Ann Clin Neurophysiol.
2018 Jul;20(2):101-104. 10.14253/acn.2018.20.2.101.
Electrophysiological and radiological evidence for the multifocal nature of a case of multifocal acquired demyelinating sensory and motor neuropathy
- Affiliations
-
- 1Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 2Department of Neurology, Kangdong Sacred Heart Hospital, Seoul, Korea.
- 3Department of Neurology, Haedong Hospital, Busan, Korea. sanghyoryu@gmail.com
- KMID: 2454714
- DOI: http://doi.org/10.14253/acn.2018.20.2.101
Abstract
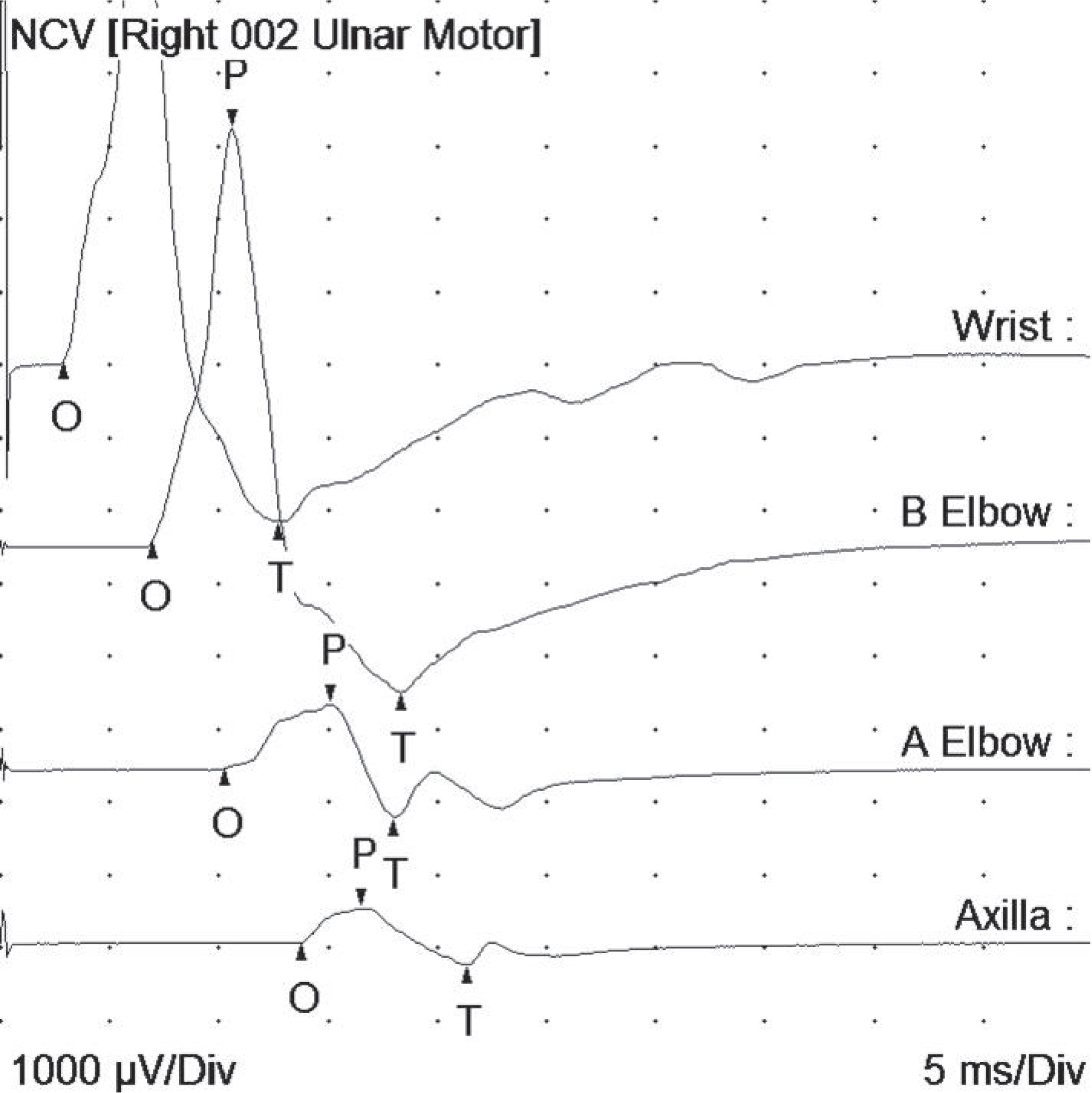
- Multifocal acquired demyelinating sensory and motor (MADSAM) neuropathy is a variant of chronic acquired demyelinating polyneuropathy. A 65-year-old women presented with upper arm weakness. A nerve conduction study showed conduction blocks over intermediate segments with sparing of distal compound action potentials. Magnetic resonance imaging revealed asymmetric hypertrophy of the brachial plexus on the affected side. These findings represent important electrophysiological and radiological evidence of MADSAM neuropathy. The condition of the patient began to improve after starting intravenous immunoglobulin administration.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Kuwabara S, Misawa S. Chronic inflammatory demyelinating polyneuropathy: clinical subtypes and their correlation with electrophysiology. Clin Exp Neuroimmunol. 2011; 2:41–48.
Article2. Shibuya K, Sugiyama A, Ito S, Misawa S, Sekiguchi Y, Mitsuma S, et el. Reconstruction magnetic resonance neurography in chronic inflammatory demyelinating polyneuropathy. Ann Neurol. 2015; 77:333–337.3. Ad Hoc Subcommittee of the American Academy of Neurology AIDS Task Force. Research criteria for the diagnosis of chronic inflammatory demyelinating polyneuropathy (CIDP). Neurology. 1991; 41:617–618.4. Van den Bergh PY, Hadden RD, Bouche P, Cornblath DR, Hahn A, Illa I, et el. European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society – first revision. Eur J Neurol. 2010; 17:356–363.5. Viala K, ReniéL, Maisonobe T, Béhin A, Neil J, Léger JM, et el. Follow-up study and response to treatment in 23 patients with Lewis-Sumner syndrome. Brain. 2004; 127(Pt 9):2010–2017.6. Park YE, Yook JW, Kim DS. A case of Lewis-Sumner syndrome showing dramatic improvement after plasma exchange. J Korean Med Sci. 2010; 25:1101–1104.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Hypoglossal Neuropathy in Multifocal Acquired Demyelinating Sensory and Motor Neuropathy: Differential Diagnosis of Motor Neuron Disease
- A Case of Multifocal Motor Neuropathy with Conduction Block
- Hemiatrophy of the Tongue with Contralateral Hemiparesis in a Patient with Multifocal Acquired Demyelinating Sensory and Motor Neuropathy
- Hereditary Transthyretin Amyloidosis Misdiagnosed as Demyelinating Neuropathy: A Report of Three Cases
- Conduction Block in Hereditary Motor Sensory Neuropathy