Cancer Res Treat.
2016 Apr;48(2):537-545. 10.4143/crt.2015.081.
Tumor Volume Reduction Rate during Adaptive Radiation Therapy as a Prognosticator for Nasopharyngeal Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ahnyc@skku.edu
- 3Bio-medical Science, Korea University, Seoul, Korea.
- KMID: 2454330
- DOI: http://doi.org/10.4143/crt.2015.081
Abstract
- PURPOSE
The purpose of this study is to evaluate the prognostic significance of the tumor volume reduction rate (TVRR) measured during adaptive definitive radiation therapy (RT) for nasopharyngeal cancer (NPC).
MATERIALS AND METHODS
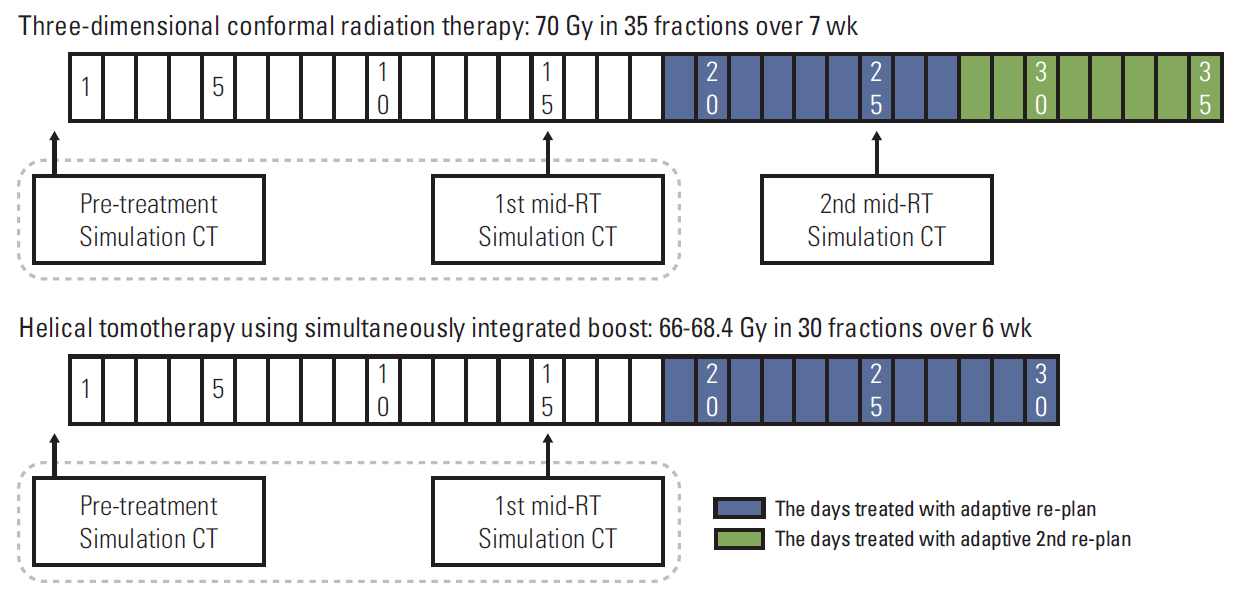
We reviewed the RT records of 159 NPC patients treated with definitive RT with or without concurrent chemotherapy between January 2006 and February 2013. Adaptive re-planning was performed in all patients at the third week of RT. The pre- and mid-RT gross tumor volumes (GTVs) of the primary tumor and the metastatic lymph nodes were measured and analyzed for prognostic implications.
RESULTS
After a median follow-up period of 41.5 months (range, 11.2 to 91.8 months) for survivors, there were 43 treatment failures. The overall survival and progression-free survival (PFS) rates at 5 years were 89.6% and 69.7%, respectively. The mean pre-RT GTV, mid-RT GTV, and TVRR were 45.9 cm3 (range, 1.5 to 185.3 cm3), 26.7 cm3 (1.0 to 113.8 cm3), and -41.9% (range, -87% to 78%), respectively. Patients without recurrence had higher TVRR than those with recurrence (44.3% in the no recurrence group vs. 34.0% in the recurrence group, p=0.004), and those with TVRR > 35% achieved a significantly higher rate of PFS at 5 years (79.2% in TVRR > 35% vs. 53.2% in TVRR ≤ 35%; p < 0.001). In multivariate analysis, TVRR was a significant factor affecting PFS (hazard ratio, 2.877; 95% confidence interval, 1.555 to 5.326; p=0.001).
CONCLUSION
TVRR proved to be a significant prognostic factor in NPC patients treated with definitive RT, and could be used as a potential indicator for early therapeutic modification during the RT course.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. New York: Springer;2009.2. Ball DL, Fisher R, Burmeister B, Graham P, Joseph D, Penniment M, et al. Stage is not a reliable indicator of tumor volume in non-small cell lung cancer: a preliminary analysis of the Trans-Tasman Radiation Oncology Group 99-05 database. J Thorac Oncol. 2006; 1:667–72.
Article3. Chen MK, Chen TH, Liu JP, Chang CC, Chie WC. Better prediction of prognosis for patients with nasopharyngeal carcinoma using primary tumor volume. Cancer. 2004; 100:2160–6.
Article4. Chua DT, Sham JS, Kwong DL, Tai KS, Wu PM, Lo M, et al. Volumetric analysis of tumor extent in nasopharyngeal carcinoma and correlation with treatment outcome. Int J Radiat Oncol Biol Phys. 1997; 39:711–9.
Article5. Lok BH, Setton J, Caria N, Romanyshyn J, Wolden SL, Zelefsky MJ, et al. Intensity-modulated radiation therapy in oropharyngeal carcinoma: effect of tumor volume on clinical outcomes. Int J Radiat Oncol Biol Phys. 2012; 82:1851–7.
Article6. Wang JZ, Mayr NA, Zhang D, Li K, Grecula JC, Montebello JF, et al. Sequential magnetic resonance imaging of cervical cancer: the predictive value of absolute tumor volume and regression ratio measured before, during, and after radiation therapy. Cancer. 2010; 116:5093–101.7. Nam H, Park W, Huh SJ, Bae DS, Kim BG, Lee JH, et al. The prognostic significance of tumor volume regression during radiotherapy and concurrent chemoradiotherapy for cervical cancer using MRI. Gynecol Oncol. 2007; 107:320–5.
Article8. Lee H, Ahn YC, Oh D, Nam H, Kim YI, Park SY. Tumor volume reduction rate measured during adaptive definitive radiation therapy as a potential prognosticator of locoregional control in patients with oropharyngeal cancer. Head Neck. 2014; 36:499–504.
Article9. Hoeben BA, Troost EG, Span PN, van Herpen CM, Bussink J, Oyen WJ, et al. 18F-FLT PET during radiotherapy or chemoradiotherapy in head and neck squamous cell carcinoma is an early predictor of outcome. J Nucl Med. 2013; 54:532–40.
Article10. Yeo SG, Kim DY, Park JW, Oh JH, Kim SY, Chang HJ, et al. Tumor volume reduction rate after preoperative chemoradiotherapy as a prognostic factor in locally advanced rectal cancer. Int J Radiat Oncol Biol Phys. 2012; 82:e193–9.
Article11. Yang SN, Liao CY, Chen SW, Liang JA, Tsai MH, Hua CH, et al. Clinical implications of the tumor volume reduction rate in head-and-neck cancer during definitive intensity-modulated radiotherapy for organ preservation. Int J Radiat Oncol Biol Phys. 2011; 79:1096–103.
Article12. Mancuso AA, Mukherji SK, Schmalfuss I, Mendenhall W, Parsons J, Pameijer F, et al. Preradiotherapy computed tomography as a predictor of local control in supraglottic carcinoma. J Clin Oncol. 1999; 17:631–7.
Article13. Pameijer FA, Mancuso AA, Mendenhall WM, Parsons JT, Mukherji SK, Hermans R, et al. Evaluation of pretreatment computed tomography as a predictor of local control in T1/T2 pyriform sinus carcinoma treated with definitive radiotherapy. Head Neck. 1998; 20:159–68.
Article14. Barker JL Jr, Garden AS, Ang KK, O'Daniel JC, Wang H, Court LE, et al. Quantification of volumetric and geometric changes occurring during fractionated radiotherapy for head-and-neck cancer using an integrated CT/linear accelerator system. Int J Radiat Oncol Biol Phys. 2004; 59:960–70.
Article15. Castadot P, Geets X, Lee JA, Christian N, Gregoire V. Assessment by a deformable registration method of the volumetric and positional changes of target volumes and organs at risk in pharyngo-laryngeal tumors treated with concomitant chemo-radiation. Radiother Oncol. 2010; 95:209–17.
Article16. Hansen EK, Bucci MK, Quivey JM, Weinberg V, Xia P. Repeat CT imaging and replanning during the course of IMRT for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2006; 64:355–62.
Article17. Bhide SA, Davies M, Burke K, McNair HA, Hansen V, Barbachano Y, et al. Weekly volume and dosimetric changes during chemoradiotherapy with intensity-modulated radiation therapy for head and neck cancer: a prospective observational study. Int J Radiat Oncol Biol Phys. 2010; 76:1360–8.
Article18. Wang W, Yang H, Hu W, Shan G, Ding W, Yu C, et al. Clinical study of the necessity of replanning before the 25th fraction during the course of intensity-modulated radiotherapy for patients with nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2010; 77:617–21.
Article19. Zhao L, Wan Q, Zhou Y, Deng X, Xie C, Wu S. The role of replanning in fractionated intensity modulated radiotherapy for nasopharyngeal carcinoma. Radiother Oncol. 2011; 98:23–7.
Article20. Yang H, Hu W, Wang W, Chen P, Ding W, Luo W. Replanning during intensity modulated radiation therapy improved quality of life in patients with nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2013; 85:e47–54.
Article21. Bosmans G, van Baardwijk A, Dekker A, Ollers M, Boersma L, Minken A, et al. Intra-patient variability of tumor volume and tumor motion during conventionally fractionated radiotherapy for locally advanced non-small-cell lung cancer: a prospective clinical study. Int J Radiat Oncol Biol Phys. 2006; 66:748–53.
Article22. Britton KR, Starkschall G, Tucker SL, Pan T, Nelson C, Chang JY, et al. Assessment of gross tumor volume regression and motion changes during radiotherapy for non-small-cell lung cancer as measured by four-dimensional computed tomography. Int J Radiat Oncol Biol Phys. 2007; 68:1036–46.
Article23. Chan AT, Ma BB, Lo YM, Leung SF, Kwan WH, Hui EP, et al. Phase II study of neoadjuvant carboplatin and paclitaxel followed by radiotherapy and concurrent cisplatin in patients with locoregionally advanced nasopharyngeal carcinoma: therapeutic monitoring with plasma Epstein-Barr virus DNA. J Clin Oncol. 2004; 22:3053–60.
Article24. Lin JC, Chen KY, Wang WY, Jan JS, Liang WM, Tsai CS, et al. Detection of Epstein-Barr virus DNA in the peripheral-blood cells of patients with nasopharyngeal carcinoma: relationship to distant metastasis and survival. J Clin Oncol. 2001; 19:2607–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Multiple Complications after Treatment in Patients with the Second Primary Nasopharyngeal Cancer
- A Case of Postradiation Chondrosarcoma of the Sphenoid and Clivus
- Early treatment volume reduction rate as a prognostic factor in patients treated with chemoradiotherapy for limited stage small cell lung cancer
- Less is more: level IB-sparing radiation therapy in nasopharyngeal cancer
- Nasopharyngeal Cancer in Patients Under Thirty Years of Age