J Periodontal Implant Sci.
2019 Jun;49(3):185-192. 10.5051/jpis.2019.49.3.185.
Effect of initial placement level and wall thickness on maintenance of the marginal bone level in implants with a conical implant-abutment interface: a 5-year retrospective study
- Affiliations
-
- 1Department of Periodontology, Gangnam Severance Dental Hospital, Yonsei University College of Dentistry, Seoul, Korea. periodong@yuhs.ac
- 2Department of Periodontology, Institute of Oral Bioscience, Chonbuk National University School of Dentistry, Jeonju, Korea.
- 3Department of Orthodontics, Gangnam Severance Dental Hospital, Yonsei University College of Dentistry, Seoul, Korea.
- 4Department of Oral and Maxillofacial Surgery, Gangnam Severance Dental Hospital, Yonsei University College of Dentistry, Seoul, Korea.
- KMID: 2454088
- DOI: http://doi.org/10.5051/jpis.2019.49.3.185
Abstract
- PURPOSE
Implant wall thickness and the height of the implant-abutment interface are known as factors that affect the distribution of stress on the marginal bone around the implant. The goal of this study was to evaluate the long-term effects of supracrestal implant placement and implant wall thickness on maintenance of the marginal bone level.
METHODS
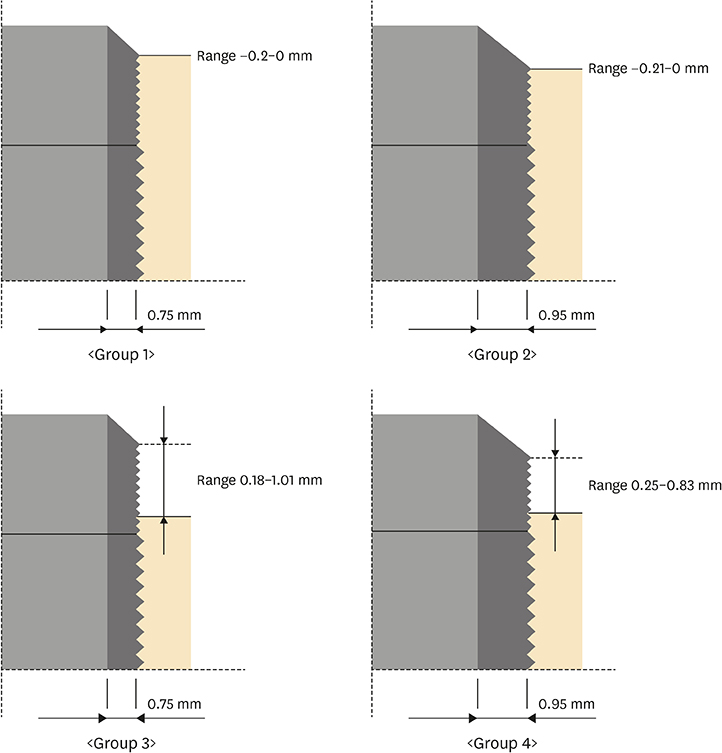
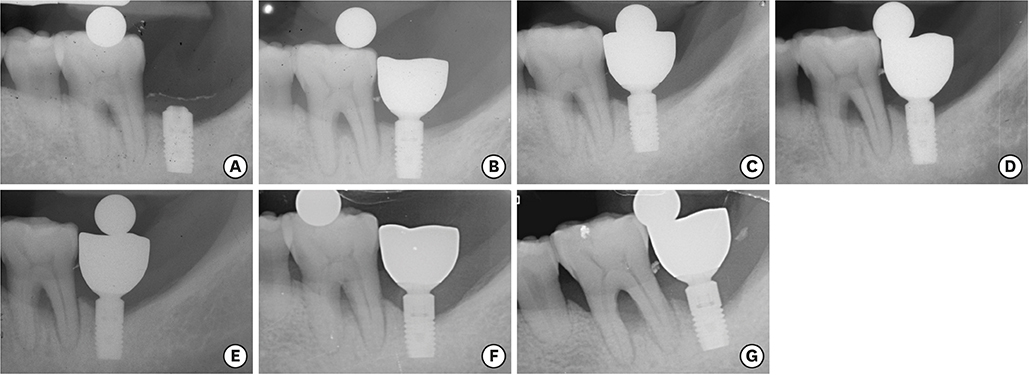
In this retrospective study, 101 patients with a single implant were divided into the following 4 groups according to the thickness of the implant wall and the initial implant placement level immediately after surgery: 0.75 mm wall thickness, epicrestal position; 0.95 mm wall thickness, epicrestal position; 0.75 mm wall thickness, supracrestal position; 0.95 mm wall thickness, supracrestal position. The marginal bone level change was assessed 1 day after implant placement, immediately after functional loading, and 1 to 5 years after prosthesis delivery. To compare the marginal bone level change, repeated-measures analysis of variance was used to evaluate the statistical significance of differences within groups and between groups over time. Pearson correlation coefficients were also calculated to analyze the correlation between implant placement level and bone loss.
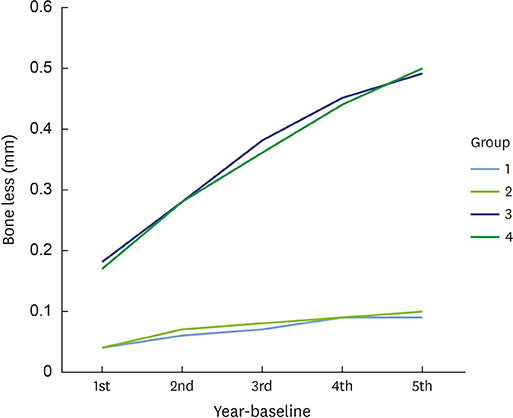
RESULTS
Statistically significant differences in bone loss among the 4 groups (P<0.01) and within each group over time (P<0.01) were observed. There was no significant difference between the groups with a wall thickness of 0.75 mm and 0.95 mm. In a multiple comparison, the groups with a supracrestal placement level showed greater bone loss than the epicrestal placement groups. In addition, a significant correlation between implant placement level and marginal bone loss was observed.
CONCLUSIONS
The degree of bone resorption was significantly higher for implants with a supracrestal placement compared to those with an epicrestal placement.
MeSH Terms
Figure
Reference
-
1. Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: myth or science? J Periodontol. 2002; 73:322–333.
Article2. Hansson S. A conical implant-abutment interface at the level of the marginal bone improves the distribution of stresses in the supporting bone. An axisymmetric finite element analysis. Clin Oral Implants Res. 2003; 14:286–293.
Article3. Hansson S. The implant neck: smooth or provided with retention elements. A biomechanical approach. Clin Oral Implants Res. 1999; 10:394–405.
Article4. Mailth G, Stoiber B, Watzek G, Matejka M. Bone resorption at the entry of osseointegrated implants--a biomechanical phenomenon. Finite element study. Z Stomatol. 1989; 86:207–216.5. Qian L, Todo M, Matsushita Y, Koyano K. Effects of implant diameter, insertion depth, and loading angle on stress/strain fields in implant/jawbone systems: finite element analysis. Int J Oral Maxillofac Implants. 2009; 24:877–886.6. Froum SJ, Cho SC, Suzuki T, Yu P, Corby P, Khouly I. Epicrestal and subcrestal placement of platform-switched implants: 18 month-result of a randomized, controlled, split-mouth, prospective clinical trial. Clin Oral Implants Res. 2018; 29:353–366.
Article7. Geramy A, Morgano SM. Finite element analysis of three designs of an implant-supported molar crown. J Prosthet Dent. 2004; 92:434–440.
Article8. Petrie CS, Williams JL. Comparative evaluation of implant designs: influence of diameter, length, and taper on strains in the alveolar crest. A three-dimensional finite-element analysis. Clin Oral Implants Res. 2005; 16:486–494.
Article9. Geng JP, Tan KB, Liu GR. Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent. 2001; 85:585–598.
Article10. Moriwaki H, Yamaguchi S, Nakano T, Yamanishi Y, Imazato S, Yatani H. Influence of implant length and diameter, bicortical anchorage, and sinus augmentation on bone stress distribution: three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2016; 31:e84–e91.
Article11. Schwarz F, Alcoforado G, Nelson K, Schaer A, Taylor T, Beuer F, et al. Impact of implant-abutment connection, positioning of the machined collar/microgap, and platform switching on crestal bone level changes. Camlog Foundation Consensus Report. Clin Oral Implants Res. 2014; 25:1301–1303.
Article12. Moergel M, Rocha S, Messias A, Nicolau P, Guerra F, Wagner W. Radiographic evaluation of conical tapered platform-switched implants in the posterior mandible: 1-year results of a two-center prospective study. Clin Oral Implants Res. 2016; 27:686–693.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Marginal bone level changes in association with different vertical implant positions: a 3-year retrospective study
- Concept and application of implant connection systems: Part I. Placement and restoration of internal conical connection implant
- A comparative study of the 1-piece and 2-piece conical abutment joint: the strength and the fatigue resistance
- Concept and application of implant connection systems: Part II. Placement and restoration of external connection implant and tissue level implant
- Effect of a counter-torque device and the internal hexagon of abutment on the tightening torque transmitted to the implant