J Korean Med Assoc.
2019 Aug;62(8):437-456. 10.5124/jkma.2019.62.8.437.
Status of common parasitic diseases in Korea in 2019
- Affiliations
-
- 1Department of Parasitology and Institute of Medical Education, College of Medicine, Hallym University, Chuncheon, Korea. shuh@hallym.ac.kr
- KMID: 2455380
- DOI: http://doi.org/10.5124/jkma.2019.62.8.437
Abstract
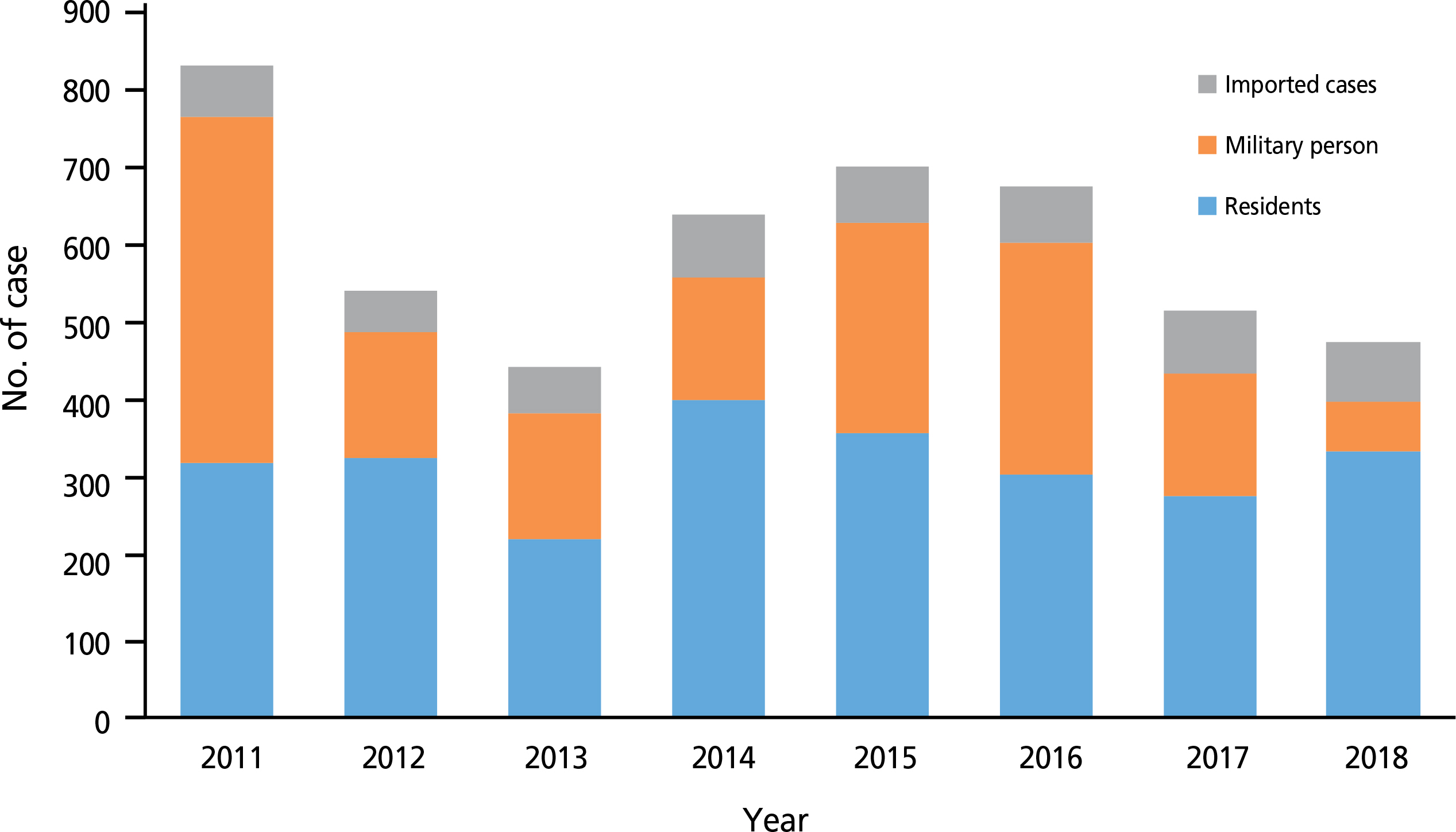
- This study aimed to determine the status of common parasitic disease in Korea in 2019. Twelve parasitic diseases were selected: toxocariasis, anisakiasis, paragonimiasis, sparganosis, cysticercosis, toxoplasmosis, clonorchiasis, enterobiasis, trichuriasis, trichomoniasis, cryptosporidiosis, and malaria. Their biology, epidemiology, pathogenesis, symptoms and signs, diagnosis, treatment, and prognosis were evaluated. Of the parasitic diseases, toxocariasis was the most prevalent according to serological results. Anisakiasis should be considered when acute gastrointestinal symptoms occur with a recent past history of raw seafood ingestion. Paragonimiasis, sparganosis, and cysticercosis can be diagnosed using an enzyme-linked immunosorbent assay; thus, enzyme-linked immunosorbent assay needs to be performed for suspected cases. Toxoplasmosis and cryptosporidiosis are opportunistic infections. The symptoms and signs are aggravated under immunocompromised conditions. Although the egg positivity rate of Clonorchis sinensis is higher than that of other intestinal parasitic diseases, encountering patients with complaints of symptoms caused by clonorchiasis is rare because the worm burden is low. Trichomoniasis is usually managed by gynecologists; therefore, it should be included in the differential diagnoses of vaginal diseases. The annual number of malaria cases has decreased, although it remains at approximately 500 cases per year. Malaria should be suspected when symptoms such as intermittent fever, headache, and splenomegaly are noted especially when the patients reside near demilitarized zones. Although the prevalence and number of reported cases of parasitic diseases have decreased in Korea, we should consider parasitic diseases in the list of differential diagnoses.
MeSH Terms
-
Animals
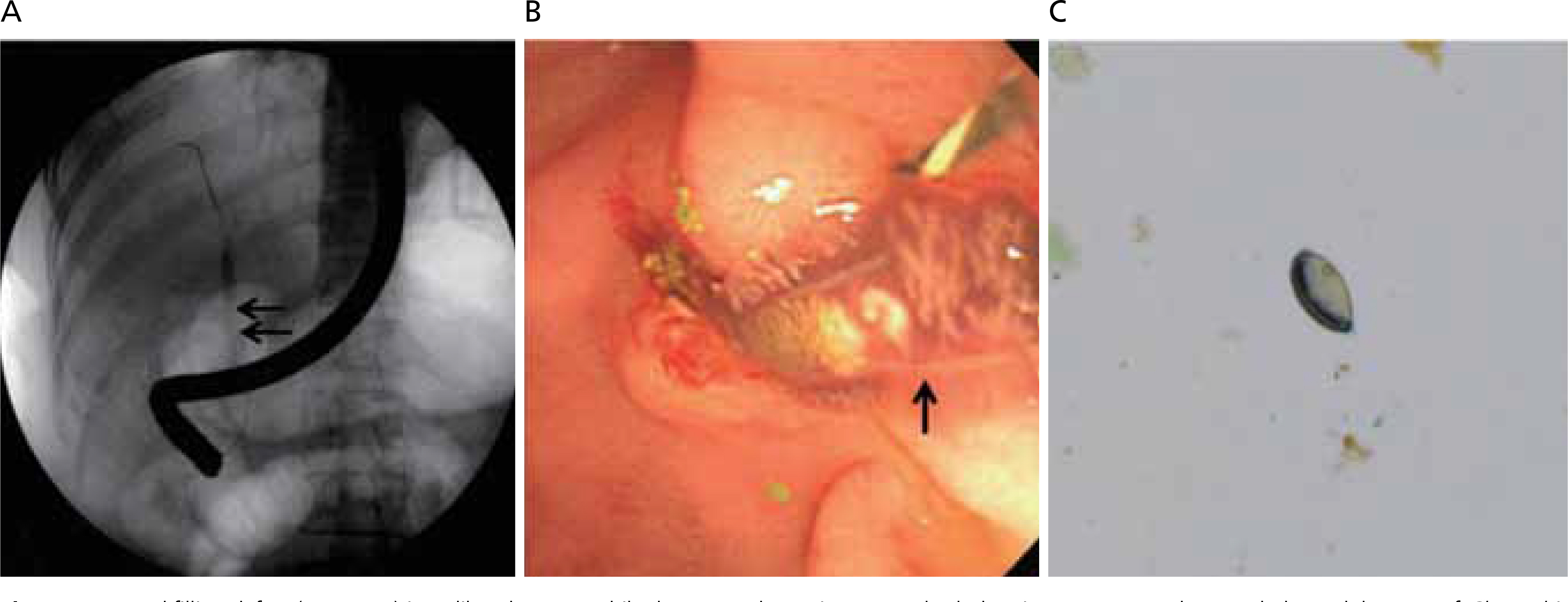
Anisakiasis
Biology
Clonorchiasis
Clonorchis sinensis
Cryptosporidiosis
Cysticercosis
Diagnosis
Diagnosis, Differential
Eating
Enterobiasis
Enzyme-Linked Immunosorbent Assay
Epidemiology
Fever
Headache
Humans
Korea*
Malaria
Opportunistic Infections
Ovum
Paragonimiasis
Parasitic Diseases*
Prevalence
Prognosis
Republic of Korea
Seafood
Sparganosis
Splenomegaly
Toxocariasis
Toxoplasmosis
Trichuriasis
Vaginal Diseases
Figure
Reference
-
1. Choi EJ. Anisakis worm from the school lunch meal in Incheon, Korea. Yonhap News. 2019 Jun 24. [cited 2019 Jul 25]. Available from:. https://www.yna.co.kr/view/AKR20190624169200065.2. Cho SH, Jeong BS, Lee SE. National survey of intestinal parasitic infections in Korea, 8th report (2013) [Internet]. Cheongju: Korea Centers for Disease Control and Prevention [cited 2019 Jul 25]. Available from:. http://www.cdc.go.kr/CDC/cms/content/mobile/52/24152_view.html.3. Korea Centers for Disease Control and Prevention. Infectious disease portal [Internet]. Cheongju: Korea Centers for Disease Control and Prevention [cited 2019 Jul 25]. Available from:. http://www.cdc.go.kr/npt/biz/npp/nppMain.do.4. Bahk YY, Park YK, Na BK, Sohn WM, Hong SJ, Chai JY, Kim TS. Survey on intestinal helminthic infection status of students in two counties, Hadong-gun and Goseong-gun, Korea. Korean J Parasitol. 2018; 56:335–339.
Article5. Cheun HI, Shin HE, Ma DW, Hong SH, Kim TY, Lee SE, Ju J, Park YK, Kim TS, Cho SH. Follow-up study of patients previously diagnosed with lymphatic filariasis in Korea. Osong Public Health Res Perspect. 2017; 8:421–424.
Article6. Kim C, June KJ, Cho SH, Park KS, Lee HS, Park JY. Prevalence and related factors of Clonorchiasis among five major river-sideresidents in South Korea. J Korean Acad Community Health Nurs. 2016; 27:346–357.7. Goo YK, Shin WS, Yang HW, Joo SY, Song SM, Ryu JS, Lee WM, Kong HH, Lee WK, Lee SE, Lee WJ, Chung DI, Hong Y. Prevalence of Trichomonas vaginalis in women visiting 2 Obstetrics and Gynecology Clinics in Daegu, South Korea. Korean J Parasitol. 2016; 54:75–80.8. Kim YE, Huh HJ, Hwang YY, Lee NY. A survey of intestinal parasite infection during a 10-year period (2003-2012). Ann Clin Microbiol. 2013; 16:134–139.
Article9. Park HY, Lee SU, Huh S, Kong Y, Magnaval JF. A seroepide-miological survey for toxocariasis in apparently healthy residents in Gangwon-do, Korea. Korean J Parasitol. 2002; 40:113–117.
Article10. Kim HS, Jin Y, Choi MH, Kim JH, Lee YH, Yoon CH, Hwang EH, Kang H, Ahn SY, Kim GJ, Hong ST. Significance of serum antibody test for toxocariasis in healthy healthcare examinees with eosinophilia in Seoul and Gyeongsangnam-do, Korea. J Korean Med Sci. 2014; 29:1618–1625.
Article11. Kim YH, Huh S, Chung YB. Seroprevalence of yoxocariasis among healthy people with eosinophilia. Korean J Parasitol. 2008; 46:29–32.12. Huh S. Toxocariasis [Internet]. New York: Medscape;2016. [cited 2019 Jul 27]. Available from:. https://emedicine.medscape.com/article/229855-overview.13. Kwon HH. Toxocariasis: a rare cause of multiple cerebral infarction. Infect Chemother. 2015; 47:137–141.
Article14. Kim SH, Park CW, Kim SK, Won S, Park WK, Kim HR, Nam KW, Lee GS. A case of anisakiasis invading the stomach and the colon at the same time after eating anchovies. Clin Endosc. 2013; 46:293–296.
Article15. Song H, Jung BK, Cho J, Chang T, Huh S, Chai JY. Molecular identification of Anisakis larvae extracted by gastrointestinal endoscopy from health check-up patients in Korea. Korean J Parasitol. 2019; 57:207–211.
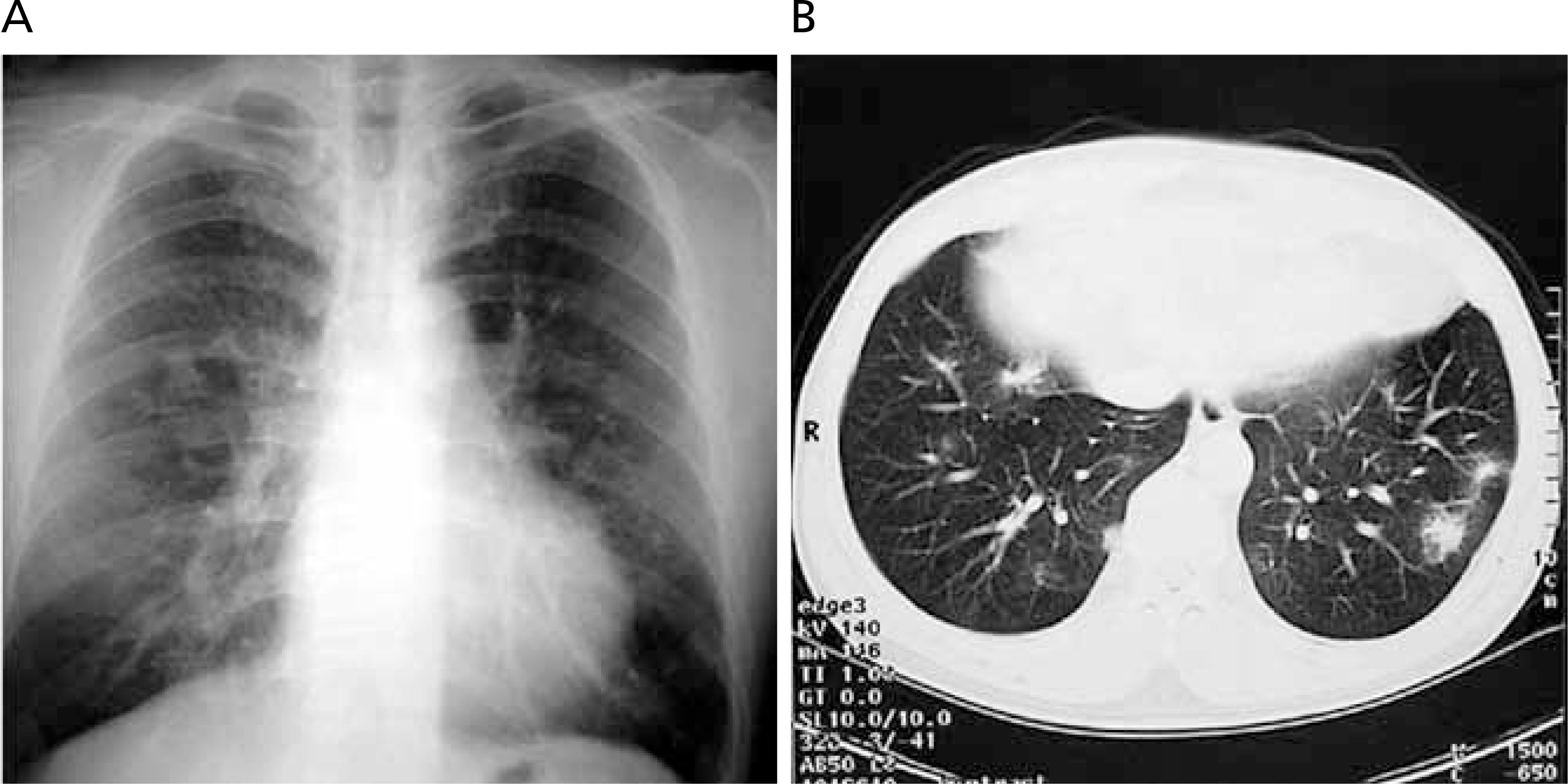
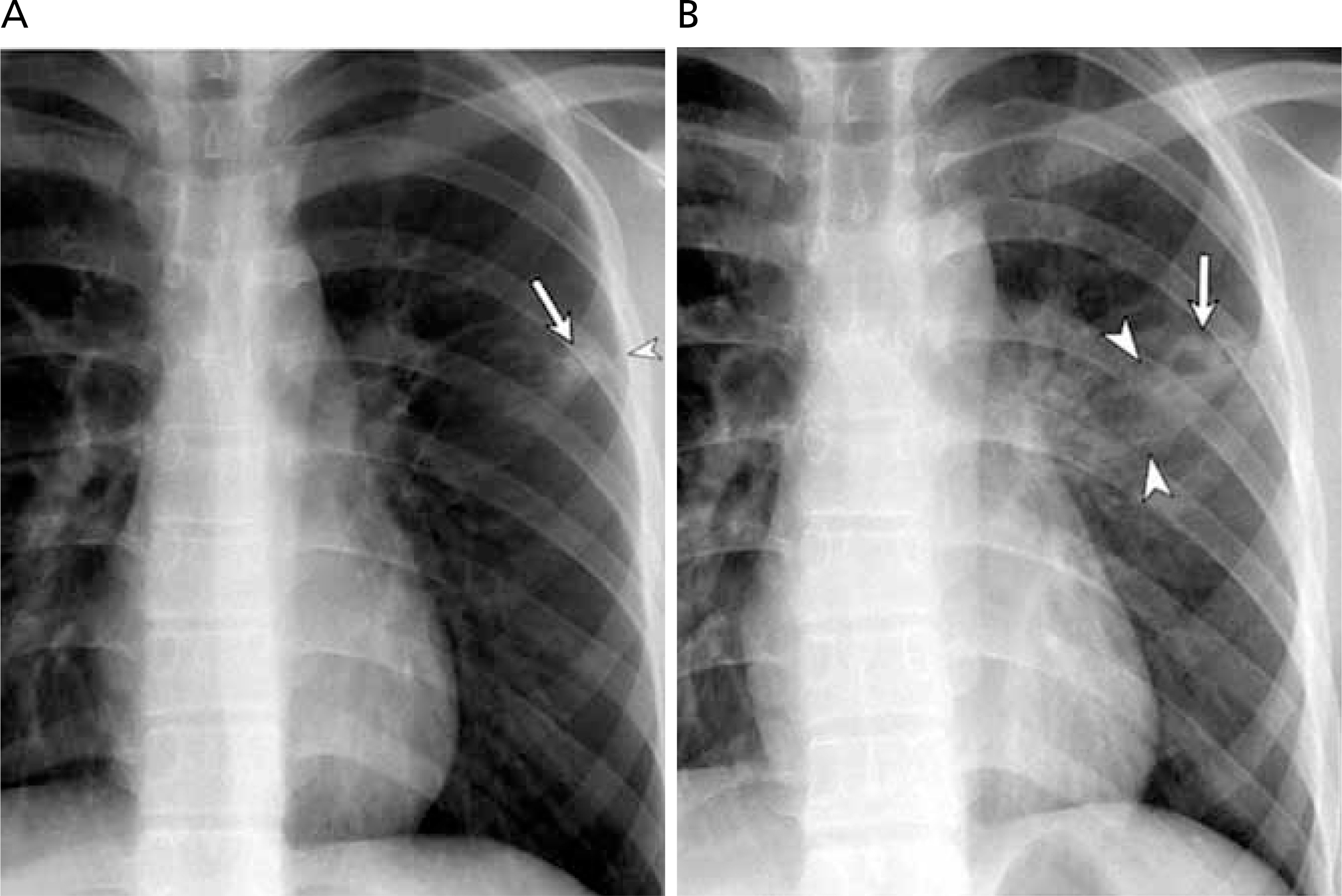
Article16. Sohn WM, Na BK, Kim TH, Park TJ. Anisakiasis: report of 15 gastric cases caused by Anisakis type I larvae and a brief review of Korean anisakiasis cases. Korean J Parasitol. 2015; 53:465–470.17. Park SE, Song B, Hwang JY. Pulmonary paragonimiasis misdiagnosed with pulmonary tuberculosis. Pediatr Infect Vaccine. 2017; 24:178–182.
Article18. Lee MK, Hong SJ, Kim HR. Seroprevalence of tissue invading parasitic infections diagnosed by ELISA in Korea. J Korean Med Sci. 2010; 25:1272–1276.
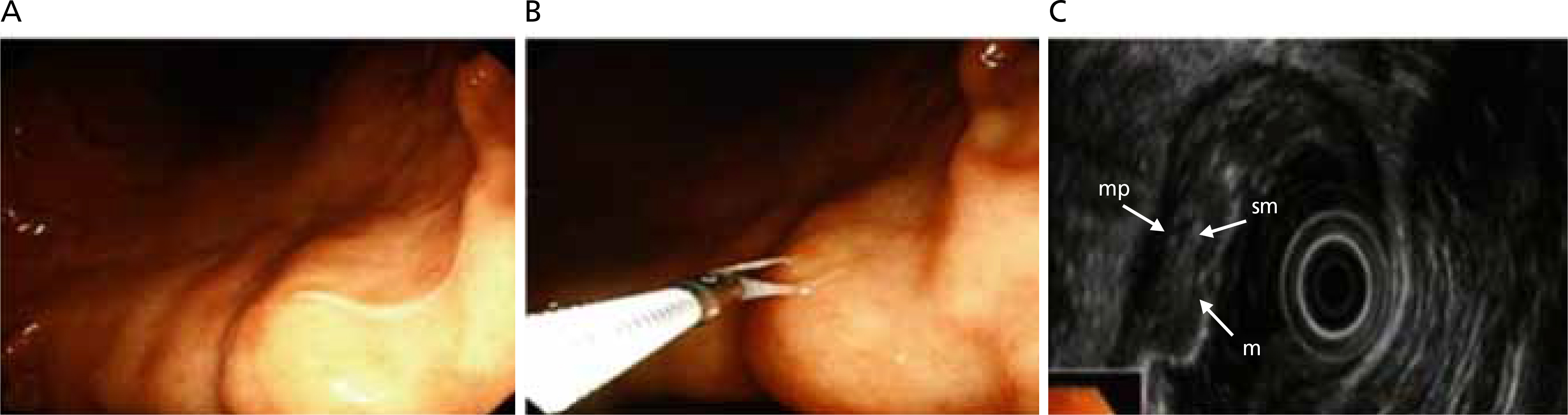
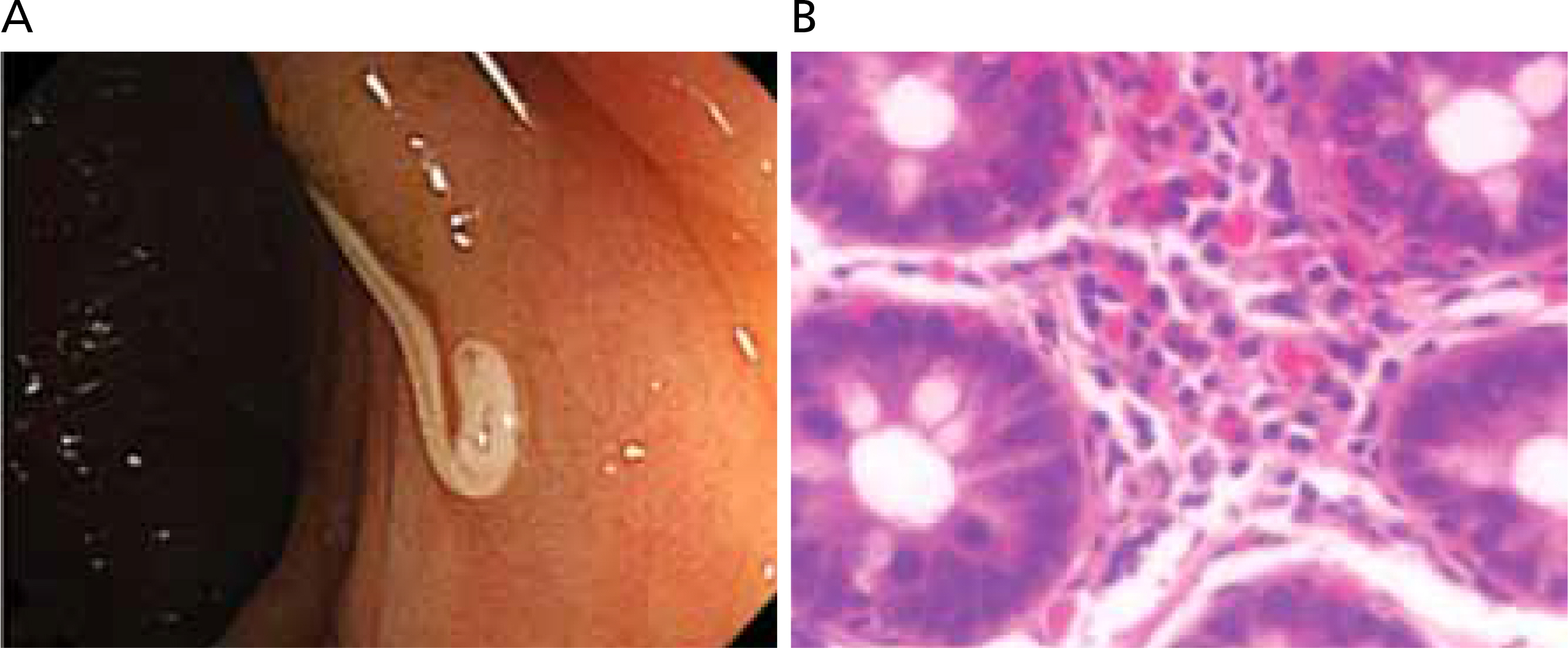
Article19. Seok H, Sohn TS, Peck KR. A Paragonimiasis mimicking gastric submucosal tumor. J Korean Med Sci. 2019; 34:e45.
Article20. Kim JY, Park MK, Lee YJ, Huh S, Cho KY. A case of pulmonary paragonimiasis with chronic abdominal pain and erythematous rash in a 6-year-old girl. Pediatr Infect Vaccine. 2018; 25:54–59.
Article21. Oh CR, Kim MJ, Lee KH. A case of intra-abdominal paragonimiasis mimicking metastasis of lung cancer diagnosed by endoscopic ultrasound-guided fine needle aspiration. Korean J Gastroenterol. 2015; 66:41–45.
Article22. Jeon KN, Park MJ, Bae K, Choi HY, Choi HC, Na JB, Choi DS, Kim HC, Jang IS, Kim DC. Paragonimiasis: a pictorial essay. J Korean Soc Radiol. 2013; 69:365–371.
Article23. Oh MY, Kim KE, Kim MJ, Chu A, Lee JY, Park JH, Kim J, Hwang KT. Breast sparganosis presenting with a painless breast lump: report of two cases. Korean J Parasitol. 2019; 57:179–184.
Article24. Kim JG, Ahn CS, Sohn WM, Nawa Y, Kong Y. Human sparganosis in Korea. J Korean Med Sci. 2018; 33:e273.
Article25. Jeong YH, Lee YS, Eun DC, Byun CW. Intradural extramedullary cysticercosis involving the thoracolumbar spinal canal in a patient with cerebral cysticercosis. J Korean Orthop Assoc. 2018; 53:369–373.
Article26. Ahn CS, Kim JG, Huh S, Kang I, Kong Y. Advances in serological diagnosis of Taenia solium neurocysticercosis in Korea. Genomics Inform. 2019; 17:e7.
Article27. Chai JY. Praziquantel treatment in trematode and cestode infections: an update. Infect Chemother. 2013; 45:32–43.
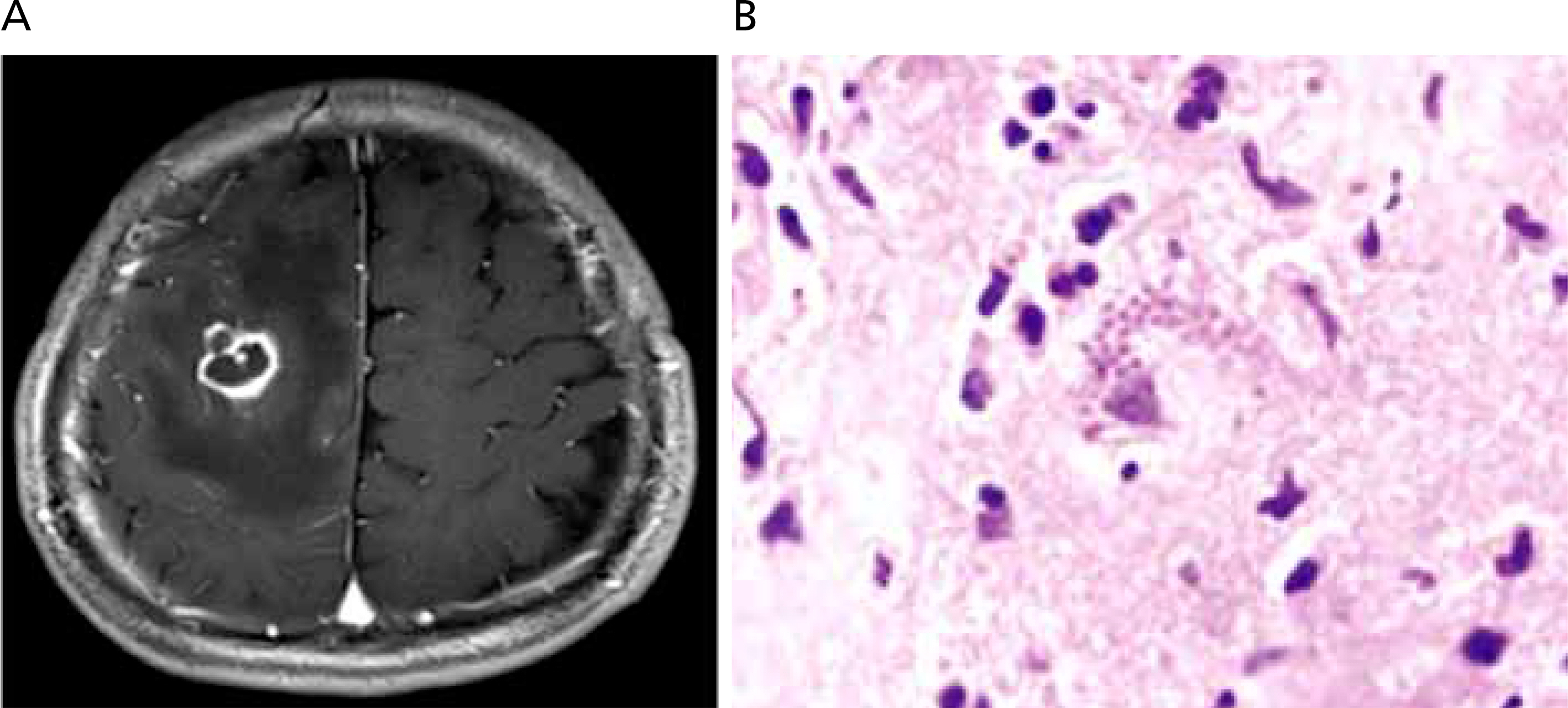
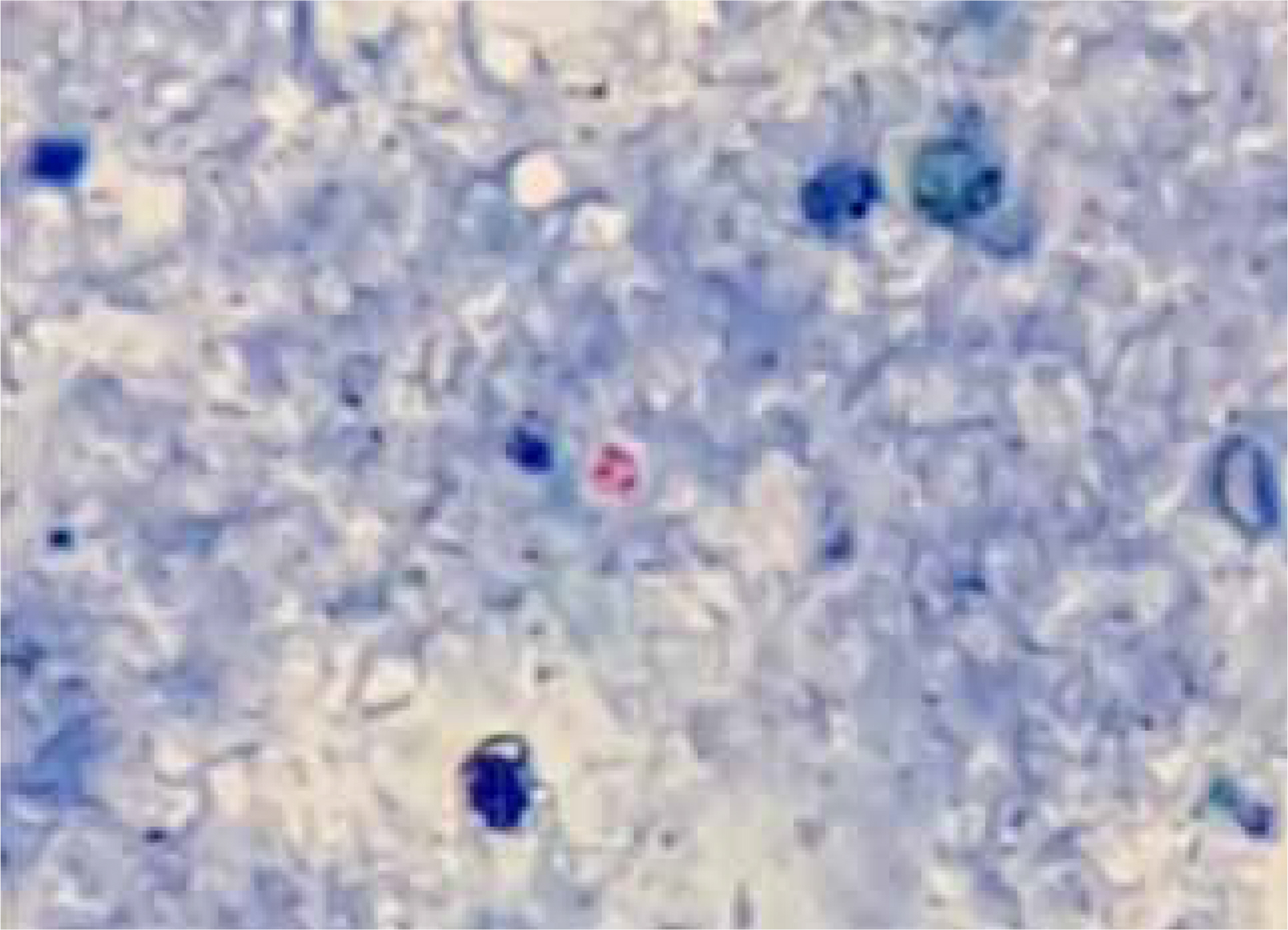
Article28. Lee SB, Lee TG. Toxoplasmic encephalitis in patient with acquired immunodeficiency syndrome. Brain Tumor Res Treat. 2017; 5:34–36.
Article29. Song KJ, Shin JC, Shin HJ, Nam HW. Seroprevalence of toxoplasmosis in Korean pregnant women. Korean J Parasitol. 2005; 43:69–71.
Article30. Yang Z, Cho PY, Ahn SK, Ahn HJ, Kim TS, Chong CK, Hong SJ, Cha SH, Nam HW. A surge in the seroprevalence of toxoplasmosis among the residents of islands in Gangwha-gun, Incheon, Korea. Korean J Parasitol. 2012; 50:191–197.
Article31. Lim H, Lee SE, Jung BK, Kim MK, Lee MY, Nam HW, Shin JG, Yun CH, Cho HI, Shin EH, Chai JY. Serologic survey of toxoplasmosis in Seoul and Jeju-do, and a brief review of its seroprevalence in Korea. Korean J Parasitol. 2012; 50:287–293.
Article32. Kim YH, Lee JH, Ahn SK, Kim TS, Hong SJ, Chong CK, Ahn HJ, Nam HW. Seroprevalence of toxoplasmosis with ELISA and rapid diagnostic test among residents in Gyodong-do, Inchon city, Korea: a four-year followup. Korean J Parasitol. 2017; 55:247–254.
Article33. Lee SE, Kim J, Kim Y, Cho SH, Ahn HJ, Woo HM, Lee WJ, Nam HW. Prevalence of Toxoplasma gondii Infection in stray and household cats in regions of Seoul, Korea. Korean J Parasitol. 2010; 48:267–270.34. Park YH, Nam HW. Clinical features and treatment of ocular toxoplasmosis. Korean J Parasitol. 2013; 51:393–399.
Article35. Yang YM, Choi H, Ryu DH, Woo CG, Han JH, Park SM. Clonorchis sinensis Infection presenting as acute cholangitis and acute cholecystitis. Korean J Pancreas Biliary Tract. 2019; 24:79–83.
Article36. Huh S. Chemotherapeutic drugs for common parasitic diseases in Korea. J Korean Med Assoc. 2013; 56:513–522.
Article37. Huh S. Parasitic diseases in children. J Korean Med Assoc. 2004; 47:512–520.
Article38. Kim DH, Cho MK, Park MK, Kang SA, Kim BY, Park SK, Yu HS. Environmental factors related to enterobiasis in a southeast region of Korea. Korean J Parasitol. 2013; 51:139–142.
Article39. Kim DH, Son HM, Lee SH, Park MK, Kang SA, Park SK, Choi JH, Park JH, Yu HS. Detection of head lice among orphanage children in Busan and Ulsan, Korea (2014). Korean J Parasitol. 2015; 53:497–499.40. Huh S. Pinworm (Enterobiasis) [Internet]. New York: Medscape;2019. [cited 2019 Jul 27]. Available from:. https://emedicine.medscape.com/article/225652-overview.41. Ok KS, Kim YS, Song JH, Lee JH, Ryu SH, Lee JH, Moon JS, Whang DH, Lee HK. Trichuris trichiura infection diagnosed by colonoscopy: case reports and review of literature. Korean J Parasitol. 2009; 47:275–280.
Article42. Huh S. Is it necessary to take anthelmintics every year in Korea? J Korean Med Assoc. 2018; 61:198–204.
Article43. Hong ST. Albendazole and praziquantel: review and safety monitoring in Korea. Infect Chemother. 2018; 50:1–10.
Article44. Kim YJ, Kim SI, Kim YR, Choi IJ, Lee MD, Park YJ, Nam HW, Kang MW. Cryptosporidiosis in a small bowel transplant recipient. J Korean Soc Transplant. 2008; 22:138–141.45. Sim S, Won J, Kim JW, Kim K, Park WY, Yu JR. Simultaneous molecular detection of Cryptosporidium and Cyclospora from raw vegetables in Korea. Korean J Parasitol. 2017; 55:137–142.
Article46. Seo M, Huh S, Chai JY, Yu JR. An epidemiological survey on Cryptosporidium parvum infection of inhabitants in Chorwon-gun, Kangwon-do. Korean J Parasitol. 2001; 39:201–203.
Article47. Park JH, Kim HJ, Guk SM, Shin EH, Kim JL, Rim HJ, Lee SH, Chai JY. A survey of cryptosporidiosis among 2,541 residents of 25 coastal islands in Jeollanam-Do (Province), Republic of Korea. Korean J Parasitol. 2006; 44:367–372.
Article48. Cheun HI, Cho SH, Lim YY, Lee BC, Kim JY, Ju JW, Na BK, Kimata I, Yu JR, Kim TS. Cryptosporidium parvum in Korea: prevalence in individuals residing in three major river valleys and genetic characteristics of the isolates. J Vet Med Sci. 2010; 72:167–172.
Article49. Moon S, Kwak W, Lee S, Kim W, Oh J, Youn SK. Epidemiological characteristics of the first water-borne outbreak of cryptosporidiosis in Seoul, Korea. J Korean Med Sci. 2013; 28:983–989.
Article50. Kim SR, Kim JH, Gu NY, Kim YS, Hong YC, Ryu JS. Prevalence of trichomoniasis by PCR in women attending health screening in Korea. Korean J Parasitol. 2016; 54:187–190.
Article51. Goo YK, Shin WS, Yang HW, Joo SY, Song SM, Ryu JS, Lee WM, Kong HH, Lee WK, Lee SE, Lee WJ, Chung DI, Hong Y. Prevalence of Trichomonas vaginalis in women visiting 2 obstetrics and gynecology clinics in Daegu, South Korea. Korean J Parasitol. 2016; 54:75–80.52. Seo JH, Yang HW, Joo SY, Song SM, Lee YR, Ryu JS, Yoo ES, Lee WK, Kong HH, Lee SE, Lee WJ, Goo YK, Chung DI, Hong Y. Prevalence of Trichomonas vaginalis by PCR in men attending a primary care urology clinic in South Korea. Korean J Parasitol. 2014; 52:551–555.
Article53. Ryu JS. Trichomoniasis. Hanyang Med Rev. 2010; 30:213–222.
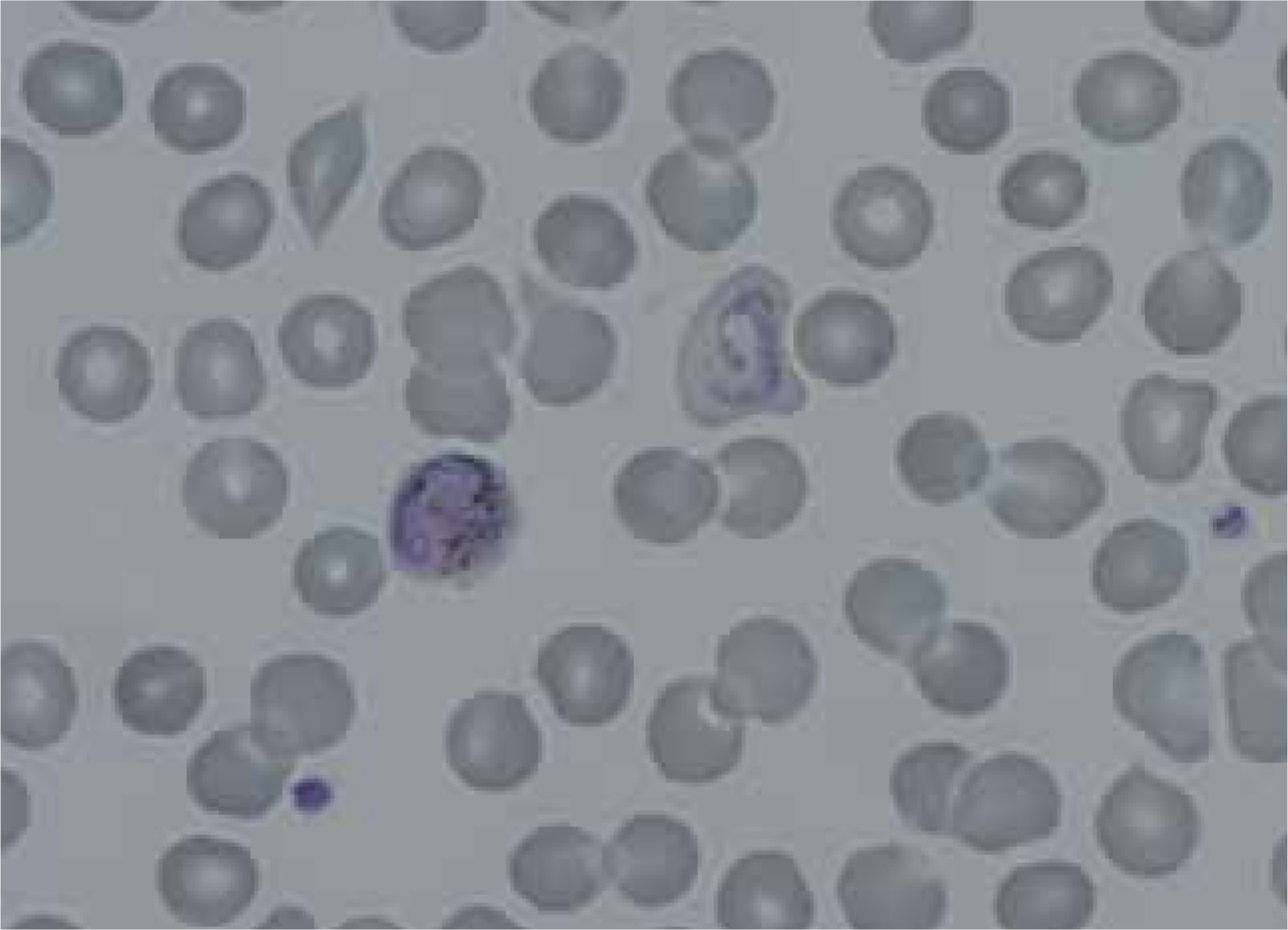
Article54. Kim NH, Lee KH, Jeon YS, Cho SG, Kim JH. Spontaneous splenic rupture in a vivax malaria case treated with transcatheter coil embolization of the splenic artery. Korean J Parasitol. 2015; 53:215–218.
Article55. Bahk YY, Park SH, Lee W, Jin K, Ahn SK, Na BK, Kim TS. Comparative assessment of diagnostic performances of two commercial rapid diagnostic test kits for detection of Plasmodium spp. in Ugandan patients with malaria. Korean J Parasitol. 2018; 56:447–452.
Article