J Korean Orthop Assoc.
2019 Aug;54(4):336-342. 10.4055/jkoa.2019.54.4.336.
Relationship between the Progression of Kyphosis in Thoracolumbar Osteoporotic Vertebral Compression Fractures and Magnetic Resonance Imaging Findings
- Affiliations
-
- 1Department of Orthopedic Surgery, Gachon University Gil Medical Center, Incheon, Korea. bbaik@hanmail.net
- KMID: 2455502
- DOI: http://doi.org/10.4055/jkoa.2019.54.4.336
Abstract
- PURPOSE
To examine the relationship between the progression of a kyphotic deformity and the magnetic resonance imaging (MRI) findings in conservatively treated osteoporotic thoracolumbar compression fracture patients.
MATERIALS AND METHODS
This study categorized the patients who underwent conservative treatment among those patients who underwent treatment under the suspicion of a thoracolumbar compression fracture from January 2007 to March 2016. Among them, this retrospective study included eighty-nine patients with osteoporosis and osteopenia with a bone density of less than −2.0 and single vertebral body fracture. This study examined the MRI of anterior longitudinal ligament or posterior longitudinal ligament injury, superior or inferior endplate disruption, superior of inferior intravertebral disc injury, the presence of low signal intensity on T2-weighted images, and bone edema of intravertebral bodies in fractured intravertebral bodies.
RESULTS
In cases where the superior endplate was disrupted or the level of bone edema of the intravertebral bodies was high, the kyphotic angle, wedge angle, and anterior vertebral compression showed remarkably progression. In the case of damage to the anterior longitudinal ligament or the superior disc, only the kyphotic angle was markedly prominent. On the T2-weighted images, low signal intensity lesions showed a high wedge angle and high anterior vertebral compression. On the other hand, there were no significant correlations among the posterior longitudinal ligament injury, inferior endplate disruption, inferior disc injury, and the progression of kyphotic deformity and vertebral compression. The risk factors that increase the kyphotic angle by more than 5° include the presence of injuries to the anterior longitudinal ligament, superior endplate disruption, and superior disc injury, and the risk factors were 21.3, 5.1, and 8.5 times higher than those of the uninjured case, and the risk differed according to the level of bone edema.
CONCLUSION
An osteoporotic thoracolumbar compression fracture in osteoporotic or osteopenic patients, anterior longitudinal ligament injury, superior endplate and intravertebral disc injury, and high level of edema in the MRI were critical factors that increases the risk of kyphotic deformity.
Keyword
MeSH Terms
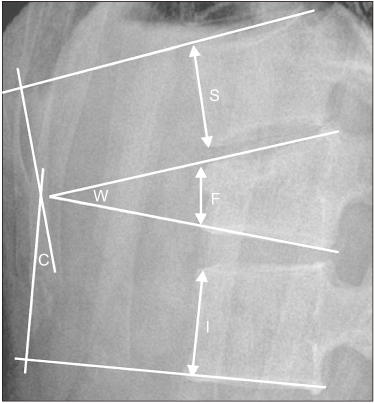
Figure
Reference
-
1. Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine (Phila Pa 1976). 1993; 18:971–976.
Article2. Krompinger WJ, Fredrickson BE, Mino DE, Yuan HA. Conservative treatment of fractures of the thoracic and lumbar spine. Orthop Clin North Am. 1986; 17:161–170.
Article3. Reid AB, Letts RM, Black GB. Pediatric chance fractures: association with intra-abdominal injuries and seatbelt use. J Trauma. 1990; 30:384–391.4. Ağuş H, Kayali C, Arslantaş M. Nonoperative treatment of burst-type thoracolumbar vertebra fractures: clinical and radiological results of 29 patients. Eur Spine J. 2005; 14:536–540.
Article5. Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar “burst” fractures treated conservatively: a long-term follow-up. Spine (Phila Pa 1976). 1988; 13:33–38.
Article6. Chow GH, Nelson BJ, Gebhard JS, Brugman JL, Brown CW, Donaldson DH. Functional outcome of thoracolumbar burst fractures managed with hyperextension casting or bracing and early mobilization. Spine (Phila Pa 1976). 1996; 21:2170–2175.
Article7. James KS, Wenger KH, Schlegel JD, Dunn HK. Biomechanical evaluation of the stability of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1994; 19:1731–1740.
Article8. Denis F, Armstrong GW, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984; (189):142–149.
Article9. Gertzbein SD. Scoliosis research society Multicenter spine fracture study. Spine (Phila Pa 1976). 1992; 17:528–540.10. Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures The clinical efficacy and outcome of nonoperativemanagement. Spine (Phila Pa 1976). 1993; 18:955–955.11. Oner FC, van Gils AP, Faber JA, Dhert WJ, Verbout AJ. Some complications of common treatment schemes of thoracolumbar spine fractures can be predicted with magnetic resonance imaging: prospective study of 53 patients with 71 fractures. Spine (Phila Pa 1976). 2002; 27:629–636.12. Williams RL, Hardman JA, Lyons K. MR imaging of suspected acute spinal instability. Injury. 1998; 29:109–113.
Article13. Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures The clinical efficacy and outcome of nonoperativemanagement. Spine (Phila Pa 1976). 1993; 18:955–955.14. Young MH. Long-term consequences of stable fractures of the thoracic and lumbar vertebral bodies. J Bone Joint Surg Br. 1973; 55:295–300.
Article15. Alanay A, Yazici M, Acaroglu E, Turhan E, Cila A, Surat A. Course of nonsurgical management of burst fractures with intact posterior ligamentous complex: an MRI study. Spine (Phila Pa 1976). 2004; 29:2425–2431.
Article16. Jacobs RR, Asher MA, Snider RK. Thoracolumbar spinal injuries A comparative study of recumbent and operative treatment in 100 patients. Spine (Phila Pa 1976). 1980; 5:463–477.17. Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine (Phila Pa 1976). 2003; 28:2459–2465.
Article18. Oner FC, van Gils AP, Dhert WJ, Verbout AJ. MRI findings of thoracolumbar spine fractures: a categorisation based on MRI examinations of 100 fractures. Skeletal Radiol. 1999; 28:433–443.
Article19. Petersilge CA, Pathria MN, Emery SE, Masaryk TJ. Thoracolumbar burst fractures: evaluation with MR imaging. Radiology. 1995; 194:49–54.
Article20. Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003; 85:773–781.21. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994; 3:184–201.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Factors between the Progression of the Compression Rate and Magnetic Resonance Imaging Findings in Osteoporotic Vertebral Fracture Patients Treated with Teriparatide
- Correlation between Progression of Compression and Bone Densiometry Index in Osteoporotic Compression Fracture of Thoracolumbar Spine
- The Influence of Initial Magnetic Resonance Imaging Findings on the Compression Rate of Thoracolumbar Osteoporotic Vertebral Compression Fracture
- The Relationship between the Progression of Kyphosis in Stable Thoracolumbar Fractures and Magnetic Resonance Imaging Findings
- Influence of Compression Ratio Differences between Magnetic Resonance Images and Simple Radiographs on Osteoporotic Vertebral Compression Fracture Prognosis after Vertebroplasty