J Korean Ophthalmol Soc.
2019 Aug;60(8):802-807. 10.3341/jkos.2019.60.8.802.
Two Case Reports of a Purtscher-like Retinopathy Occurring after Retrobulbar Anesthesia
- Affiliations
-
- 1Department of Ophthalmology, Wonkwang University College of Medicine, Iksan, Korea. ardin@hanmail.net
- 2Institute of Wonkwang Medical Science, Wonkwang University, Iksan, Korea.
- KMID: 2455465
- DOI: http://doi.org/10.3341/jkos.2019.60.8.802
Abstract
- PURPOSE
Although there are significant risks, retrobulbar anesthesia is commonly used for eye surgery. We report two cases of Purtscher-like retinopathy, a rare complication.
CASE SUMMARY
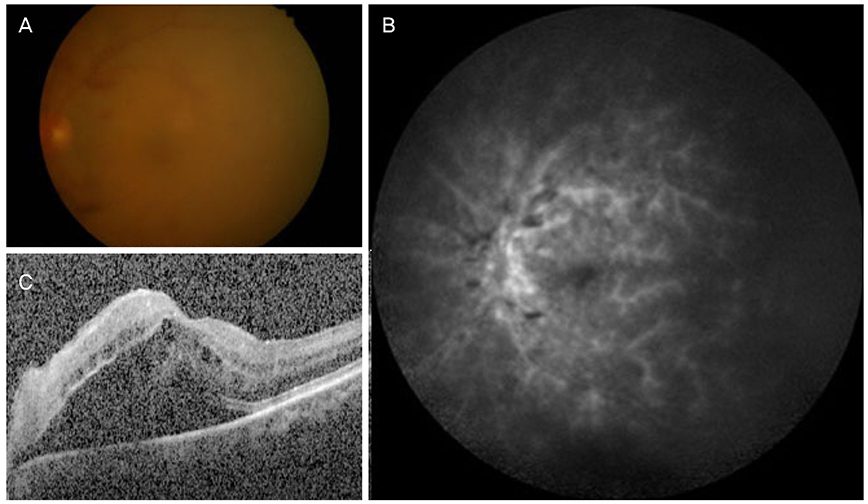
(Case 1) A 76-year-old female visited our hospital because of decreased vision. She underwent right cataract surgery with retrobulbar anesthesia. After 7 days, she had decreased visual acuity (VA) and a constricted visual field. Multiple white spots and cotton wool spots around the optic nerve and post pole, macular edema (ME), and subretinal fluid (SRF) were found using a fundus examination. A non-perfusion area and staining of the vascular wall were seen using fluorescence angiography. Although carotid arterial angiography, thrombolysis, and intravenous injection of high-dose steroids were performed, the ME and SRF persisted. After intravitreal aflibercept was injected twice (2-month interval), the ME and SRF decreased and remained stable. (Case 2) A 61-year-old male underwent left cataract surgery with retrobulbar anesthesia. After anesthesia, the VA of the left eye was 10 cm finger count. The fundus examination showed multiple hemorrhage blots and retinal hemorrhages, and hyperfluorescence around the optic nerve and post pole; vascular wall staining revealed a Purtscher-like retinopathy. Left carotid arterial angiography, thrombolysis, and intravenous injection of high-dose steroids were then performed. After treatment, the VA of the left eye, ME, and SRF were improved at the 4-month follow-up.
CONCLUSIONS
We report rare complications of retrobulbar anesthesia, with active and timely treatment having a positive impact on the visual prognosis.
MeSH Terms
Figure
Reference
-
1. Morgan CM, Schartz H, Vine AK, et al. Ocular complications associated with retrobulbar injections. Ophthalmology. 1988; 95:660–665.
Article2. Nicoll JM, Acharya PA, Ahlen K, et al. Central nervous system complications after 6,000 retrobulbar block. Anesth Analg. 1987; 66:1298–1302.3. Jacob HS, Craddock PR, Hammerschmidt DE, Moldow CF. Complement-induced granulocyte aggregation: an unsuspected mechanism of disease. N Engl J Med. 1980; 302:789–794.4. Chuang EL, Miller FS 3rd, Kalina RE. Retinal lesions following long bone fracture. Ophthalmology. 1985; 92:370–374.5. Purtscher O. Traumatic retinal angiopathy. Lymph assosiated syndrome. Graefes Arch Clin Exp Ophthalmol. 1912; 2:347–371.6. Agrawal A, McKibbin MA. Purtscher’s and Purtscher-like retinopathies: a review. Surv Ophthalmol. 2006; 51:129–136.
Article7. Beckingsale AB, Rosenthal AR. Early fundus fluorescein angiographic findings and sequelae in traumatic retinopathy: case report. Br J Ophthalmol. 1983; 67:119–123.
Article8. Lemagne JM, Michiels X, Van Causenbroeck S, Snyers B. Purtscher-like retinopathy after retrobulbar anesthesia. Ophthalmology. 1990; 97:859–861.
Article9. Blodi BA, Williams CA. Purtscher-like retinopathy after uncomplicated administration of retrobulbar anesthesia. Am J Ophthalmol. 1997; 124:702–703.
Article10. Atabay C, Kansu T, Nurlu G. Late visual recovery after intravenous methylprednisolone treatment of Purtscher's retinopathy. Ann Ophthalmol. 1993; 25:330–333.11. Bojić L, Ivanisević M, Gosović G. Hyperbaric oxygen therapy in two patients with non-arteritic anterior optic neuropathy who did not respond to prednisone. Undersea Hyperb Med. 2002; 29:86–92.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Purtscher's-lke Retinopathy in Patients with Systemic Hypertension
- Acute Pancreatitis with Purtscher's-like Retinopathy
- A Case of Purtscher's Retinopathy
- Purtscher-like Retinopathy after Aortic Valve Replacement Surgery
- Central Retinal Artery Occlusion Without Retrobular Hemorrhage after Retrobulbar Anesthesia