera FA, Benhaim P, Suliman A, Roostaeian J, Azari K, Mitchell S. Cost comparison of open fasciectomy versus percutaneous needle aponeurotomy for treatment of Dupuytren contracture. Ann Plast Surg. 2013; 70:454–456.
Article27. Dias JJ, Braybrooke J. Dupuytren's contracture: an audit of the outcomes of surgery. J Hand Surg Br. 2006; 31:514–521.
Article28. Binhammer P. Comparative outcomes of Dupuytren disease treatment. Hand Clin. 2018; 34:377–386.
Article