World J Mens Health.
2019 Sep;37(3):355-363. 10.5534/wjmh.180081.
Roles of Ureaplasma Species in Idiopathic Chronic Prostatitis: A Case-Control Study
- Affiliations
-
- 1Department of Urology, Dankook University College of Medicine, Cheonan, Korea. multiorigins@yahoo.com
- KMID: 2455412
- DOI: http://doi.org/10.5534/wjmh.180081
Abstract
- PURPOSE
Because of the inconsistent symptoms associated with Ureaplasma infections, their clinical significances in genitourinary tracts are under debate. Therefore, we evaluated the presence of Ureaplasma urealyticum (UU) and Ureaplasma parvum (UP) in urine samples and examined their associations with chronic prostatitis (CP) through a case and control study.
MATERIALS AND METHODS
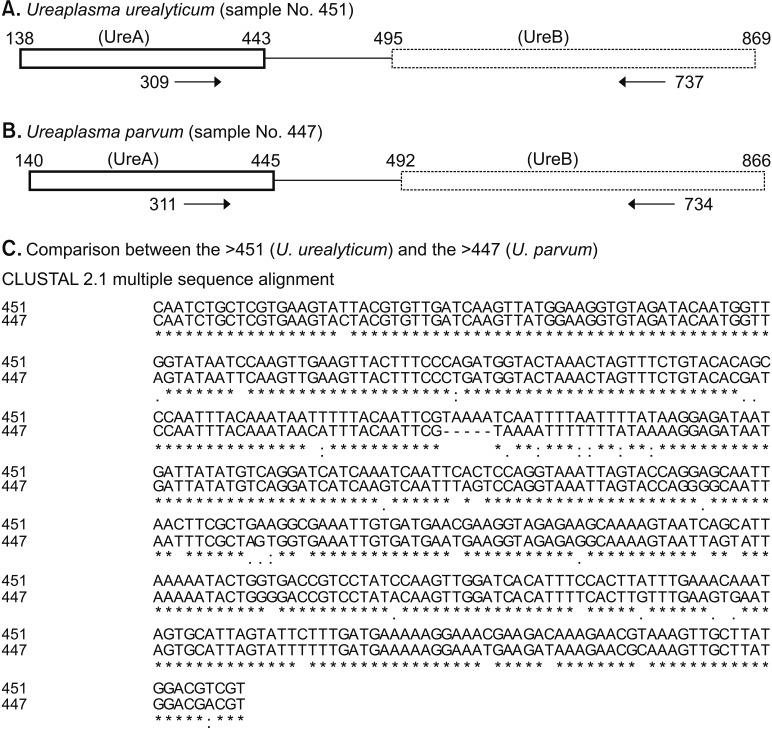
We included 696 nonchlamydial nongonococcal (NCNG) urine samples from men; 350 were categorized into non-inflammatory CP, 88 in inflammatory CP, and 258 in non-CP group. We amplified a region in the Ureaplasma urease areas from these samples and determined their biovars using the Sanger method.
RESULTS
Among the NCNG population, the rates of UU, UP, and non-UU/UP were 3.88%, 6.46%, and 89.66%, respectively. The overall infection rates of non-CP, inflammatory CP, and non-inflammatory CP groups were 4.15%, 6.10%, and 3.65% in UU (p=0.612) and 6.85%, 7.22%, and 6.50% in UP (p=0.968), respectively. UU infection increased the risk of white blood cell (WBC) counts (≥5) in urine (p=0.005). In contrast, UP infections did not increase the risks of urethritis. Re-analysis from the 633 men who were excluded from urethritis effects did not reveal the associations between UU infection and the clinical characteristics of CP. Furthermore, the profiles from the National Institutes of Health-Chronic Prostatitis Symptom Index questionnaire and WBC counts in expressed prostatic secretion were similar among the non-CP and the two CP groups in each Ureaplasma infection.
CONCLUSIONS
We found that UU may induce male urethritis. However, Ureapalsma species in urine were not definitively associated with the occurrence of CP.
MeSH Terms
Figure
Reference
-
1. Pollack JD. Ureaplasma urealyticum: an opportunity for combinatorial genomics. Trends Microbiol. 2001; 9:169–175. PMID: 11286881.
Article2. Miles R, Nicholas R. Introduction. In : Miles R, Nicholas R, editors. Mycoplasma protocols. Totowa: Humana Press;1998. p. 1–5.3. Nguyen CT, Shoskes DA. Evaluation of the prostatitis patient. In : Shoskes DA, editor. Chronic prostatitis/chronic pelvic pain syndrome. Totowa: Humana Press;2008. p. 1–16.4. Krieger JN, Riley DE, Roberts MC, Berger RE. Prokaryotic DNA sequences in patients with chronic idiopathic prostatitis. J Clin Microbiol. 1996; 34:3120–3128. PMID: 8940458.
Article5. Park H, Sim SM, Lee G. The presence of Chlamydia is associated with increased leukocyte counts and pain severity in men with chronic pelvic pain syndrome. Urology. 2015; 85:574–579. PMID: 25733268.
Article6. Choe HS, Lee DS, Lee SJ, Hong SH, Park DC, Lee MK, et al. Performance of Anyplex™ II multiplex real-time PCR for the diagnosis of seven sexually transmitted infections: comparison with currently available methods. Int J Infect Dis. 2013; 17:e1134–e1140. PMID: 24095619.
Article7. Xiao J, Ren L, Lv H, Ding Q, Lou S, Zhang W, et al. Atypical microorganisms in expressed prostatic secretion from patients with chronic prostatitis/chronic pelvic pain syndrome: microbiological results from a case-control study. Urol Int. 2013; 91:410–416. PMID: 23970289.
Article8. Skerk V, Krhen I, Schonwald S, Cajic V, Markovinovic L, Roglic S, et al. The role of unusual pathogens in prostatitis syndrome. Int J Antimicrob Agents. 2004; 24(Suppl 1):S53–S56. PMID: 15364308.
Article9. Frølund M, Lidbrink P, Wikström A, Cowan S, Ahrens P, Jensen JS. Urethritis-associated pathogens in urine from men with non-gonococcal urethritis: a case-control study. Acta Derm Venereol. 2016; 96:689–694. PMID: 26658669.
Article10. Irajian G, Sharifi M, Mirkalantari S, Mirnejad R, Jalali Nadoushan MR, Ghorbanpour N. Molecular detection of ureaplasma urealyticum from prostate tissues using PCR-RFLP, Tehran, Iran. Iran J Pathol. 2016; 11:138–143. PMID: 27499775.11. Seo Y, Lee G. Antimicrobial resistance pattern in Enterococcus faecalis strains isolated from expressed prostatic secretions of patients with chronic bacterial prostatitis. Korean J Urol. 2013; 54:477–481. PMID: 23878692.12. Lee G, Park J, Kim B, Kim SA, Yoo CK, Seong WK. OmpA genotyping of Chlamydia trachomatis from Korean female sex workers. J Infect. 2006; 52:451–454. PMID: 16233917.
Article13. Delva D. Social implications of sexually transmitted diseases. Can Fam Physician. 1983; 29:1933–1936. PMID: 21283431.14. Del Prete R, Ronga L, Lestingi M, Addati G, Angelotti UF, Di Carlo D, et al. Simultaneous detection and identification of STI pathogens by multiplex real-time PCR in genital tract specimens in a selected area of Apulia, a region of Southern Italy. Infection. 2017; 45:469–477. PMID: 28260146.
Article15. Unemo M, Bradshaw CS, Hocking JS, de Vries HJC, Francis SC, Mabey D, et al. Sexually transmitted infections: challenges ahead. Lancet Infect Dis. 2017; 17:e235–e279. PMID: 28701272.
Article16. Moi H, Reinton N, Randjelovic I, Reponen EJ, Syvertsen L, Moghaddam A. Urethral inflammatory response to ureaplasma is significantly lower than to Mycoplasma genitalium and Chlamydia trachomatis. Int J STD AIDS. 2017; 28:773–780. PMID: 27558163.
Article17. Brosh-Nissimov T, Kedem R, Ophir N, Shental O, Keller N, Amit S. Management of sexually transmissible infections in the era of multiplexed molecular diagnostics: a primary care survey. Sex Health. 2018; 15:298–303. PMID: 29706149.
Article18. Redelinghuys MJ, Ehlers MM, Dreyer AW, Lombaard HA, Kock MM. Antimicrobial susceptibility patterns of Ureaplasma species and Mycoplasma hominis in pregnant women. BMC Infect Dis. 2014; 14:171. PMID: 24679107.
Article19. Beeton ML, Spiller OB. Antibiotic resistance among Ureaplasma spp. isolates: cause for concern? J Antimicrob Chemother. 2017; 72:330–337. PMID: 27798207.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of the Isolation of Ureaplasma Urealyticum in Nongonococcal Urethritis
- The Concentrations of Zinc in Expressed Prostatic Secretion of Chronic Prostatitis Patients
- Ureaplasma urealyticum or Ureaplasma parvum: what's the difference?
- Prednisolone Provocative Test for Chronic Prostatitis
- Ureaplasma infections in pre-term infants: Recent information regarding the role of Ureaplasma species as neonatal pathogens