Anesth Pain Med.
2019 Jul;14(3):322-330. 10.17085/apm.2019.14.3.322.
The effect of early extubation on postoperative delirium in patients with liver transplantation: a propensity score matching analysis
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea. yoonji07@gmail.com
- 2Department of Anesthesiology and Pain Medicine, Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- KMID: 2454818
- DOI: http://doi.org/10.17085/apm.2019.14.3.322
Abstract
- BACKGROUND
Maintenance of tracheal intubation is associated with use of sedatives, stress due to mechanical ventilation, or respiratory complications. The aim of this study is to compare the incidence of delirium between early and late extubation groups after liver transplantation (LT).
METHODS
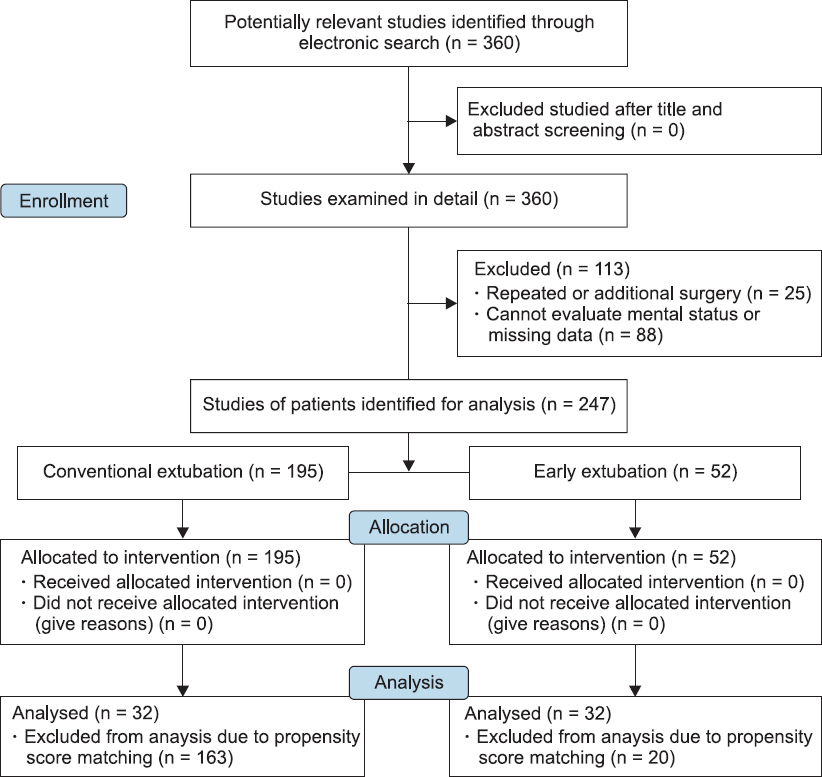
Medical records from 247 patients who received LT from January 2010 to July 2017 in a single university hospital were retrospectively reviewed. Patients were divided with 2 groups: Those who underwent early extubation after LT (E group, n = 52) and those who underwent extubation within few hours of intensive care unit (ICU) admission after surgery (C group, n = 195). The patients' demographic data, perioperative managements and postoperative complications were collected. Early extubation was defined as performing extubation in the operating room after LT. A propensity score matching analysis was performed to reduce the effects of selection bias.
RESULTS
Among them, 4/52 (7.69%) in E group and 30/195 (15.38%) in C group occurred postoperative delirium after LT, respectively (P = 0.180). After propensity score matching, there was no difference of the period of hospitalization in ICU (P = 0.961), time to discharge after surgery (P = 0.117) and incidence of delirium between groups (P = 1.000).
CONCLUSIONS
Although this study is a retrospective study and limited by the small number of subjects, early extubation does not affect the incidence of delirium after LT. Therefore, further prospective studies on this were needed.
MeSH Terms
-
Airway Extubation
Delirium*
Hospitalization
Humans
Hypnotics and Sedatives
Incidence
Intensive Care Units
Intubation
Liver Transplantation*
Liver*
Medical Records
Operating Rooms
Postoperative Complications
Propensity Score*
Prospective Studies
Respiration, Artificial
Retrospective Studies
Selection Bias
Hypnotics and Sedatives
Figure
Reference
-
1. Vogt DP, Lederman RJ, Carey WD, Broughan TA. Neurologic complications of liver transplantation. Transplantation. 1988; 45:1057–61. DOI: 10.1097/00007890-198806000-00011. PMID: 2837845.2. Mueller AR, Platz KP, Krause P, Kahl A, Rayes N, Glanemann M, et al. Perioperative factors influencing patient outcome after liver transplantation. Transpl Int. 2000; 13(Suppl 1):S158–61. DOI: 10.1111/j.1432-2277.2000.tb02010.x. PMID: 11111987.3. Bronster DJ, Emre S, Mor E, Sheiner P, Miller CM, Schwartz ME. Neurologic complications of orthotopic liver transplantation. Mt Sinai J Med. 1994; 61:63–9. PMID: 8183296.4. Algahtani HA, Abdu AP. Delirium. A comprehensive review. Neurosciences (Riyadh). 2012; 17:205–12.5. Mody K, Kaur S, Mauer EA, Gerber LM, Greenwald BM, Silver G, et al. Benzodiazepines and development of delirium in critically ill children:estimating the causal effect. Crit Care Med. 2018; 46:1486–91. DOI: 10.1097/CCM.0000000000003194. PMID: 29727363.6. Haugen CE, Mountford A, Warsame F, Berkowitz R, Bae S, Thomas AG, et al. Incidence, risk factors, and sequelae of post- kidney transplant delirium. J Am Soc Nephrol. 2018; 29:1752–9. DOI: 10.1681/ASN.2018010064. PMID: 29685884. PMCID: PMC6054339.7. Clegg A, Siddiqi N, Heaven A, Young J, Holt R. Interventions for preventing delirium in older people in institutional long-term care. Cochrane Database Syst Rev. 2014; 1:CD009537. DOI: 10.1002/14651858.CD009537.pub2. PMID: 24488526.8. Choi JG. Delirium in the intensive care unit. Korean J Anesthesiol. 2013; 65:195–202. DOI: 10.4097/kjae.2013.65.3.195. PMID: 24101952. PMCID: PMC3790029.9. Mandell MS, Lezotte D, Kam I, Zamudio S. Reduced use of intensive care after liver transplantation:influence of early extubation. Liver Transpl. 2002; 8:676–81. DOI: 10.1053/jlts.2002.34379. PMID: 12149759.10. Cuervas-Mons V, Julio Martinez A, Dekker A, Starzl TE, Van Thiel DH. Adult liver transplantation:an analysis of the early causes of death in 40 consecutive cases. Hepatology. 1986; 6:495–501. DOI: 10.1002/hep.1840060329. PMID: 3519418. PMCID: PMC2964136.11. Plevak DJ, Southorn PA, Narr BJ, Peters SG. Intensive-care unit experience in the Mayo liver transplantation program:the first 100 cases. Mayo Clin Proc. 1989; 64:433–45. DOI: 10.1016/S0025-6196(12)65734-6. PMID: 2654500.12. Stock PG, Payne WD. Liver transplantation. Crit Care Clin. 1990; 6:911–26. DOI: 10.1016/S0749-0704(18)30345-2. PMID: 2265386.13. Muralidhar V, Jayalaxmi TS. Anaesthesia for liver transplantation:perioperative problems and management. Trop Gastroenterol. 1994; 15:191–203. PMID: 7618200.14. Carton EG, Plevak DJ, Kranner PW, Rettke SR, Geiger HJ, Coursin DB. Perioperative care of the liver transplant patient:part 2. Anesth Analg. 1994; 78:382–99. DOI: 10.1213/00000539-199402000-00031. PMID: 8311294.15. Choi JH, Kim TH, Lee JM. Evaluation of usefulness of perioperative risk factors which affect early or delayed extubation after liver transplantation. Korean J Anesthesiol. 2003; 44:847–52. DOI: 10.4097/kjae.2003.44.6.847.16. Blacher RS. The psychological and psychiatric consequences of the ICU stay. Eur J Anaesthesiol Suppl. 1997; 15:45–7. DOI: 10.1097/00003643-199705001-00009. PMID: 9202938.17. Tilouche N, Hassen MF, Ali HBS, Jaoued O, Gharbi R, El Atrous SS. Delirium in the intensive care unit:incidence, risk factors, and impact on outcome. Indian J Crit Care Med. 2018; 22:144–9. DOI: 10.4103/ijccm.IJCCM_244_17. PMID: 29657370. PMCID: PMC5879855.18. Kolkka R, Hilberman M. Neurologic dysfunction following cardiac operation with low-flow, low-pressure cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1980; 79:432–7. PMID: 6965513.19. Sadler PD. Incidence, degree, and duration of postcardiotomy delirium. Heart Lung. 1981; 10:1084–92. PMID: 6913574.20. Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004; 291:1753–62. DOI: 10.1001/jama.291.14.1753. PMID: 15082703.21. Baliga P, Merion RM, Turcotte JG, Ham JM, Henley KS, Lucey MR, et al. Preoperative risk factor assessment in liver transplantation. Surgery. 1992; 112:704–10. PMID: 1411941.22. Lee JM, Choi JH, Kim BS, Kim YG. Evaluation of clinical factors associated with early tracheal extubation after liver transplantation. Korean J Anesthesiol. 1999; 36:645–52. DOI: 10.4097/kjae.1999.36.4.645.23. Shaw BW Jr, Wood RP, Gordon RD, Iwatsuki S, Gillquist WP, Starzl TE. Influence of selected patient variables and operative blood loss on six-month survival following liver transplantation. Semin Liver Dis. 1985; 5:385–93. DOI: 10.1055/s-2008-1040637. PMID: 3909433. PMCID: PMC3022507.24. Michard B, Artzner T, Lebas B, Besch C, Guillot M, Faitot F, et al. Liver transplantation in critically ill patients:preoperative predictive factors of post-transplant mortality to avoid futility. Clin Transplant. 2017; 31:e13115. DOI: 10.1111/ctr.13115. PMID: 28895204.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Patient-controlled Intravenous Analgesia (PCIA) on Postoperative Delirium in Patients with Liver Transplantation: a Propensity Score Matching Analysis
- Evaluation of Clinical Factors Associated with Early Tracheal Extubation after Liver Transplantation
- Risk Factors for Postoperative Delirium after Liver Transplantation in the Intensive Care Unit
- Applications of propensity score matching: a case series of articles published in Annals of Coloproctology
- Evaluation of Usefulness of Perioperative Risk Factors Which Affect Early or Delayed Extubation after Liver Transplantation