World J Mens Health.
2019 Sep;37(3):364-371. 10.5534/wjmh.180084.
The Relationships between Thyroid Hormone Levels and Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia
- Affiliations
-
- 1Department of Urology, National Police Hospital, Seoul, Korea.
- 2Department of Urology, Samsung Medical Center, Samsung Biomedical Research Institute, Sungkyunkwan University School of Medicine, Seoul, Korea. drswlee@skku.edu
- KMID: 2455413
- DOI: http://doi.org/10.5534/wjmh.180084
Abstract
- PURPOSE
We examined the association between thyroid hormone and lower urinary tract symptoms (LUTS)/benign prostatic hyperplasia (BPH).
MATERIALS AND METHODS
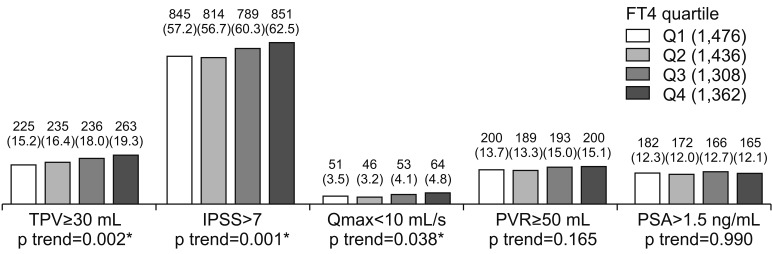
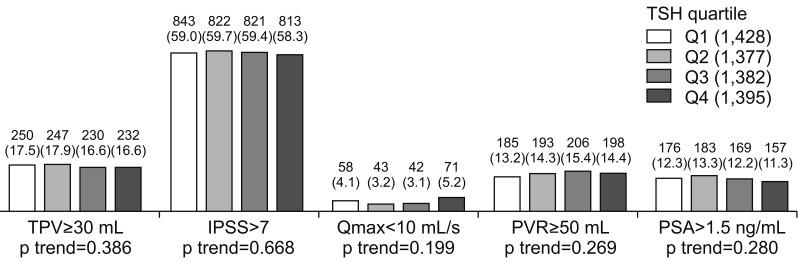
A total of 5,708 middle aged men were included. LUTS/BPH were assessed using the international prostate symptom score (IPSS), total prostate volume (TPV), maximal flow rate (Qmax), and a full metabolic workup. Thyroid stimulating hormone (TSH) and free thyroxine (FT4) levels were measured using chemiluminescence immunoassay. We divided participants into quartiles based on their TSH and FT4 levels: first to fourth quartile (Q1-Q4).
RESULTS
There was a significant increase in the percentage of men with IPSS>7, Qmax<10 mL/s, and TPV≥30 mL with increase of FT4 quartile. The adjusted odds ratio (OR) for TPV≥30 mL and IPSS>7 were significantly different between FT4 quartile groups (ORs; [5-95 percentile interval], p; TPV≥30 mL, Q1: 0.000 [references]; Q2: 1.140 [0.911-1.361], p=0.291; Q3: 1.260 [1.030-1.541], p=0.025; Q4: 1.367 [1.122-1.665], p=0.002; IPSS>7: Q1: 0.000 [references]; Q2: 0.969 [0.836-1.123], p=0.677; Q3: 1.123 [0.965-1.308], p=0.133; Q4: 1.221 [1.049-1.420], p=0.010). In men with above median levels of testosterone, the FT4 correlated positively with TPV, even after adjusting for confounders. However, the FT4 was not correlated with TPV in men with below median levels of testosterone. TSH was not related to LUTS/BPH measurements.
CONCLUSIONS
TPV, IPSS, and Qmax were significantly related to FT4. TPV and IPSS were significantly and independently related to FT4. Additionally, the relationship between FT4 and TPV was distinct when testosterone levels are high.
MeSH Terms
Figure
Cited by 2 articles
-
Thyroid Prostate Axis. Does It Really Exist?
Sandro La Vignera, Rosita A. Condorelli, Rossella Cannarella, Aldo E. Calogero
World J Mens Health. 2019;37(3):257-260. doi: 10.5534/wjmh.190060.Thyroid Prostate Axis. Does It Really Exist?
Sandro La Vignera, Rosita A. Condorelli, Rossella Cannarella, Aldo E. Calogero
World J Mens Health. 2019;37(3):257-260. doi: 10.5534/wjmh.190060.
Reference
-
1. Ziada A, Rosenblum M, Crawford ED. Benign prostatic hyperplasia: an overview. Urology. 1999; 53(3 Suppl 3a):1–6. PMID: 10094094.
Article2. La Vignera S, Condorelli RA, Russo GI, Morgia G, Calogero AE. Endocrine control of benign prostatic hyperplasia. Andrology. 2016; 4:404–411. PMID: 27089546.
Article3. Hercbergs A. The thyroid gland as an intrinsic biologic response-modifier in advanced neoplasia: a novel paradigm. In Vivo. 1996; 10:245–247. PMID: 8744809.4. Moeller LC, Führer D. Thyroid hormone, thyroid hormone receptors, and cancer: a clinical perspective. Endocr Relat Cancer. 2013; 20:R19–R29. PMID: 23319493.
Article5. Anil C, Guney T, Gursoy A. The prevalence of benign breast diseases in patients with nodular goiter and Hashimoto's thyroiditis. J Endocrinol Invest. 2015; 38:971–975. PMID: 25827711.
Article6. Spinos N, Terzis G, Crysanthopoulou A, Adonakis G, Markou KB, Vervita V, et al. Increased frequency of thyroid nodules and breast fibroadenomas in women with uterine fibroids. Thyroid. 2007; 17:1257–1259. PMID: 17988198.
Article7. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67:1099–1109. PMID: 25613154.
Article8. Kim SH, Kim SH. Correlations between the various methods of estimating prostate volume: transabdominal, transrectal, and three-dimensional US. Korean J Radiol. 2008; 9:134–139. PMID: 18385560.
Article9. Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin North Am. 2016; 43:289–297. PMID: 27476122.10. Barry MJ, Fowler FJ Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992; 148:1549–1557. PMID: 1279218.11. Huh JS, Kim YJ, Kim SD. Prevalence of benign prostatic hyperplasia on Jeju Island: analysis from a cross-sectional community-based survey. World J Mens Health. 2012; 30:131–137. PMID: 23596600.
Article12. Lim KB, Ho H, Foo KT, Wong MY, Fook-Chong S. Comparison of intravesical prostatic protrusion, prostate volume and serum prostatic-specific antigen in the evaluation of bladder outlet obstruction. Int J Urol. 2006; 13:1509–1513. PMID: 17118026.
Article13. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005; 112:2735–2752. PMID: 16157765.14. Lepor H. Pathophysiology of benign prostatic hyperplasia: insights from medical therapy for the disease. Rev Urol. 2009; 11:S9–S13. PMID: 20126609.15. Lehrer S, Diamond EJ, Stone NN, Droller MJ, Stock RG. Serum triiodothyronine is increased in men with prostate cancer and benign prostatic hyperplasia. J Urol. 2002; 168:2431–2433. PMID: 12441933.
Article16. Eldhose A, Nandeesha H, Dorairajan LN, Sreenivasulu K, Arul Vijaya Vani S. Thyroid and parathyroid hormones in benign prostatic hyperplasia. Br J Biomed Sci. 2016; 73:94–96. PMID: 27181171.
Article17. Khan SR, Chaker L, Ruiter R, Aerts JG, Hofman A, Dehghan A, et al. Thyroid function and cancer risk: the Rotterdam study. J Clin Endocrinol Metab. 2016; 101:5030–5036. PMID: 27648963.
Article18. Kress E, Samarut J, Plateroti M. Thyroid hormones and the control of cell proliferation or cell differentiation: paradox or duality. Mol Cell Endocrinol. 2009; 313:36–49. PMID: 19737599.
Article19. Roberts RO, Jacobson DJ, Rhodes T, Klee GG, Leiber MM, Jacobsen SJ. Serum sex hormones and measures of benign prostatic hyperplasia. Prostate. 2004; 61:124–131. PMID: 15305335.
Article20. Moore RJ, Gazak JM, Quebbeman JF, Wilson JD. Concentration of dihydrotestosterone and 3 alpha-androstanediol in naturally occurring and androgen-induced prostatic hyperplasia in the dog. J Clin Invest. 1979; 64:1003–1010. PMID: 90055.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Trend of the Primary Treatment in Lower Urinary Tract Symptom/Benign Prostatic Hyperplasia
- A Study on Physiological Index, Anxiety and Depression by the Severity of Lower Urinary Tract Symptoms in Patients with Benign Prostatic Hyperplasia
- Prostate Artery Embolization: Treatment of Symptomatic Benign Prostatic Hyperplasia
- The Relationship between Benign Prostate Hyperplasia and Erectile Dysfunction: What is Reality?
- Benign Prostatic Hyperplasia and Sexual Dysfunction