Anesth Pain Med.
2019 Jul;14(3):266-271. 10.17085/apm.2019.14.3.266.
Effects of fetal position on maternal hemodynamics after spinal anesthesia for cesarean delivery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Cheil General Hospital & Women's Healthcare Center, Seoul, Korea. kmh1201h@naver.com
- KMID: 2454810
- DOI: http://doi.org/10.17085/apm.2019.14.3.266
Abstract
- BACKGROUND
Aortocaval compression by the gravid uterus is a known physiological phenomenon that is classically claimed to cause supine hypotension in full-term pregnant women. This study aimed to investigate the effects of fetal position on maternal hemodynamics after spinal anesthesia during cesarean delivery.
METHODS
In total, 71 women with intrauterine pregnancy over 36 weeks of gestation who were scheduled for elective cesarean delivery under spinal anesthesia were enrolled in the study. Based on the fetal position, the women were divided into two groups: right position group (group R) and left position group (group L). Occurrence of hypotension, requirement for rescue bolus injections of phenylephrine, and the total amount of infused phenylephrine before delivery were recorded in each group.
RESULTS
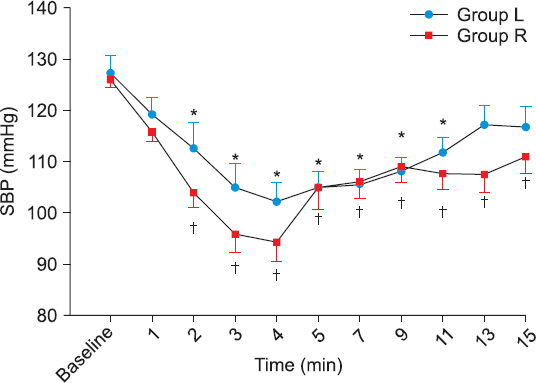
There was no statistically significant difference in the occurrence of hypotension between the two groups (P = 0.075); however, the amount of phenylephrine required before delivery was significantly greater in group R (P = 0.028). There was a statistically significant decrease in the systolic blood pressure compared with the baseline values in group R, and this change persisted until 15 min after spinal anesthesia.
CONCLUSIONS
There was no difference according to fetal position in the number of patients who showed hypotension before delivery after spinal anesthesia.
Keyword
MeSH Terms
Figure
Reference
-
1. Howard BK, Goodson JH, Mengert WF. Supine hypotensive syndrome in late pregnancy. Obstet Gynecol. 1953; 1:371–7. PMID: 13055188.2. Emmett RS, Cyna AM, Andrew M, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 2001; 3:CD002251. DOI: 10.1002/14651858.CD002251. PMID: 11687021. PMCID: PMC6009735.3. Ngan Kee WD. Prevention of maternal hypotension after regional anaesthesia for caesarean section. Curr Opin Anaesthesiol. 2010; 23:304–9. DOI: 10.1097/ACO.0b013e328337ffc6. PMID: 20173633.4. Sharwood-Smith G, Drummond GB. Hypotension in obstetric spinal anaesthesia:a lesson from pre-eclampsia. Br J Anaesth. 2009; 102:291–4. DOI: 10.1093/bja/aep003. PMID: 19218369.5. Kinsella SM, Lohmann G. Supine hypotensive syndrome. Obstet Gynecol. 1994; 83(5 Pt 1):774–88. PMID: 8164943.6. Holmes F. The supine hypotensive syndrome 1960. Anaesthesia. 1995; 50:972–7. DOI: 10.1111/j.1365-2044.1995.tb05931.x. PMID: 8678255.7. Tihtonen K, Kööbi T, Yli-Hankala A, Huhtala H, Uotila J. Maternal haemodynamics in pre-eclampsia compared with normal pregnancy during caesarean delivery. BJOG. 2006; 113:657–63. DOI: 10.1111/j.1471-0528.2006.00931.x. PMID: 16709208.8. Stewart A, Fernando R, McDonald S, Hignett R, Jones T, Columb M. The dose-dependent effects of phenylephrine for elective cesarean delivery under spinal anesthesia. Anesth Analg. 2010; 111:1230–7. DOI: 10.1213/ANE.0b013e3181f2eae1. PMID: 20841418.9. Weis FR Jr, Markello R, Mo B, Bochiechio P. Cardiovascular effects of oxytocin. Obstet Gynecol. 1975; 46:211–4. PMID: 1153152.10. Langesaeter E, Rosseland LA, Stubhaug A. Hemodynamic effects of oxytocin during cesarean delivery. Int J Gynaecol Obstet. 2006; 95:46–7. DOI: 10.1016/j.ijgo.2006.05.032. PMID: 16920118.11. Rosseland LA, Hauge TH, Grindheim G, Stubhaug A, Langesæter E. Changes in blood pressure and cardiac output during cesarean delivery:the effects of oxytocin and carbetocin compared with placebo. Anesthesiology. 2013; 119:541–51. DOI: 10.1097/ALN.0b013e31829416dd. PMID: 23598289.12. Langesaeter E, Rosseland LA, Stubhaug A. Haemodynamic effects of repeated doses of oxytocin during Caesarean delivery in healthy parturients. Br J Anaesth. 2009; 103:260–2. DOI: 10.1093/bja/aep137. PMID: 19502285.13. Lee AJ, Landau R, Mattingly JL, Meenan MM, Corradini B, Wang S, et al. Left lateral table tilt for elective cesarean delivery under spinal anesthesia has no effect on neonatal acid-base status:a randomized controlled trial. Anesthesiology. 2017; 127:241–9. DOI: 10.1097/ALN.0000000000001737. PMID: 28598894.14. Sohn HM, Won DW, Oh AY, Hwang JW, Song IA. Effect of prolonged lateral position for 10-minutes following spinal anesthesia on hypotension and sensory blockade during cesarean delivery. Anesth Pain Med. 2016; 11:354–8. DOI: 10.17085/apm.2016.11.4.354.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic management for preeclampsia: Hemodynamic monitoring and volume therapy
- The Comparison of Maternal Hemodynamics and Infant's Apgar Score between the Supine Position with and without Left Uterine Displacement for a Cesarean Section
- Comparison of Neonatal Outcomes among Patients Undergoing Cesarean Delivery under General or Spinal Anesthesia
- Comparison of maternal and fetal effects of ephedrine, phenylephrine, and combination infusion during spinal anesthesia for cesarean delivery
- Plasma Concentrations of Prolactin and Cortisol during Cesarean Section under General and Spinal Anesthesia