Cancer Res Treat.
2019 Jul;51(3):1001-1010. 10.4143/crt.2018.415.
Dummy Run of Quality Assurance Program before Prospective Study of Hippocampus-Sparing Whole-Brain Radiotherapy and Simultaneous Integrated Boost for Multiple Brain Metastases from Non-small Cell Lung Cancer: Korean Radiation Oncology Group (KROG) 17-06 Study
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ahnyc@skku.edu
- 2Department of Radiation Oncology, Gachon University Gil Medical Center, Incheon, Korea.
- 3Department of Radiation Oncology, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 4Department of Radiation Oncology, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 5Proton Therapy Center, National Cancer Center, Goyang, Korea.
- 6Department of Radiation Oncology, Korea University Guro Hospital, Seoul, Korea.
- 7Department of Radiation Oncology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 8Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea.
- 9Department of Radiation Oncology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 10Department of Radiation Oncology, Ajou University School of Medicine, Suwon, Korea.
- 11Department of Radiation Oncology, Yeungnam University College of Medicine, Daegu, Korea.
- 12Department of Radiation Oncology, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea.
- 13Department of Radiation Oncology, Ewha Womans University School of Medicine, Seoul, Korea.
- 14Department of Radiation Oncology, Jeju National University School of Medicine, Jeju, Korea.
- 15Department of Radiation Oncology, Chungbuk National University College of Medicine, Cheongju, Korea.
- 16Department of Radiation Oncology, School of Medicine, Kyungpook National University Daegu, Korea.
- 17Department of Radiation Oncology, Inje University School of Medicine, Busan, Korea.
- 18Department of Medical Device Management and Research, SAIHST, Sungkyunkwan University, Seoul, Korea.
- KMID: 2454292
- DOI: http://doi.org/10.4143/crt.2018.415
Abstract
- PURPOSE
Lung Cancer Subcommittee of Korean Radiation Oncology Group (KROG) has recently launched a prospective clinical trial (KROG 17-06) of hippocampus-sparing whole brain radiotherapy (HS-WBRT) with simultaneous integrated boost (SIB) in treating multiple brain metastases from non-small cell lung cancer. In order to improve trial quality, dummy run studies among the participating institutions were designed. This work reported the results of two-step dummy run procedures of the KROG 17-06 study.
MATERIALS AND METHODS
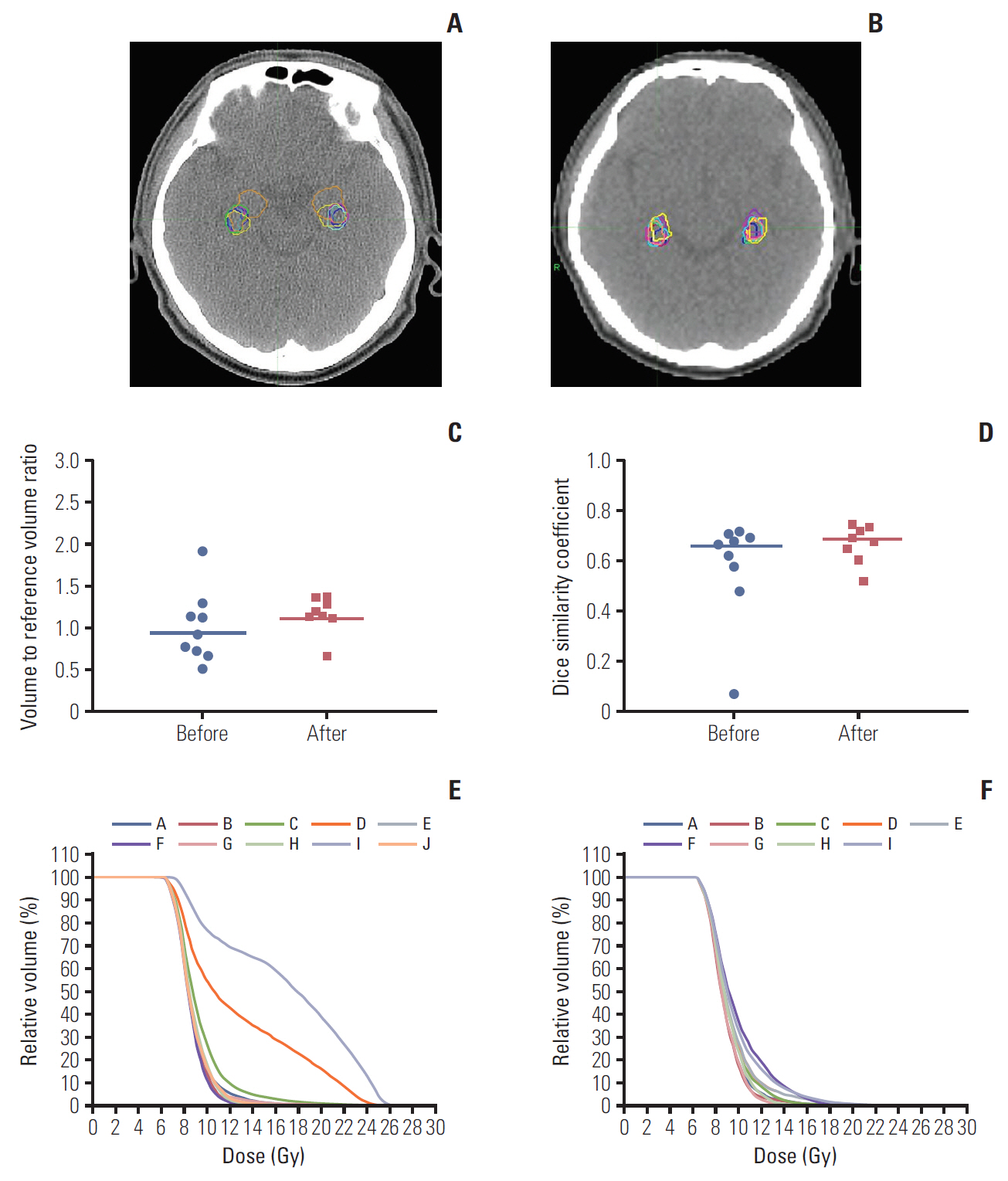
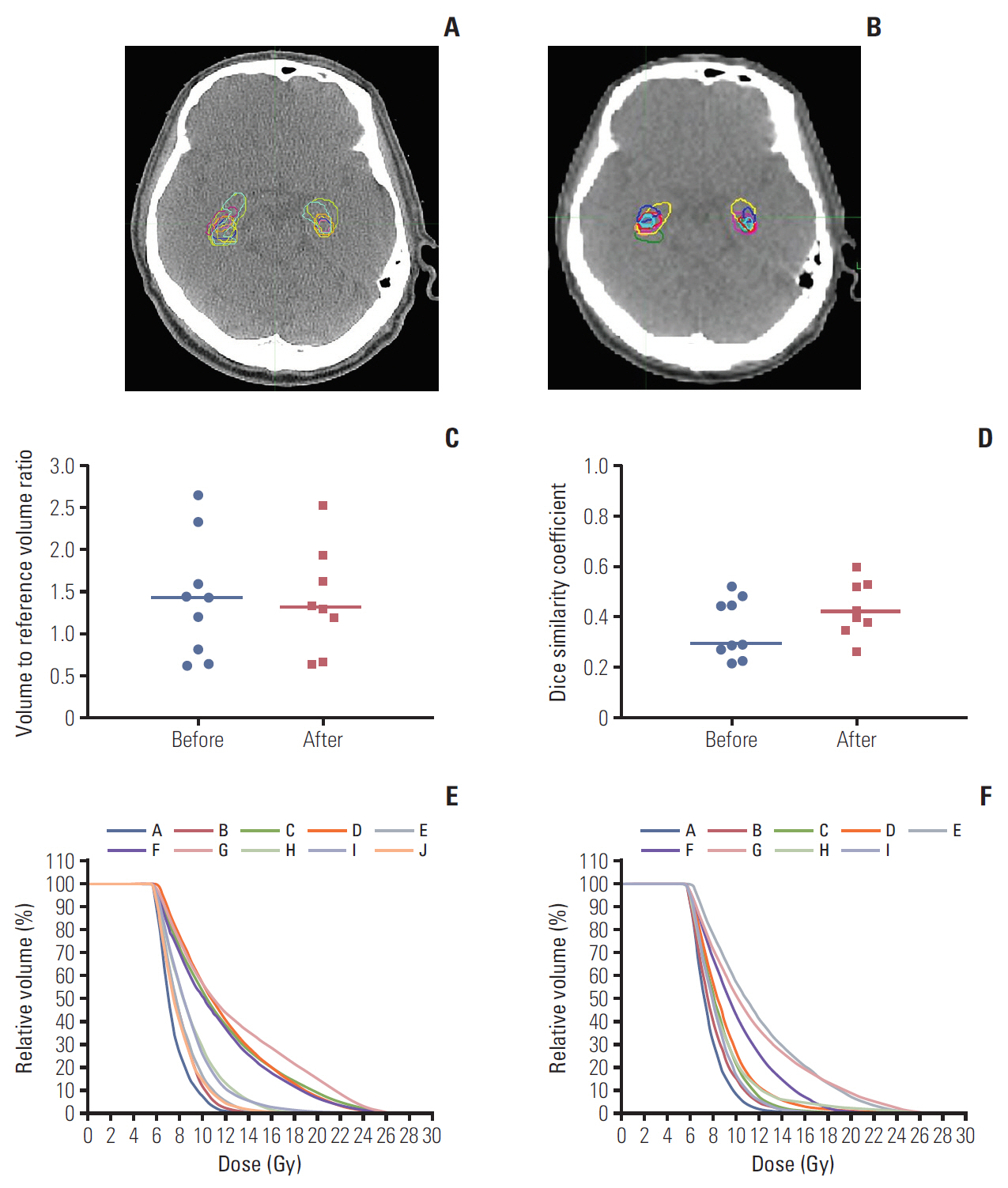
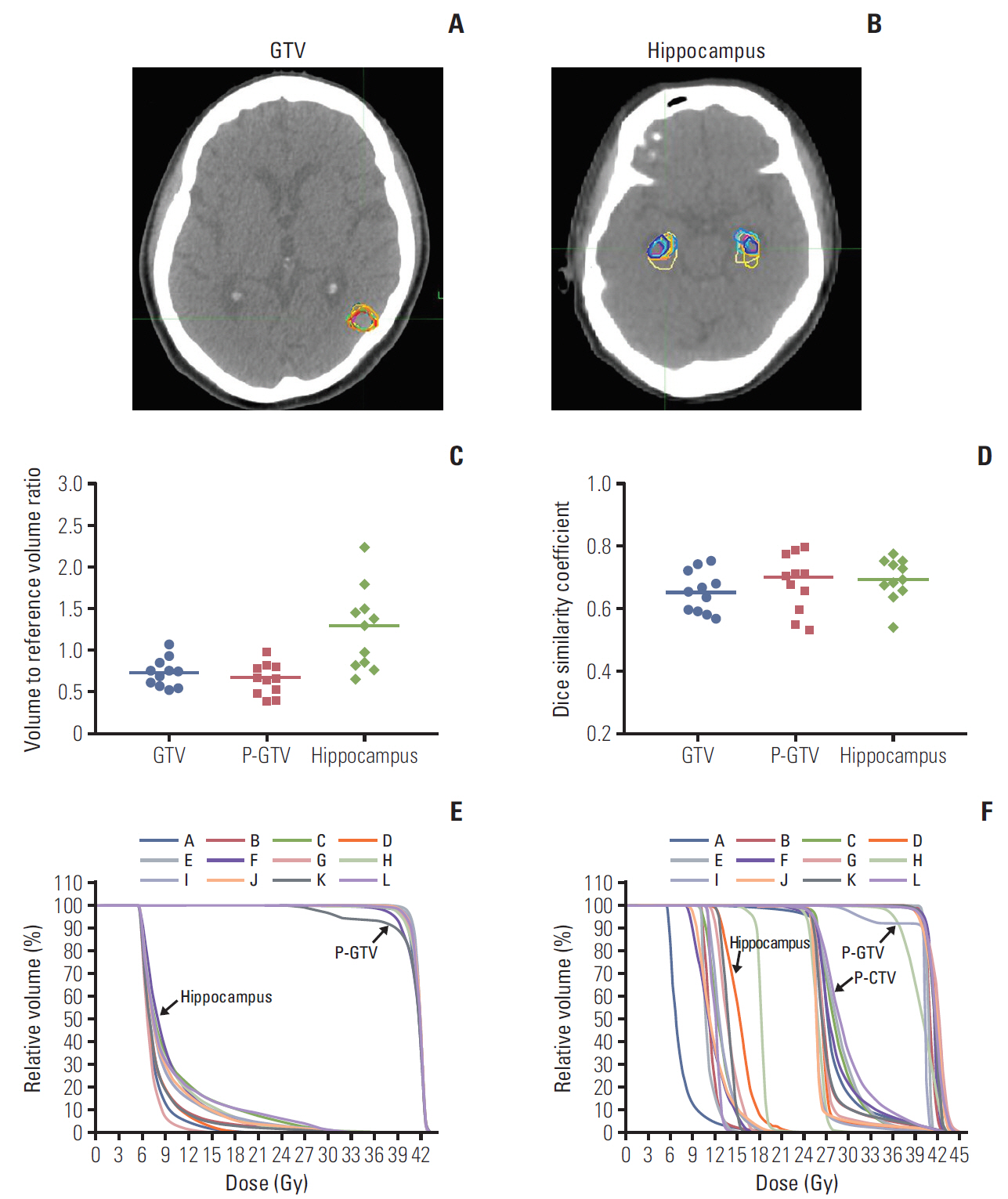
Two steps tested hippocampus contouring variability and radiation therapy planning compliance. In the first step, the variation of the hippocampus delineation was investigated for two representative cases using the Dice similarity coefficients. In the second step, the participating institutions were requested to generate a HS-WBRT with SIB treatment plan for another representative case. The compliance of the treatment plans to the planning protocol was evaluated.
RESULTS
In the first step, the median Dice similarity coefficients of the hippocampus contours for two other dummy run cases changed from 0.669 (range, 0.073 to 0.712) to 0.690 (range, 0.522 to 0.750) and from 0.291 (range, 0.219 to 0.522) to 0.412 (range, 0.264 to 0.598) after providing the hippocampus contouring feedback. In the second step, with providing additional plan priority and extended dose constraints to the target volumes and normal structures, we observed the improved compliance of the treatment plans to the planning protocol.
CONCLUSION
The dummy run studies demonstrated the notable inter-institutional variability in delineating the hippocampus and treatment plan generation, which could be decreased through feedback from the trial center.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Gaspar LE, Mehta MP, Patchell RA, Burri SH, Robinson PD, Morris RE, et al. The role of whole brain radiation therapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010; 96:17–32.
Article2. Tsao MN, Rades D, Wirth A, Lo SS, Danielson BL, Gaspar LE, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): an American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol. 2012; 2:210–25.
Article3. Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA. 2006; 295:2483–91.4. Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009; 10:1037–44.
Article5. Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011; 29:134–41.6. Aoyama H, Tago M, Shirato H; Japanese Radiation Oncology Study Group 99-1 (JROSG 99-1) Investigators. Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 randomized clinical trial. JAMA Oncol. 2015; 1:457–64.7. Gondi V, Tolakanahalli R, Mehta MP, Tewatia D, Rowley H, Kuo JS, et al. Hippocampal-sparing whole-brain radiotherapy: a "how-to" technique using helical tomotherapy and linear accelerator-based intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2010; 78:1244–52.
Article8. Gondi V, Tome WA, Mehta MP. Why avoid the hippocampus? A comprehensive review. Radiother Oncol. 2010; 97:370–6.
Article9. Gondi V, Pugh SL, Tome WA, Caine C, Corn B, Kanner A, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol. 2014; 32:3810–6.
Article10. Hsu F, Carolan H, Nichol A, Cao F, Nuraney N, Lee R, et al. Whole brain radiotherapy with hippocampal avoidance and simultaneous integrated boost for 1-3 brain metastases: a feasibility study using volumetric modulated arc therapy. Int J Radiat Oncol Biol Phys. 2010; 76:1480–5.
Article11. Giaj Levra N, Sicignano G, Fiorentino A, Fersino S, Ricchetti F, Mazzola R, et al. Whole brain radiotherapy with hippocampal avoidance and simultaneous integrated boost for brain metastases: a dosimetric volumetric-modulated arc therapy study. Radiol Med. 2016; 121:60–9.
Article12. Oehlke O, Wucherpfennig D, Fels F, Frings L, Egger K, Weyerbrock A, et al. Whole brain irradiation with hippocampal sparing and dose escalation on multiple brain metastases: Local tumour control and survival. Strahlenther Onkol. 2015; 191:461–9.13. Kim KH, Cho BC, Lee CG, Kim HR, Suh YG, Kim JW, et al. Hippocampus-sparing whole-brain radiotherapy and simultaneous integrated boost for multiple brain metastases from lung adenocarcinoma: early response and dosimetric evaluation. Technol Cancer Res Treat. 2016; 15:122–9.14. Gondi V, Cui Y, Mehta MP, Manfredi D, Xiao Y, Galvin JM, et al. Real-time pretreatment review limits unacceptable deviations on a cooperative group radiation therapy technique trial: quality assurance results of RTOG 0933. Int J Radiat Oncol Biol Phys. 2015; 91:564–70.
Article15. Dice LR. Measures of the amount of ecologic association between species. Ecology. 1945; 26:297–302.
Article16. Zou KH, Warfield SK, Bharatha A, Tempany CM, Kaus MR, Haker SJ, et al. Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol. 2004; 11:178–89.17. Ohri N, Shen X, Dicker AP, Doyle LA, Harrison AS, Showalter TN. Radiotherapy protocol deviations and clinical outcomes: a meta-analysis of cooperative group clinical trials. J Natl Cancer Inst. 2013; 105:387–93.
Article18. Weber DC, Tomsej M, Melidis C, Hurkmans CW. QA makes a clinical trial stronger: evidence-based medicine in radiation therapy. Radiother Oncol. 2012; 105:4–8.
Article19. Fairchild A, Straube W, Laurie F, Followill D. Does quality of radiation therapy predict outcomes of multicenter cooperative group trials? A literature review. Int J Radiat Oncol Biol Phys. 2013; 87:246–60.
Article20. Gondi V, Tome WA, Rowley H, Mehta MP. Hippocampal contouring: a contouring atlas for RTOG 0933 [Internet]. Bethesda, MD: RTOG Foundation;2010. [cited 2018 Sep 1]. Available from: http://www.rtog.org.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accelerated Fractionation In The Treatment of Brain Metastasis From Non-Small Cell Carcinoma of The Lung
- Radiotherapy of Brain Metastases from Lung Cancer
- Comparison of Stereotactic Radiosurgery and Whole Brain Radiotherapy in Patients with Four or More Brain Metastases
- Prognostic Factors in Patients with Vrain Metastases from Non-Small Cell Lung Carcinoma
- Clinical application of RapidArc volumetric modulated arc therapy as a component in whole brain radiation therapy for poor prognostic, four or more multiple brain metastases