World J Mens Health.
2019 Sep;37(3):296-312. 10.5534/wjmh.190055.
Male Oxidative Stress Infertility (MOSI): Proposed Terminology and Clinical Practice Guidelines for Management of Idiopathic Male Infertility
- Affiliations
-
- 1American Center for Reproductive Medicine, Cleveland Clinic, OH, USA. agarwaa@ccf.org
- 2Department of Urology, Cleveland Clinic, Cleveland, OH, USA.
- 3Department of Medical Bioscience, University of the Western Cape, Cape Town, South Africa.
- 4Department of Urology, Lilavati Hospital and Research Centre, Mumbai, India.
- 5School of Biosciences, University of Kent, Canterbury, UK.
- 6Department of Urology, University of Miami, Miami, FL, USA.
- 7Department of Urology, Loma Linda University Health, Loma Linda, CA, USA.
- 8Department of Obstetrics Gynaecology and Reproductive Medicine, Flinders University, Bedford Park, Australia.
- 9Division of Urology, Department of Surgery, University of Campinas (UNICAMP), Campinas, Brazil.
- 10Faculty of Health, Aarhus University, Aarhus, Denmark.
- 11Department of Urology, Hamad Medical Corporation and Weill Cornell Medicine-Qatar, Doha, Qatar.
- 12Centro Androgen, La Coruña, Spain and Harvard Medical School, Boston, MA, USA.
- 13School of BioSciences, University of Melbourne, Parkville, Australia.
- 14Section of Investigative Medicine, Imperial College London, UK.
- 15Department of Andrology, Hammersmith Hospital, London, UK.
- 16Department of Surgery, Union Hospital, Shatin, Hong Kong.
- 17Department of Dermatology, Venereology and Andrology, Faculty of Medicine, Sohag University, Sohag, Egypt.
- 18Boston IVF, Waltham, MA, USA.
- 19Department of Urology, University of Utah, Salt Lake City, UT, USA.
- 20Cooper University Hospital, Camden, NJ, USA.
- 21Departamento de BiologÃa, Universidad Autónoma de Madrid, Madrid, Spain.
- 22Department of Urology, Pusan National University School of Medicine, Busan, Korea.
- 23Medical Research Institute of Pusan National University Hospital, Busan, Korea.
- 24Department of Surgery, McGill University, Montreal, QC, Canada.
- 25Austin Fertility & Reproductive Medicine/Westlake IVF, Austin, TX, USA.
- 26Uromedica Polyclinic, Kneza Milosa, Belgrade, Serbia.
- 27Department of Urology, University of Virginia, Charlottesville, VA, USA.
- 28Sapienza University of Rome, Rome, Italy.
- 29Istanbul Florence Nightingale Hospital, Istanbul, Turkey.
- 30Department of Dermatology, University Hospital Bonn, Bonn, Germany.
- 31Division of Endocrinology, Department of Clinical and Molecular Sciences, Polytechnic University of Marche, Umberto I Hospital, Ancona, Italy.
- 32IVI Foundation Edificio Biopolo - Instituto de Investigación Sanitaria la Fe, Valencia, Spain.
- 33University Hospital, School of Médicine and PERITOX Laboratory, Amiens, France.
- 34Division of Urology, Southern Illinois University School of Medicine, Springfield, IL, USA.
- 35Centre for Human Reproductive Science, IMSR, College of Medical & Dental Sciences, The University of Birmingham Edgbaston, UK.
- 36The Birmingham Women's Fertility Centre, Birmingham Women's and Children's NHS Foundation Trust, Mindelsohn Drive, Edgbaston, UK.
- 37Department of Obstetrics and Gynaecology, University of Toronto, Toronto, ON, Canada.
- 38Reproductive Medicine Center, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China.
- 39Fertility Medical Group, São Paulo, Brazil.
- 40Department of Obstetrics & Gynecology, Andrology Unit Faculties of Health Sciences, Tygerberg Hospital, Tygerberg, South Africa.
- 41Department of Urology, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
- 42IVF Japan Group, Horac Grand Front Osaka Clinic, Osaka, Japan.
- 43Manipal Fertility, Bangalore, India.
- 44Genk Institute for Fertility Technology, Genk, Belgium.
- 45Hasselt University, Biomedical Research Institute, Diepenbeek, Belgium.
- 46Department of Experimental and Clinical Medicine, Center of Excellence DeNothe, University of Florence, Italy.
- 47Department of Experimental and Clinical Biomedical Sciences “Mario Serioâ€, Unit of Sexual Medicine and Andrology, Center of Excellence DeNothe, University of Florence, Florence, Italy.
- 48Department of Urology, Reproduction Center, Yokohama City University Medical Center, Yokohama, Japan.
- 49Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy.
- 50Androbest Andrology & Urology Center, Hyderabad, India.
- 51Section of Urology, University of Santo Tomas Hospital, Manila, Philippines.
- 52SCSA Diagnostics, Brookings, SD, USA.
- 53Fleury Group and Hospital Israelita Albert Einstein, São Paulo, Brazil.
- 54Origen, Center for Reproductive Medicine, Rio de Janeiro, Brazil.
- 55Department of Urology, University of São Paulo (USP), Brazil.
- 56Division of Urology, Infertility Center ALFA, São Paulo, Brazil.
- 57Head of Male Infertility Division, Andrology Department, Brazilian Society of Urology, Rio de Janeiro, Brazil.
- 58Fertility and IVF Unit, Department of Obstetrics and Gynecology, Hebrew-University Hadassah Medical Center, Jerusalem, Israel.
- 59Infertility and IVF Unit, Department of Obstetrics and Gynecology, Chaim Sheba Medical Center (Tel Hashomer), Ramat Gan, Israel.
- 60Tarnesby-Tarnowski Chair for Family Planning and Fertility Regulation, Sackler Faculty of Medicine, Tel-Aviv University, Tel Aviv, Israel.
- 61Soroka University Medical Center, Ben-Gurion University of the Negev Beer-Sheva, Beersheba, Israel.
- 62IVF Unit, Meir Medical Center, Kfar Sava, Israel.
- 63Sackler Medicine School, Tel Aviv University, Tel Aviv, Israel.
- 64Department of Urology, Hamad Medical Corporation, Doha, Qatar.
- 65Department of Andrology and Urology, Diyos Hospital, New Delhi, India.
- 66PUR Clinic, South Lake Hospital, Clermont, FL, USA.
- 67University of Central Florida, Orlando, FL, USA.
- 68Baby Center, Institute for Reproductive Medicine, São Paulo, Brazil.
- 69College Institute of Clinical Research and Teaching Development, São Paulo, Brazil.
- 70Lab for Molecular Reproduction and Genetics, Anatomy, All India Institute of Medical Sciences, New Delhi, India.
- 71Department of Reproductive Biology, Hôpitaux Universitaires Paris Seine Saint-Denis, Bondy, France.
- 72Department of Reproductive Medicine and Embryology, Manipal Hospital, New Delhi, India.
- 73Department of Urology, Hacettepe University Faculty of Medicine, Ankara, Turkey.
- 74Department of Endocrinology/ Andrology, University Hospital Ghent, Ghent, Belgium.
- 75Department of Reproductive Medicine, Hannibal International Clinic, Tunis, Tunisia.
- 76Department of Obstetrics, Gynecology and Reproductive Medicine, Pierre Cherest and Hartman Clinics, Paris, France.
- 77Clinic of Urology, Clinical Centre of Serbia, Faculty of Medicine, University of Belgrade, Belgrade, Serbia.
- 78Department of Physiology, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh Campus, Jalan Hospital, Selangor, Malaysia.
- 79Department of Embryology, Faculty of Medicine, University of Sousse, Sousse, Tunisia.
- 80Department of Pediatrics, New York University School of Medicine, New York, NY, USA.
- 81Department of Obstetrics and Gynaecology, Lilavati Hospital and Research Centre, Mumbai, India.
- 82Department of Experimental Medicine, Sapienza University of Rome, Rome, Italy.
- 83School of Natural Medicine, University of the Western Cape, Cape Town, South Africa.
- 84Department of Andrology, Shahid Sadoughi Medical University, Yazd, Iran.
- 85Southend Fertility & IVF, Delhi, India.
- 86Department of Urology, School of Medicine, University of Ankara, Ankara, Turkey.
- 87Redox Biology Laboratory, Department of Zoology and Center of Excellence in Environment and Public Health, Ravenshaw University, Cutrack, India.
- 88Marrakech Fertility Institute, Marrakech, Morocco.
- 89Jindal Hospital, Meerut, India.
- 90Department of Urology, Istinye University Faculty of Medicine, Liv Hospital Ulus, Istanbul, Turkey.
- 91Department of Urology, Ege University School of Medicine, Ä°zmir, Turkey.
- 92Center of Urology, CODRA Hospital, Podgorica, Montenegro.
- 93Fertility and IVF Unit, Soroka University Medical Center, Ben Gurion University of the Negev, Beer Sheva, Israel.
- KMID: 2455407
- DOI: http://doi.org/10.5534/wjmh.190055
Abstract
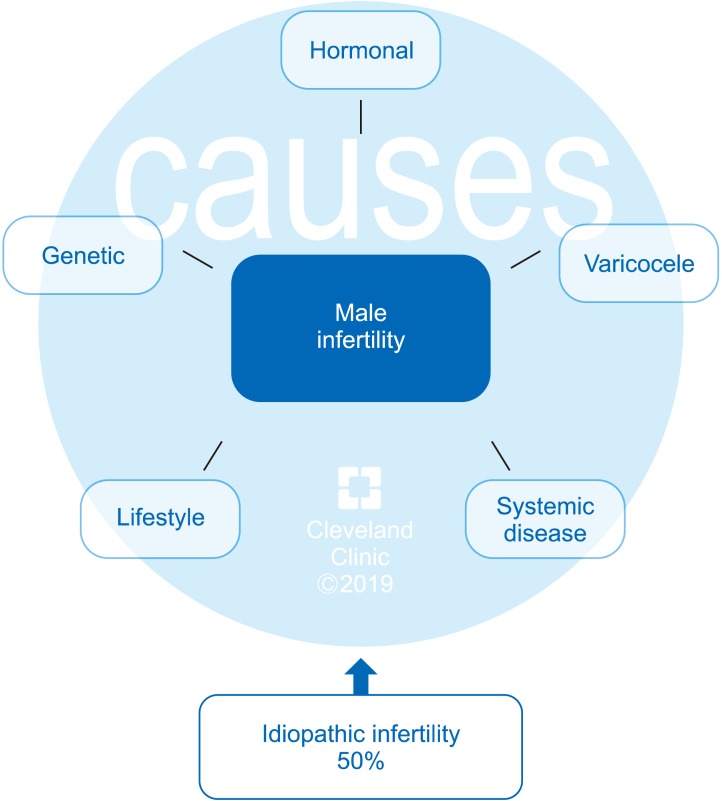
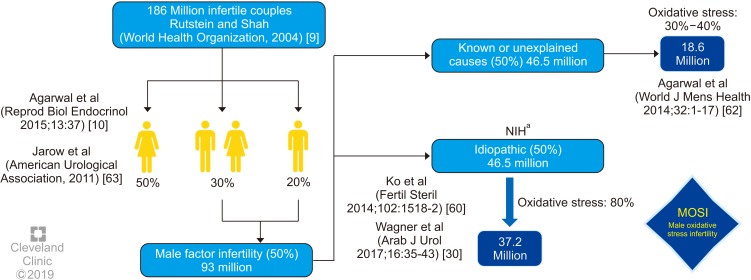
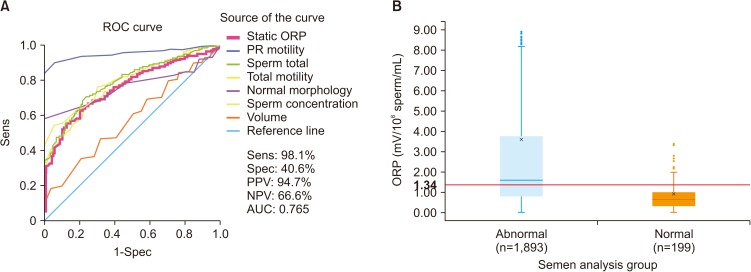
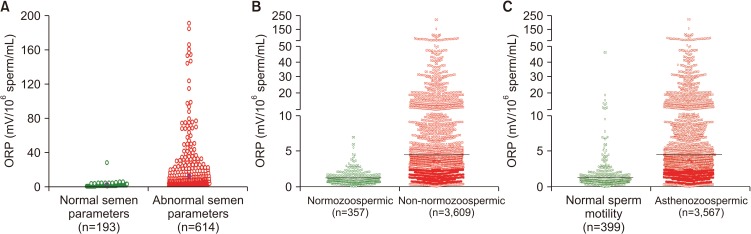
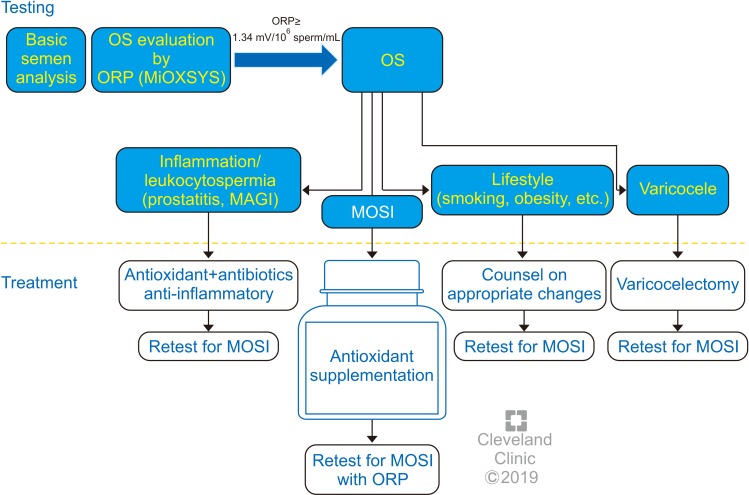
- Despite advances in the field of male reproductive health, idiopathic male infertility, in which a man has altered semen characteristics without an identifiable cause and there is no female factor infertility, remains a challenging condition to diagnose and manage. Increasing evidence suggests that oxidative stress (OS) plays an independent role in the etiology of male infertility, with 30% to 80% of infertile men having elevated seminal reactive oxygen species levels. OS can negatively affect fertility via a number of pathways, including interference with capacitation and possible damage to sperm membrane and DNA, which may impair the sperm's potential to fertilize an egg and develop into a healthy embryo. Adequate evaluation of male reproductive potential should therefore include an assessment of sperm OS. We propose the term Male Oxidative Stress Infertility, or MOSI, as a novel descriptor for infertile men with abnormal semen characteristics and OS, including many patients who were previously classified as having idiopathic male infertility. Oxidation-reduction potential (ORP) can be a useful clinical biomarker for the classification of MOSI, as it takes into account the levels of both oxidants and reductants (antioxidants). Current treatment protocols for OS, including the use of antioxidants, are not evidence-based and have the potential for complications and increased healthcare-related expenditures. Utilizing an easy, reproducible, and cost-effective test to measure ORP may provide a more targeted, reliable approach for administering antioxidant therapy while minimizing the risk of antioxidant overdose. With the increasing awareness and understanding of MOSI as a distinct male infertility diagnosis, future research endeavors can facilitate the development of evidence-based treatments that target its underlying cause.
MeSH Terms
-
Antioxidants
Classification
Clinical Protocols
Diagnosis
DNA
Embryonic Structures
Female
Fertility
Health Expenditures
Humans
Infertility*
Infertility, Male*
Male*
Membranes
Ovum
Oxidants
Oxidation-Reduction
Oxidative Stress*
Reactive Oxygen Species
Reducing Agents
Reproductive Health
Semen
Spermatozoa
Subject Headings
Antioxidants
DNA
Oxidants
Reactive Oxygen Species
Reducing Agents
Figure
Reference
-
1. Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, Sundaram R, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013; 99:1324–1331.e1. PMID: 23290741.
Article2. Kassa EM, Kebede E. Time-to-pregnancy and associated factors among couples with natural planned conception in Addis Ababa, Ethiopia. Afr J Reprod Health. 2018; 22:33–42. PMID: 30381930.3. Slama R, Hansen OK, Ducot B, Bohet A, Sorensen D, Giorgis Allemand L, et al. Estimation of the frequency of involuntary infertility on a nation-wide basis. Hum Reprod. 2012; 27:1489–1498. PMID: 22416008.
Article4. Juul S, Karmaus W, Olsen J. Regional differences in waiting time to pregnancy: pregnancy-based surveys from Denmark, France, Germany, Italy and Sweden. Hum Reprod. 1999; 14:1250–1254. PMID: 10325272.
Article5. Zinaman MJ, Clegg ED, Brown CC, O'Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil Steril. 1996; 65:503–509. PMID: 8774277.6. Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The international glossary on infertility and fertility care, 2017. Fertil Steril. 2017; 108:393–406. PMID: 28760517.
Article7. Practice Committee of American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2013; 99:63. PMID: 23095139.8. Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015; 21:411–426. PMID: 25801630.
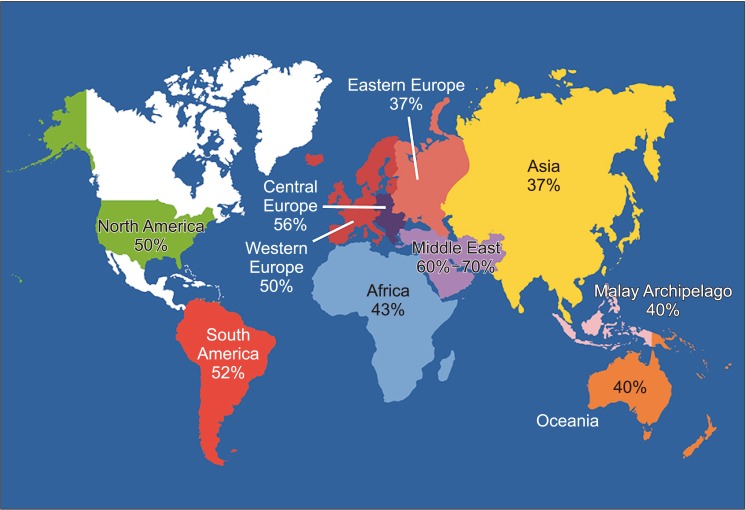
Article9. Rutstein SO, Shah IH. ORC Macro. World Health Organization. Infecundity, infertility, and childlessness in developing countries. Calverton: World Health Organization;2004.10. Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015; 13:37. PMID: 25928197.
Article11. World Health Organization. WHO laboratory manual for the examination and processing of human semen. Geneva: World Health Organization;2010.12. Irvine DS. Epidemiology and aetiology of male infertility. Hum Reprod. 1998; 13(Suppl 1):33–44.
Article13. O'Flynn O'Brien KL, Varghese AC, Agarwal A. The genetic causes of male factor infertility: a review. Fertil Steril. 2010; 93:1–12. PMID: 20103481.14. Sharma R, Biedenharn KR, Fedor JM, Agarwal A. Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol. 2013; 11:66. PMID: 23870423.
Article15. Jurewicz J, Dziewirska E, Radwan M, Hanke W. Air pollution from natural and anthropic sources and male fertility. Reprod Biol Endocrinol. 2018; 16:109. PMID: 30579357.
Article16. Punab M, Poolamets O, Paju P, Vihljajev V, Pomm K, Ladva R, et al. Causes of male infertility: a 9-year prospective monocentre study on 1737 patients with reduced total sperm counts. Hum Reprod. 2017; 32:18–31. PMID: 27864361.
Article17. Tournaye H, Krausz C, Oates RD. Novel concepts in the aetiology of male reproductive impairment. Lancet Diabetes Endocrinol. 2017; 5:544–553. PMID: 27395771.
Article18. Gabrielsen JS, Tanrikut C. Chronic exposures and male fertility: the impacts of environment, diet, and drug use on spermatogenesis. Andrology. 2016; 4:648–661. PMID: 27230702.
Article19. Pasqualotto FF, Pasqualotto EB, Sobreiro BP, Hallak J, Medeiros F, Lucon AM. Clinical diagnosis in men undergoing infertility investigation in a university hospital. Urol Int. 2006; 76:122–125. PMID: 16493211.
Article20. Chehab M, Madala A, Trussell JC. On-label and off-label drugs used in the treatment of male infertility. Fertil Steril. 2015; 103:595–604. PMID: 25660648.
Article21. Jungwirth A, Diemer T, Kopa Z, Krausz C, Minhas S, Tournaye H. EAU guidelines on male infertility. Arnhem: European Association of Urology;2018.23. Hamada A, Esteves SC, Agarwal A. Unexplained male infertility: potential causes and management. Hum Androl. 2011; 1:2–16.24. Agarwal A, Durairajanayagam D, Halabi J, Peng J, Vazquez-Levin M. Proteomics, oxidative stress and male infertility. Reprod Biomed Online. 2014; 29:32–58. PMID: 24813754.
Article25. Aitken RJ. Oxidative stress and the etiology of male infertility. J Assist Reprod Genet. 2016; 33:1691–1692. PMID: 27544275.
Article26. Bui AD, Sharma R, Henkel R, Agarwal A. Reactive oxygen species impact on sperm DNA and its role in male infertility. Andrologia. 2018; 50:e13012. PMID: 29644708.
Article27. Agarwal A, Sharma RK, Nallella KP, Thomas AJ Jr, Alvarez JG, Sikka SC. Reactive oxygen species as an independent marker of male factor infertility. Fertil Steril. 2006; 86:878–885. PMID: 17027357.
Article28. Tremellen K. Oxidative stress and male infertility: a clinical perspective. Hum Reprod Update. 2008; 14:243–258. PMID: 18281241.
Article29. Aitken RJ, De Iuliis GN, Drevet JR. Role of oxidative stress in the etiology of male infertility and the potential therapeutic value of antioxidants. In : Henkel R, Samanta L, Agarwal A, editors. Oxidants, antioxidants, and impact of the oxidative status in male reproduction. London: Elsevier/Academic Press;2018. p. 91–100.30. Wagner H, Cheng JW, Ko EY. Role of reactive oxygen species in male infertility: an updated review of literature. Arab J Urol. 2017; 16:35–43. PMID: 29713534.
Article31. Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996; 48:835–850. PMID: 8973665.
Article32. Aitken RJ. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol Reprod Dev. 2017; 84:1039–1052. PMID: 28749007.
Article33. Robinson JM. Phagocytic leukocytes and reactive oxygen species. Histochem Cell Biol. 2009; 131:465–469. PMID: 19224236.
Article34. Aitken RJ, West K, Buckingham D. Leukocytic infiltration into the human ejaculate and its association with semen quality, oxidative stress, and sperm function. J Androl. 1994; 15:343–352. PMID: 7982803.35. Cassina A, Silveira P, Cantu L, Montes JM, Radi R, Sapiro R. Defective human sperm cells are associated with mitochondrial dysfunction and oxidant production. Biol Reprod. 2015; 93:119. PMID: 26447142.
Article36. Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril. 2003; 79:829–843. PMID: 12749418.
Article37. Du Plessis SS, Agarwal A, Halabi J, Tvrda E. Contemporary evidence on the physiological role of reactive oxygen species in human sperm function. J Assist Reprod Genet. 2015; 32:509–520. PMID: 25646893.
Article38. O'Flaherty C. Redox regulation of mammalian sperm capacitation. Asian J Androl. 2015; 17:583–590. PMID: 25926608.39. Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J. The role of oxidative stress and antioxidants in male fertility. Cent European J Urol. 2013; 66:60–67.40. Agarwal A, Cho CL, Esteves SC, Majzoub A. Reactive oxygen species and sperm DNA fragmentation. Transl Androl Urol. 2017; 6:S695–S696. PMID: 29082952.
Article41. Agarwal A, Ikemoto I, Loughlin KR. Relationship of sperm parameters with levels of reactive oxygen species in semen specimens. J Urol. 1994; 152:107–110. PMID: 8201640.
Article42. Menezo Y, Evenson DP, Cohen M, Dale B. Effect of antioxidants on sperm genetic damage. In : Baldi E, Muratori M, editors. Genetic damage in human spermatozoa. New York: Springer;2014. p. 173–189.43. Truong T, Gardner DK. Antioxidants improve IVF outcome and subsequent embryo development in the mouse. Hum Reprod. 2017; 32:2404–2413. PMID: 29136144.
Article44. Bisht S, Faiq M, Tolahunase M, Dada R. Oxidative stress and male infertility. Nat Rev Urol. 2017; 14:470–485. PMID: 28508879.
Article45. Muratori M, Tamburrino L, Marchiani S, Cambi M, Olivito B, Azzari C, et al. Investigation on the origin of sperm DNA fragmentation: role of apoptosis, immaturity and oxidative stress. Mol Med. 2015; 21:109–122. PMID: 25786204.
Article46. Aitken RJ. DNA damage in human spermatozoa; important contributor to mutagenesis in the offspring. Transl Androl Urol. 2017; 6:S761–S764. PMID: 29082208.
Article47. Agarwal A, Allamaneni SS. Free radicals and male reproduction. J Indian Med Assoc. 2011; 109:184–187. PMID: 22010591.48. Tremellen K. Treatment of sperm oxidative stress: a collaborative approach between clinician and embryologist. In : Henkel R, Samanta L, Agarwal A, editors. Oxidants, antioxidants, and impact of the oxidative status in male reproduction. London: Elsevier/Academic Press;2018. p. 225–235.49. Agarwal A, Rana M, Qiu E, AlBunni H, Bui AD, Henkel R. Role of oxidative stress, infection and inflammation in male infertility. Andrologia. 2018; 50:e13126. PMID: 30569652.
Article50. Shekarriz M, Thomas AJ Jr, Agarwal A. Incidence and level of seminal reactive oxygen species in normal men. Urology. 1995; 45:103–107. PMID: 7817460.
Article51. Ochsendorf FR, Thiele J, Fuchs J, Schüttau H, Freisleben HJ, Buslau M, et al. Chemiluminescence in semen of infertile men. Andrologia. 1994; 26:289–293. PMID: 7825744.
Article52. Henkel R, Sandhu IS, Agarwal A. The excessive use of antioxidant therapy: a possible cause of male infertility? Andrologia. 2019; 51:e13162. PMID: 30259539.
Article53. Ross C, Morriss A, Khairy M, Khalaf Y, Braude P, Coomarasamy A, et al. A systematic review of the effect of oral antioxidants on male infertility. Reprod Biomed Online. 2010; 20:711–723. PMID: 20378409.
Article54. Adewoyin M, Ibrahim M, Roszaman R, Isa MLM, Alewi NAM, Rafa AAA, et al. Male infertility: the effect of natural antioxidants and phytocompounds on seminal oxidative stress. Diseases. 2017; 5:E9. PMID: 28933362.
Article55. Dada R, Shamsi MB, Venkatesh S, Gupta NP, Kumar R. Attenuation of oxidative stress & DNA damage in varicocelectomy: implications in infertility management. Indian J Med Res. 2010; 132:728–730. PMID: 21245622.56. Chen SS, Huang WJ, Chang LS, Wei YH. Attenuation of oxidative stress after varicocelectomy in subfertile patients with varicocele. J Urol. 2008; 179:639–642. PMID: 18082213.
Article57. Agarwal A, Gupta S, Sharma R. Reactive oxygen species (ROS) measurement. In : Agarwal A, Gupta S, Sharma R, editors. Andrological evaluation of male infertility: a laboratory guide. Cham: Springer International Publishing;2016. p. 155–163.58. Agarwal A, Roychoudhury S, Sharma R, Gupta S, Majzoub A, Sabanegh E. Diagnostic application of oxidation-reduction potential assay for measurement of oxidative stress: clinical utility in male factor infertility. Reprod Biomed Online. 2017; 34:48–57. PMID: 27839743.
Article59. Agarwal A, Panner Selvam MK, Arafa M, Okada H, Homa S, Killeen A, et al. Multi-center evaluation of oxidation-reduction potential by the MiOXSYS System in males with abnormal semen. Asian J Androl. 2019; In press.60. Ko EY, Sabanegh ES Jr, Agarwal A. Male infertility testing: reactive oxygen species and antioxidant capacity. Fertil Steril. 2014; 102:1518–1527. PMID: 25458618.
Article61. Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988–1989). Hum Reprod. 1991; 6:811–816. PMID: 1757519.62. Agarwal A, Virk G, Ong C, du Plessis SS. Effect of oxidative stress on male reproduction. World J Mens Health. 2014; 32:1–17. PMID: 24872947.
Article63. Jarow J, Sigman M, Kolettis PN, Lipshultz LR, McClure RD, Nangia AK, et al. The optimal evaluation of the infertile male: AUA best practice statement reviewed and validity confirmed 2011. Linthicum: American Urological Association;2011.64. Esteves SC, Sharma RK, Gosálvez J, Agarwal A. A translational medicine appraisal of specialized andrology testing in unexplained male infertility. Int Urol Nephrol. 2014; 46:1037–1052. PMID: 24771472.
Article65. Patel AS, Leong JY, Ramasamy R. Prediction of male infertility by the World Health Organization laboratory manual for assessment of semen analysis: a systematic review. Arab J Urol. 2017; 16:96–102. PMID: 29713540.
Article66. Wang C, Swerdloff RS. Limitations of semen analysis as a test of male fertility and anticipated needs from newer tests. Fertil Steril. 2014; 102:1502–1507. PMID: 25458617.
Article67. Esteves SC, Zini A, Aziz N, Alvarez JG, Sabanegh ES Jr, Agarwal A. Critical appraisal of World Health Organization's new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology. 2012; 79:16–22. PMID: 22070891.
Article68. Bonde JP, Ernst E, Jensen TK, Hjollund NH, Kolstad H, Henriksen TB, et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet. 1998; 352:1172–1177. PMID: 9777833.
Article69. Agarwal A, Sharma R, Roychoudhury S, Du Plessis S, Sabanegh E. MiOXSYS: a novel method of measuring oxidation reduction potential in semen and seminal plasma. Fertil Steril. 2016; 106:566–573.e10. PMID: 27260688.
Article70. Samanta L, Agarwal A, Swain N, Sharma R, Gopalan B, Esteves SC, et al. Proteomic signatures of sperm mitochondria in varicocele: clinical use as biomarkers of varicocele associated infertility. J Urol. 2018; 200:414–422. PMID: 29530785.
Article71. Arafa M, Agarwal A, Al Said S, Majzoub A, Sharma R, Bjugstad KB, et al. Semen quality and infertility status can be identified through measures of oxidation-reduction potential. Andrologia. 2018; 50:e12881.
Article72. Homa ST, Vassiliou AM, Stone J, Killeen AP, Dawkins A, Xie J, et al. A comparison between two assays for measuring seminal oxidative stress and their relationship with sperm DNA fragmentation and semen parameters. Genes (Basel). 2019; 10:E236. PMID: 30893955.
Article73. Okouchi S, Suzuki M, Sugano K, Kagamimori S, Ikeda S. Water desirable for the human body in terms of oxidation-reduction potential (ORP) to pH relationship. J Food Sci. 2002; 67:1594–1598.
Article74. Grotto D, Santa Maria LD, Boeira S, Valentini J, Charão MF, Moro AM, et al. Rapid quantification of malondialdehyde in plasma by high performance liquid chromatography-visible detection. J Pharm Biomed Anal. 2007; 43:619–624. PMID: 16949242.
Article75. Vessey W, Perez-Miranda A, Macfarquhar R, Agarwal A, Homa S. Reactive oxygen species in human semen: validation and qualification of a chemiluminescence assay. Fertil Steril. 2014; 102:1576–1583.e4. PMID: 25439800.
Article76. Agarwal A, Roychoudhury S, Bjugstad KB, Cho CL. Oxidation-reduction potential of semen: what is its role in the treatment of male infertility? Ther Adv Urol. 2016; 8:302–318. PMID: 27695529.
Article77. Agarwal A, Qiu E, Sharma R. Laboratory assessment of oxidative stress in semen. Arab J Urol. 2017; 16:77–86. PMID: 29713538.
Article78. Agarwal A, Wang SM. Clinical relevance of oxidation-reduction potential in the evaluation of male infertility. Urology. 2017; 104:84–89. PMID: 28214572.
Article79. Agarwal A, Arafa MM, Elbardisi H, Majzoub A, Alsaid SS. Relationship between seminal oxidation reduction potential and sperm DNA fragmentation in infertile men. Fertil Steril. 2017; 108:e316.
Article80. Agarwal A, Gupta S, Sharma R. Oxidation-reduction potential measurement in ejaculated semen samples. In : Agarwal A, Gupta S, Sharma R, editors. Andrological evaluation of male infertility: a laboratory guide. Cham: Springer International Publishing;2016. p. 165–170.81. Majzoub A, Arafa M, Mahdi M, Agarwal A, Al Said S, Al-Emadi I, et al. Oxidation-reduction potential and sperm DNA fragmentation, and their associations with sperm morphological anomalies amongst fertile and infertile men. Arab J Urol. 2018; 16:87–95. PMID: 29713539.
Article82. Ko EY, Siddiqi K, Brannigan RE, Sabanegh ES Jr. Empirical medical therapy for idiopathic male infertility: a survey of the American Urological Association. J Urol. 2012; 187:973–978. PMID: 22264467.
Article83. Kim HH, Schlegel PN. Endocrine manipulation in male infertility. Urol Clin North Am. 2008; 35:303–318. PMID: 18423250.
Article84. Jung JH, Seo JT. Empirical medical therapy in idiopathic male infertility: promise or panacea? Clin Exp Reprod Med. 2014; 41:108–114. PMID: 25309854.
Article85. Tadros NN, Sabanegh ES. Empiric medical therapy with hormonal agents for idiopathic male infertility. Indian J Urol. 2017; 33:194–198. PMID: 28717268.
Article86. Nieschlag E, Kamischke A. Empirical therapies for idiopathic male infertility. In : Nieschlag E, Behre HM, Nieschlag S, editors. Andrology: male reproductive health and dysfunction. Berlin, Heidelberg: Springer Berlin Heidelberg;2010. p. 457–467.87. Attia AM, Abou-Setta AM, Al-Inany HG. Gonadotrophins for idiopathic male factor subfertility. Cochrane Database Syst Rev. 2013; CD005071. PMID: 23970458.
Article88. Kumar R, Gautam G, Gupta NP. Drug therapy for idiopathic male infertility: rationale versus evidence. J Urol. 2006; 176:1307–1312. PMID: 16952617.
Article89. Clark RV, Sherins RJ. Treatment of men with idiopathic oligozoospermic infertility using the aromatase inhibitor, testolactone. Results of a double-blinded, randomized, placebocontrolled trial with crossover. J Androl. 1989; 10:240–247. PMID: 2663800.
Article90. Siddiq FM, Sigman M. A new look at the medical management of infertility. Urol Clin North Am. 2002; 29:949–963. PMID: 12516764.
Article91. Mirończuk-Chodakowska I, Witkowska AM, Zujko ME. Endogenous non-enzymatic antioxidants in the human body. Adv Med Sci. 2018; 63:68–78. PMID: 28822266.92. Halliwell B, Gutteridge JMC. Antioxidant defences synthesized in vivo. In : Halliwell B, Gutteridge JMC, editors. Free radicals in biology and medicine. 5th ed. Oxford: Oxford University Press;2015.93. Majzoub A, Agarwal A. Antioxidant therapy in idiopathic oligoasthenoteratozoospermia. Indian J Urol. 2017; 33:207–214. PMID: 28717270.
Article94. Hsieh YY, Sun YL, Chang CC, Lee YS, Tsai HD, Lin CS. Superoxide dismutase activities of spermatozoa and seminal plasma are not correlated with male infertility. J Clin Lab Anal. 2002; 16:127–131. PMID: 11968048.
Article95. Kobayashi T, Miyazaki T, Natori M, Nozawa S. Protective role of superoxide dismutase in human sperm motility: superoxide dismutase activity and lipid peroxide in human seminal plasma and spermatozoa. Hum Reprod. 1991; 6:987–991. PMID: 1761671.96. Ben Abdallah F, Dammak I, Attia H, Hentati B, Ammar-Keskes L. Lipid peroxidation and antioxidant enzyme activities in infertile men: correlation with semen parameter. J Clin Lab Anal. 2009; 23:99–104. PMID: 19288454.
Article97. Lenzi A, Lombardo F, Gandini L, Culasso F, Dondero F. Glutathione therapy for male infertility. Arch Androl. 1992; 29:65–68. PMID: 1503526.
Article98. Lenzi A, Culasso F, Gandini L, Lombardo F, Dondero F. Placebo-controlled, double-blind, cross-over trial of glutathione therapy in male infertility. Hum Reprod. 1993; 8:1657–1662. PMID: 8300824.99. Atig F, Raffa M, Habib BA, Kerkeni A, Saad A, Ajina M. Impact of seminal trace element and glutathione levels on semen quality of Tunisian infertile men. BMC Urol. 2012; 12:6. PMID: 22429816.
Article100. Dawson EB, Harris WA, Rankin WE, Charpentier LA, Mc-Ganity WJ. Effect of ascorbic acid on male fertility. Ann N Y Acad Sci. 1987; 498:312–323. PMID: 3476000.
Article101. Akmal M, Qadri JQ, Al-Waili NS, Thangal S, Haq A, Saloom KY. Improvement in human semen quality after oral supplementation of vitamin C. J Med Food. 2006; 9:440–442. PMID: 17004914.
Article102. Suleiman AA, Alboqai OK, Yasein N, Al-Essa MK, El Masri K. Prevalence of vitamin-mineral supplement use among Jordan University students. Saudi Med J. 2008; 29:1326–1331. PMID: 18813421.103. Kessopoulou E, Powers HJ, Sharma KK, Pearson MJ, Russell JM, Cooke ID, et al. A double-blind randomized placebo cross-over controlled trial using the antioxidant vitamin E to treat reactive oxygen species associated male infertility. Fertil Steril. 1995; 64:825–831. PMID: 7672157.
Article104. Nadjarzadeh A, Shidfar F, Amirjannati N, Vafa MR, Motevalian SA, Gohari MR, et al. Effect of coenzyme Q10 supplementation on antioxidant enzymes activity and oxidative stress of seminal plasma: a double-blind randomised clinical trial. Andrologia. 2014; 46:177–183. PMID: 23289958.
Article105. Tvrda E, Peer R, Sikka SC, Agarwal A. Iron and copper in male reproduction: a double-edged sword. J Assist Reprod Genet. 2015; 32:3–16. PMID: 25245929.
Article106. Zhao J, Dong X, Hu X, Long Z, Wang L, Liu Q, et al. Zinc levels in seminal plasma and their correlation with male infertility: a systematic review and meta-analysis. Sci Rep. 2016; 6:22386. PMID: 26932683.
Article107. Ahsan U, Kamran Z, Raza I, Ahmad S, Babar W, Riaz MH, et al. Role of selenium in male reproduction: a review. Anim Reprod Sci. 2014; 146:55–62. PMID: 24613013.108. Ciftci H, Verit A, Savas M, Yeni E, Erel O. Effects of N-acetylcysteine on semen parameters and oxidative/antioxidant status. Urology. 2009; 74:73–76. PMID: 19428083.
Article109. Oeda T, Henkel R, Ohmori H, Schill WB. Scavenging effect of N-acetyl-L-cysteine against reactive oxygen species in human semen: a possible therapeutic modality for male factor infertility? Andrologia. 1997; 29:125–131. PMID: 9197915.
Article110. Stanislavov R, Rohdewald P. Sperm quality in men is improved by supplementation with a combination of L-arginine, L-citrullin, roburins and Pycnogenol®. Minerva Urol Nefrol. 2014; 66:217–223. PMID: 25531191.111. Wong WY, Merkus HM, Thomas CM, Menkveld R, Zielhuis GA, Steegers-Theunissen RP. Effects of folic acid and zinc sulfate on male factor subfertility: a double-blind, randomized, placebo-controlled trial. Fertil Steril. 2002; 77:491–498. PMID: 11872201.
Article112. Castagné V, Lefèvre K, Natero R, Clarke PG, Bedker DA. An optimal redox status for the survival of axotomized ganglion cells in the developing retina. Neuroscience. 1999; 93:313–320. PMID: 10430495.
Article113. Busetto GM, Agarwal A, Virmani A, Antonini G, Ragonesi G, Del Giudice F, et al. Effect of metabolic and antioxidant supplementation on sperm parameters in oligo-asthenoteratozoospermia, with and without varicocele: a double-blind placebo-controlled study. Andrologia. 2018; 150.
Article114. Safarinejad MR. Efficacy of coenzyme Q10 on semen parameters, sperm function and reproductive hormones in infertile men. J Urol. 2009; 182:237–248. PMID: 19447425.
Article115. Balercia G, Regoli F, Armeni T, Koverech A, Mantero F, Boscaro M. Placebo-controlled double-blind randomized trial on the use of L-carnitine, L-acetylcarnitine, or combined L-carnitine and L-acetylcarnitine in men with idiopathic asthenozoospermia. Fertil Steril. 2005; 84:662–671. PMID: 16169400.
Article116. Safarinejad MR, Safarinejad S, Shafiei N, Safarinejad S. Effects of the reduced form of coenzyme Q10 (ubiquinol) on semen parameters in men with idiopathic infertility: a double-blind, placebo controlled, randomized study. J Urol. 2012; 188:526–531. PMID: 22704112.117. ElSheikh MG, Hosny MB, Elshenoufy A, Elghamrawi H, Fayad A, Abdelrahman S. Combination of vitamin E and clomiphene citrate in treating patients with idiopathic oligoasthenozoospermia: a prospective, randomized trial. Andrology. 2015; 3:864–867. PMID: 26235968.
Article118. Majzoub A, Agarwal A, Esteves SC. Antioxidants for elevated sperm DNA fragmentation: a mini review. Transl Androl Urol. 2017; 6:S649–S653. PMID: 29082954.
Article119. Micic S, Lalic N, Djordjevic D, Bojanic N, Bogavac-Stanojevic N, Busetto GM, et al. Double-blind, randomised, placebo-controlled trial on the effect of L-carnitine and L-acetylcarnitine on sperm parameters in men with idiopathic oligoasthenozoospermia. Andrologia. 2019; e13267. DOI: 10.1111/and.13267. PMID: 30873633.
Article120. Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, Amoroso S, et al. Coenzyme Q10 treatment in infertile men with idiopathic asthenozoospermia: a placebo-controlled, double-blind randomized trial. Fertil Steril. 2009; 91:1785–1792. PMID: 18395716.
Article121. Tunc O, Thompson J, Tremellen K. Improvement in sperm DNA quality using an oral antioxidant therapy. Reprod Biomed Online. 2009; 18:761–768. PMID: 19490779.
Article122. Tremellen K, Miari G, Froiland D, Thompson J. A randomised control trial examining the effect of an antioxidant (Menevit) on pregnancy outcome during IVF-ICSI treatment. Aust N Z J Obstet Gynaecol. 2007; 47:216–221. PMID: 17550489.
Article123. Imamovic Kumalic S, Pinter B. Review of clinical trials on effects of oral antioxidants on basic semen and other parameters in idiopathic oligoasthenoteratozoospermia. Biomed Res Int. 2014; 2014:426951. PMID: 24800224.
Article124. Lampiao F. Free radicals generation in an in vitro fertilization setting and how to minimize them. World J Obstet Gynecol. 2012; 1:29–34.125. Bedaiwy MA, Falcone T, Mohamed MS, Aleem AA, Sharma RK, Worley SE, et al. Differential growth of human embryos in vitro: role of reactive oxygen species. Fertil Steril. 2004; 82:593–600. PMID: 15374701.
Article126. Showell MG, Mackenzie-Proctor R, Brown J, Yazdani A, Stankiewicz MT, Hart RJ. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2014; CD007411. PMID: 25504418.
Article127. Mora-Esteves C, Shin D. Nutrient supplementation: improving male fertility fourfold. Semin Reprod Med. 2013; 31:293–300. PMID: 23775385.
Article128. Gil-Villa AM, Cardona-Maya W, Agarwal A, Sharma R, Cadavid A. Role of male factor in early recurrent embryo loss: do antioxidants have any effect? Fertil Steril. 2009; 92:565–571. PMID: 18829003.
Article129. Calogero AE, Duca Y, Condorelli RA, La Vignera S. Male accessory gland inflammation, infertility, and sexual dysfunctions: a practical approach to diagnosis and therapy. Andrology. 2017; 5:1064–1072. PMID: 28992374.
Article130. La Vignera S, Vicari E, Condorelli RA, D'Agata R, Calogero AE. Male accessory gland infection and sperm parameters (review). Int J Androl. 2011; 34:e330–e347. PMID: 21696400.
Article131. Colpi GM, Francavilla S, Haidl G, Link K, Behre HM, Goulis DG, et al. European Academy of Andrology guideline Management of oligo-astheno-teratozoospermia. Andrology. 2018; 6:513–524. PMID: 30134082.
Article132. Haidl G, Haidl F, Allam JP, Schuppe HC. Therapeutic options in male genital tract inflammation. Andrologia. 2019; 51:e13207. PMID: 30474250.
Article133. Barratt CLR, Björndahl L, De Jonge CJ, Lamb DJ, Osorio Martini F, McLachlan R, et al. The diagnosis of male infertility: an analysis of the evidence to support the development of global WHO guidance-challenges and future research opportunities. Hum Reprod Update. 2017; 23:660–680. PMID: 28981651.
Article134. Atik RB, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S, et al. ESHRE guideline: recurrent pregnancy loss. Hum Reprod Open. 2018; DOI: 10.1093/hropen/hoy002.135. Henkel RR. Leukocytes and oxidative stress: dilemma for sperm function and male fertility. Asian J Androl. 2011; 13:43–52. PMID: 21076433.
Article136. Gutteridge JM, Halliwell B. Antioxidants: molecules, medicines, and myths. Biochem Biophys Res Commun. 2010; 393:561–564. PMID: 20171167.
Article137. Pérez-Torres I, Guarner-Lans V, Rubio-Ruiz ME. Reductive stress in inflammation-associated diseases and the prooxidant effect of antioxidant agents. Int J Mol Sci. 2017; 18:E2098. PMID: 28981461.
Article138. Ufer C, Wang CC, Borchert A, Heydeck D, Kuhn H. Redox control in mammalian embryo development. Antioxid Redox Signal. 2010; 13:833–875. PMID: 20367257.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oxidative Stress: A Comprehensive Review of Biochemical, Molecular, and Genetic Aspects in the Pathogenesis and Management of Varicocele
- A Schematic Overview of the Current Status of Male Infertility Practice
- The effects of oral antioxidants on the semen of men with idiopathic oligoasthenoteratozoospermia
- Genetic Causes in Male Infertility and Current Studies on Infertility Genes
- Oxidation-reduction potential as a new marker for oxidative stress: Correlation to male infertility