Clin Exp Otorhinolaryngol.
2019 Aug;12(3):308-316. 10.21053/ceo.2018.01235.
Clinical Outcomes of a 14-Day In-Hospital Stay Program in Patients Undergoing Head and Neck Cancer Surgery With Free Flap Reconstruction Under the National Health Insurance System
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hansin.jeong@samsung.com
- KMID: 2455373
- DOI: http://doi.org/10.21053/ceo.2018.01235
Abstract
OBJECTIVES
Length of in-hospital stay (LOS) is often regarded as a surrogate marker of efficiency in medical care. A shorter stay can redistribute medical resources to more patients if patient outcomes would not be worsened. However, the adequate LOS remains largely understudied for a complex head and neck cancer (HNC) surgery and free flap reconstruction.
METHODS
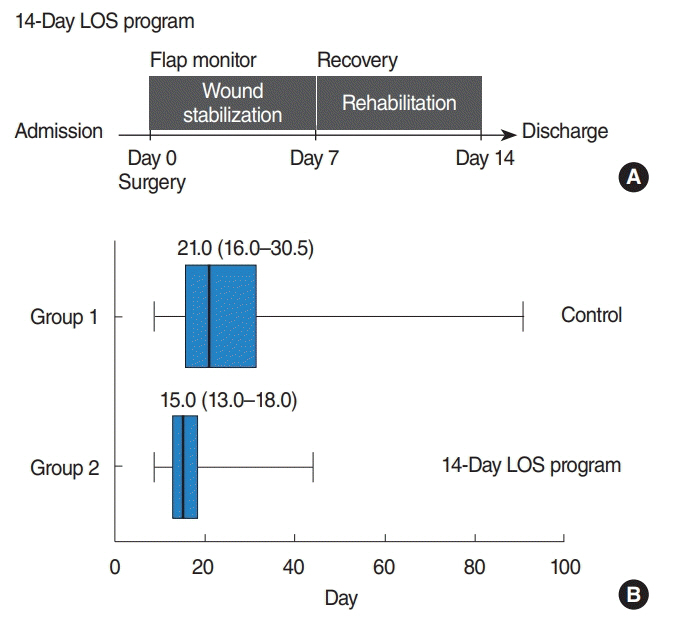
Active management of LOS (14-day LOS program) included detailed preoperative surgical planning, intensive wound care, postoperative early ambulation and positive psychological encouragement. It was applied to 43 patients undergoing HNC surgery and free flap reconstruction. Outcomes such as noninferior oncological results, rates of timely adjuvant treatments and complications were compared with those of 125 patients without active management of LOS. In addition, the medical costs of shortened LOS were compared with those of the control group. Cases undergoing HNC surgery as a salvage treatment were excluded from both groups for analyses.
RESULTS
Active management of LOS resulted in less in-hospital period compared to the control group (15.0 vs. 21.0 days, P=0.001), and reduced medical costs significantly. Incidence of postoperative complications was comparable between the two groups. Oncological outcomes did not differ significantly according to LOS. In all patients in both groups, initial high T status (T3-4) and occurrence of postoperative complications were independent risk factors for long LOS (>30 days).
CONCLUSION
In patients undergoing HNC surgery with free flap reconstruction as an initial treatment, a 14-day LOS could be safe in terms of comparable oncological outcomes and postoperative complications. To achieve this goal safely, careful management for T3-4 tumors and prevention of postoperative complications seem to be necessary.
MeSH Terms
Figure
Reference
-
1. Rosenthal E, Carroll W, Dobbs M, Scott Magnuson J, Wax M, Peters G. Simplifying head and neck microvascular reconstruction. Head Neck. 2004; Nov. 26(11):930–6.
Article2. Cordeiro PG, Hidalgo DA. Soft tissue coverage of mandibular reconstruction plates. Head Neck. 1994; Mar-Apr. 16(2):112–5.
Article3. Kroll SS, Reece GP, Miller MJ, Schusterman MA. Comparison of the rectus abdominis free flap with the pectoralis major myocutaneous flap for reconstructions in the head and neck. Am J Surg. 1992; Dec. 164(6):615–8.
Article4. Schusterman MA, Kroll SS, Weber RS, Byers RM, Guillamondegui O, Goepfert H. Intraoral soft tissue reconstruction after cancer ablation: a comparison of the pectoralis major flap and the free radial forearm flap. Am J Surg. 1991; Oct. 162(4):397–9.
Article5. Stern JR, Keller AJ, Wenig BL. Evaluation of reconstructive techniques of oropharyngeal defects. Ann Plast Surg. 1989; Apr. 22(4):332–6.
Article6. Kroll SS, Evans GR, Goldberg D, Wang BG, Reece GP, Miller MJ, et al. A comparison of resource costs for head and neck reconstruction with free and pectoralis major flaps. Plast Reconstr Surg. 1997; Apr. 99(5):1282–6.
Article7. Ryan MW, Hochman M. Length of stay after free flap reconstruction of the head and neck. Laryngoscope. 2000; Feb. 110(2 Pt 1):210–6.
Article8. Girod A, Brancati A, Mosseri V, Kriegel I, Jouffroy T, Rodriguez J. Study of the length of hospital stay for free flap reconstruction of oral and pharyngeal cancer in the context of the new French casemix-based funding. Oral Oncol. 2010; Mar. 46(3):190–4.
Article9. Cohen J, Stock M, Chan B, Meininger M, Wax M, Andersen P, et al. Microvascular reconstruction and tracheotomy are significant determinants of resource utilization in head and neck surgery. Arch Otolaryngol Head Neck Surg. 2000; Aug. 126(8):947–9.
Article10. Haughey BH, Wilson E, Kluwe L, Piccirillo J, Fredrickson J, Sessions D, et al. Free flap reconstruction of the head and neck: analysis of 241 cases. Otolaryngol Head Neck Surg. 2001; Jul. 125(1):10–7.
Article11. Kiener JL, Hoffman WY, Mathes SJ. Influence of radiotherapy on microvascular reconstruction in the head and neck region. Am J Surg. 1991; Oct. 162(4):404–7.
Article12. Lueg EA. Comparing microvascular outcomes at a large integrated health maintenance organization with flagship centers in the United States. Arch Otolaryngol Head Neck Surg. 2004; Jun. 130(6):779–85.
Article13. Cloke DJ, Green JE, Khan AL, Hodgkinson PD, McLean NR. Factors influencing the development of wound infection following free-flap reconstruction for intra-oral cancer. Br J Plast Surg. 2004; Sep. 57(6):556–60.
Article14. Klug C, Berzaczy D, Reinbacher H, Voracek M, Rath T, Millesi W, et al. Influence of previous radiotherapy on free tissue transfer in the head and neck region: evaluation of 455 cases. Laryngoscope. 2006; Jul. 116(7):1162–7.
Article15. Papi M, Pontecorvi L, Setola R. A new model for the length of stay of hospital patients. Health Care Manag Sci. 2016; Mar. 19(1):58–65.
Article16. Bonde C, Khorasani H, Eriksen K, Wolthers M, Kehlet H, Elberg J. Introducing the fast track surgery principles can reduce length of stay after autologous breast reconstruction using free flaps: a case control study. J Plast Surg Hand Surg. 2015; 49(6):367–71.
Article17. Coyle MJ, Main B, Hughes C, Craven R, Alexander R, Porter G, et al. Enhanced recovery after surgery (ERAS) for head and neck oncology patients. Clin Otolaryngol. 2016; Apr. 41(2):118–26.
Article18. Willemsen PJ, Appeltans BM. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 1999; Jul. 86(7):968–9.19. Nicholson A, Lowe MC, Parker J, Lewis SR, Alderson P, Smith AF. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg. 2014; Feb. 101(3):172–88.
Article20. Patel RS, McCluskey SA, Goldstein DP, Minkovich L, Irish JC, Brown DH, et al. Clinicopathologic and therapeutic risk factors for perioperative complications and prolonged hospital stay in free flap reconstruction of the head and neck. Head Neck. 2010; Oct. 32(10):1345–53.
Article21. Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol. 2014; Oct. 20(38):13950–5.22. Pearsall EA, Meghji Z, Pitzul KB, Aarts MA, McKenzie M, McLeod RS, et al. A qualitative study to understand the barriers and enablers in implementing an enhanced recovery after surgery program. Ann Surg. 2015; Jan. 261(1):92–6.
Article23. Xu X, Wang Y, Feng T, Zhao X, Liao Y, Ji W, et al. Nonstrict and individual enhanced recovery after surgery (ERAS) in partial hepatectomy. Springerplus. 2016; Nov. 5(1):2011.
Article24. Ding J, Sun B, Song P, Liu S, Chen H, Feng M, et al. The application of enhanced recovery after surgery (ERAS)/fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Oncotarget. 2017; Jun. 8(43):75699–711.
Article25. Schmidt CR. Enhanced recovery after surgery-Summary recommendations. J Surg Oncol. 2017; Oct. 116(5):638.
Article26. Zhao Y, Qin H, Wu Y, Xiang B. Enhanced recovery after surgery program reduces length of hospital stay and complications in liver resection: a PRISMA-compliant systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2017; Aug. 96(31):e7628.27. Bater M, King W, Teare J, D’Souza J. Enhanced recovery in patients having free tissue transfer for head and neck cancer: does it make a difference. Br J Oral Maxillofac Surg. 2017; Dec. 55(10):1024–9.
Article28. Gemma M, Toma S, Lira Luce F, Beretta L, Braga M, Bussi M. Enhanced recovery program (ERP) in major laryngeal surgery: building a protocol and testing its feasibility. Acta Otorhinolaryngol Ital. 2017; Dec. 37(6):475–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Six Cases of Reconstruction with Latissimus Dorsi Pedicled Flap for Head and Neck Defects in the Era of Free Flap Reconstruction
- Robot-Assisted Free Flap Reconstruction for Oropharyngeal Cancer: A Systematic Review
- Reconstruction of Midfacial Defect With Radial Forearm Free Flap
- Lateral Arm Free Flap for Oral Cavity and Oropharyngeal Reconstruction
- Early Experiences of Head and Neck Reconstruction: Appropriacy and Surgical Outcome