Clin Nutr Res.
2019 Jul;8(3):171-183. 10.7762/cnr.2019.8.3.171.
Importance of Adherence to Personalized Diet Intervention in Obesity Related Metabolic Improvement in Overweight and Obese Korean Adults
- Affiliations
-
- 1Department of Food Science and Nutrition, Dong-A University, Busan 49315, Korea. oykim@dau.ac.kr
- 2Center for Silver-targeted Biomaterials, Brain Busan 21 Plus Program, Dong-A University, Busan 49315, Korea.
- 3Institute of Health Insurance and Clinical Research, National Health Insurance Service Ilsan Hospital, Goyang 10444, Korea.
- 4Busan Cardiocerebrovascular Center, Dong-A University Hospital, College of Medicine, Busan 49201, Korea.
- KMID: 2454075
- DOI: http://doi.org/10.7762/cnr.2019.8.3.171
Abstract
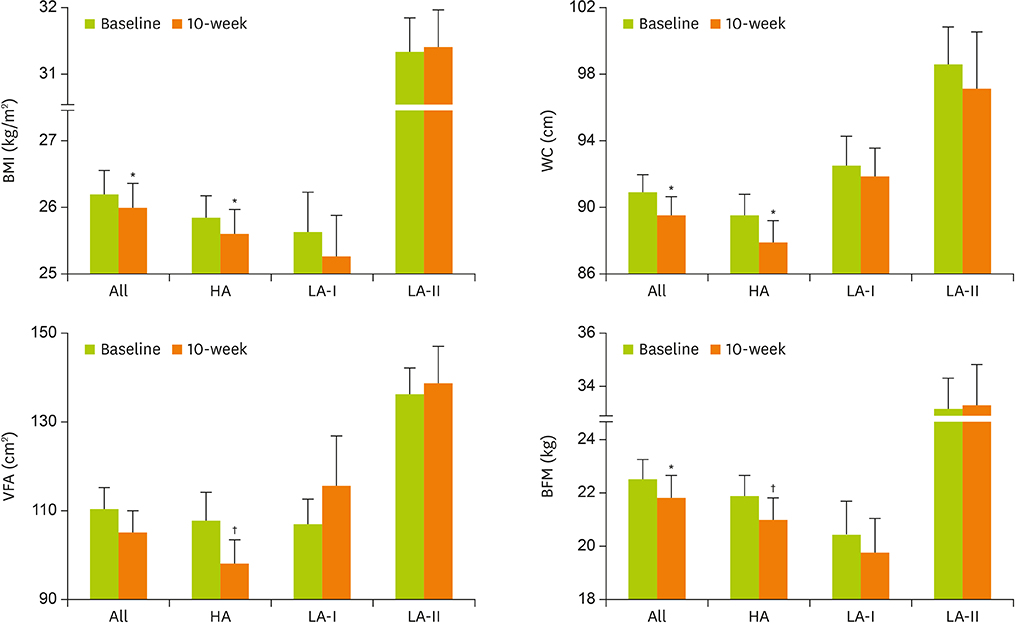
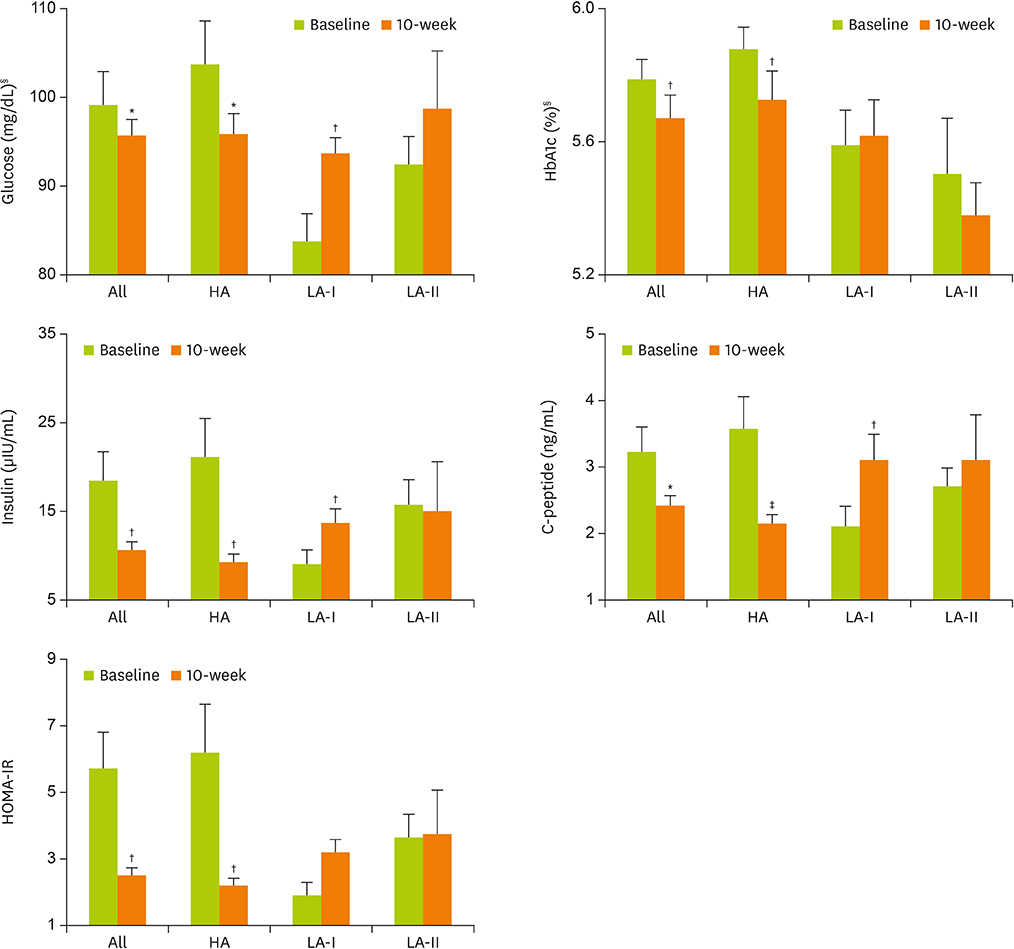
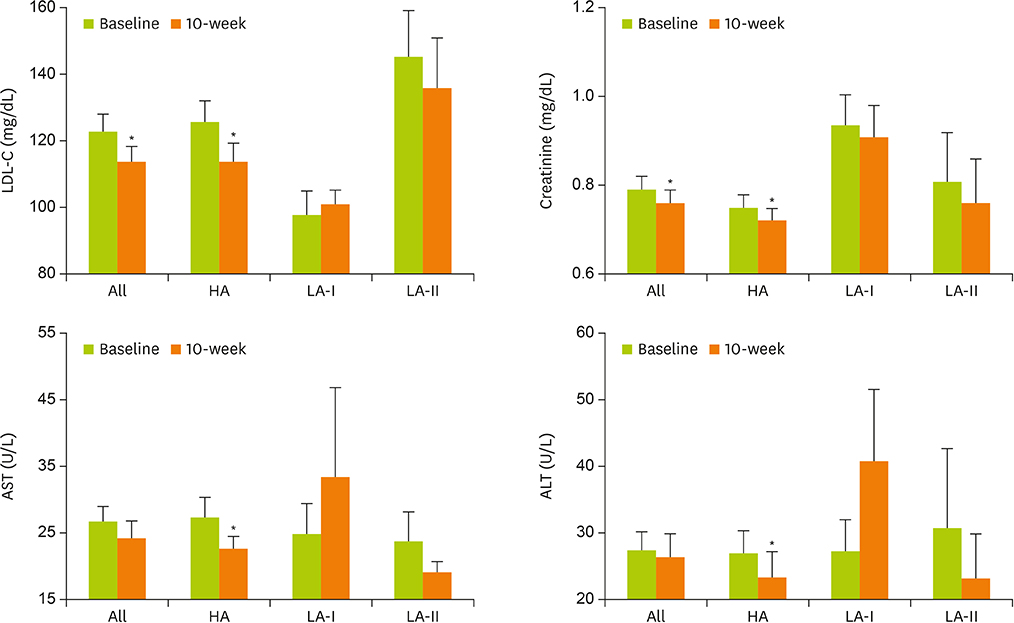
- We investigated weight loss effect of personalized diet education in overweight/obese Korean adults. Overweight/obese Korean adults (body mass index [BMI] ≥ 23 kg/m2 or waist circumference [WC] ≥ 90 cm for men, ≥ 85 cm for women) were recruited, and 40 participants who completed the 10-week intervention were finally included in the analyses. At first visit, study participants (small group with individual counseling) were educated for optimal diet by clinical dietitian, and checked for their compliance through telephone/text message every 1-2 week during the intervention. Anthropometric and biochemical parameters and dietary intake were investigated. Body weight, BMI, WC, and body fat mass were significantly reduced in whole participants. Hemoglobin A1c, insulin, and low-density lipoprotein cholesterol were also significantly decreased after the intervention. Total energy intake (EI) during the intervention was not significantly decreased compared to the baseline value, but the proportions of energy derived from macronutrients were within the ranges recommended by 2015 Dietary Reference Intake for Koreans. Based on actual EI, participants were classified into high-adherence (HA) (prescribed EI ± 25%, n = 29), low-adherence I (LA-I) (< 75% of prescribed EI, n = 7), and low-adherence II (LA-II) group (> 125% of prescribed EI, n = 4). Only HA group showed significant improvements in anthropometric parameters, glycemic control and lipid profile. Interestingly, LA-I group showed significant increases in glucose, insulin, C-peptide and insulin resistance. In conclusion, a shift from overweight/obesity to healthy weight can be accomplished by high adherence to personalized diet modification, not by EI reduction.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. WHO obesity and overweight fact sheet. No. 311. Geneva: World Health Organization;2016.2. Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015; 33:673–689.
Article3. Bhupathiraju SN, Hu FB. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016; 118:1723–1735.
Article4. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2017: Korea National Health and Nutrition Examination Survey (KNHANES VII-2). Cheongju: Korea Centers for Disease Control and Prevention;2018.5. Organization for Economic Cooperation and Development (OECD). Obesity update 2017. Paris: OECD;2017.6. McArdle MA, Finucane OM, Connaughton RM, McMorrow AM, Roche HM. Mechanisms of obesity-induced inflammation and insulin resistance: insights into the emerging role of nutritional strategies. Front Endocrinol (Lausanne). 2013; 4:52.
Article7. Arnold M, Leitzmann M, Freisling H, Bray F, Romieu I, Renehan A, Soerjomataram I. Obesity and cancer: an update of the global impact. Cancer Epidemiol. 2016; 41:8–15.
Article8. Alegría Ezquerra E, Castellano Vázquez JM, Alegría Barrero A. Obesity, metabolic syndrome and diabetes: cardiovascular implications and therapy. Rev Esp Cardiol. 2008; 61:752–764.
Article9. Meldrum DR, Morris MA, Gambone JC. Obesity pandemic: causes, consequences, and solutions-but do we have the will? Fertil Steril. 2017; 107:833–839.
Article10. Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017; 376:254–266.
Article11. Webb VL, Wadden TA. Intensive lifestyle intervention for obesity: principles, practices, and results. Gastroenterology. 2017; 152:1752–1764.
Article12. Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016; 387:1947–1956.
Article13. Fock KM, Khoo J. Diet and exercise in management of obesity and overweight. J Gastroenterol Hepatol. 2013; 28:Suppl 4. 59–63.
Article14. Contento IR. Nutrition education: linking research, theory, and practice. Asia Pac J Clin Nutr. 2008; 17:Suppl 1. 176–179.15. Wang H, Song Z, Ba Y, Zhu L, Wen Y. Nutritional and eating education improves knowledge and practice of patients with type 2 diabetes concerning dietary intake and blood glucose control in an outlying city of China. Public Health Nutr. 2014; 17:2351–2358.
Article16. Yuan C, Lai CW, Chan LW, Chow M, Law HK, Ying M. The effect of diabetes self-management education on body weight, glycemic control, and other metabolic markers in patients with type 2 diabetes mellitus. J Diabetes Res. 2014; 2014:789761.
Article17. Lim HM, Park JE, Choi YJ, Huh KB, Kim WY. Individualized diabetes nutrition education improves compliance with diet prescription. Nutr Res Pract. 2009; 3:315–322.
Article18. Wagner MG, Rhee Y, Honrath K, Blodgett Salafia EH, Terbizan D. Nutrition education effective in increasing fruit and vegetable consumption among overweight and obese adults. Appetite. 2016; 100:94–101.
Article19. Mohammadshahi M, Haidari F, Karandish M, Ebrahimi S, Haghighizadeh MH. A randomized clinical trial of nutrition education for improvement of diet quality and inflammation in Iranian obese women. J Nutr Metab. 2014; 2014:605782.
Article20. Pimentel GD, Portero-McLellan KC, Oliveira EP, Spada AP, Oshiiwa M, Zemdegs JC, Barbalho SM. Long-term nutrition education reduces several risk factors for type 2 diabetes mellitus in Brazilians with impaired glucose tolerance. Nutr Res. 2010; 30:186–190.
Article21. Gibson AA, Sainsbury A. Strategies to improve adherence to dietary weight loss interventions in research and real-world settings. Behav Sci (Basel). 2017; 7:44.
Article22. de Vos BC, Runhaar J, van Middelkoop M, Krul M, Bierma-Zeinstra SM. Long-term effects of a randomized, controlled, tailor-made weight-loss intervention in primary care on the health and lifestyle of overweight and obese women. Am J Clin Nutr. 2016; 104:33–40.
Article23. Marklund M, Magnusdottir OK, Rosqvist F, Cloetens L, Landberg R, Kolehmainen M, Brader L, Hermansen K, Poutanen KS, Herzig KH, Hukkanen J, Savolainen MJ, Dragsted LO, Schwab U, Paananen J, Uusitupa M, Åkesson B, Thorsdottir I, Risérus U. A dietary biomarker approach captures compliance and cardiometabolic effects of a healthy Nordic diet in individuals with metabolic syndrome. J Nutr. 2014; 144:1642–1649.
Article24. Vincent-Baudry S, Defoort C, Gerber M, Bernard MC, Verger P, Helal O, Portugal H, Planells R, Grolier P, Amiot-Carlin MJ, Vague P, Lairon D. The Medi-RIVAGE study: reduction of cardiovascular disease risk factors after a 3-mo intervention with a Mediterranean-type diet or a low-fat diet. Am J Clin Nutr. 2005; 82:964–971.
Article25. Kristensen M, Pelletier X, Ross AB, Thielecke F. A high rate of non-compliance confounds the study of whole grains and weight maintenance in a randomised intervention trial-the case for greater use of dietary biomarkers in nutrition intervention studies. Nutrients. 2017; 9:55.
Article26. Salinardi TC, Batra P, Roberts SB, Urban LE, Robinson LM, Pittas AG, Lichtenstein AH, Deckersbach T, Saltzman E, Das SK. Lifestyle intervention reduces body weight and improves cardiometabolic risk factors in worksites. Am J Clin Nutr. 2013; 97:667–676.
Article27. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.
Article28. Nazare JA, Smith J, Borel AL, Alméras N, Tremblay A, Bergeron J, Poirier P, Després JP. Changes in both global diet quality and physical activity level synergistically reduce visceral adiposity in men with features of metabolic syndrome. J Nutr. 2013; 143:1074–1083.
Article29. Kim J, Bea W, Lee K, Han J, Kim S, Kim M, Na W, Sohn C. Effect of the telephone-delivered nutrition education on dietary intake and biochemical parameters in subjects with metabolic syndrome. Clin Nutr Res. 2013; 2:115–124.
Article30. Arab A, Askari G, Golshiri P, Feizi A, Hekmatnia A, Iraj B, Nourian M. The effect of a lifestyle modification education on adiposity measures in overweight and obese nonalcoholic fatty liver disease patients. Int J Prev Med. 2017; 8:10.
Article31. Pinho CPS, Diniz ADS, Arruda IKG, Leite APDL, Rodrigues IG. Effects of weight loss on adipose visceral and subcutaneous tissue in overweight adults. Clin Nutr. 2018; 37:1252–1258.
Article32. Liu RH, Wharton S, Sharma AM, Ardern CI, Kuk JL. Influence of a clinical lifestyle-based weight loss program on the metabolic risk profile of metabolically normal and abnormal obese adults. Obesity (Silver Spring). 2013; 21:1533–1539.
Article33. Yeo R, Yoon SR, Kim OY. The association between food group consumption patterns and early metabolic syndrome risk in non-diabetic healthy people. Clin Nutr Res. 2017; 6:172–182.
Article34. Jane M, Hagger M, Foster J, Ho S, Kane R, Pal S. Effects of a weight management program delivered by social media on weight and metabolic syndrome risk factors in overweight and obese adults: a randomised controlled trial. PLoS One. 2017; 12:e0178326.
Article35. Mummah S, Robinson TN, Mathur M, Farzinkhou S, Sutton S, Gardner CD. Effect of a mobile app intervention on vegetable consumption in overweight adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2017; 14:125.
Article36. Leung AW, Chan RS, Sea MM, Woo J. An overview of factors associated with adherence to lifestyle modification programs for weight management in adults. Int J Environ Res Public Health. 2017; 14:922.
Article37. Busnello FM, Bodanese LC, Pellanda LC, Santos ZE. Nutritional intervention and the impact on adherence to treatment in patients with metabolic syndrome. Arq Bras Cardiol. 2011; 97:217–224.38. Rodriguez-Cano A, Mier-Cabrera J, Balas-Nakash M, Muñoz-Manrique C, Legorreta-Legorreta J, Perichart-Perera O. Dietary changes associated with improvement of metabolic syndrome components in postmenopausal women receiving two different nutrition interventions. Menopause. 2015; 22:758–764.
Article39. Karintrakul S, Angkatavanich J. A randomized controlled trial of an individualized nutrition counseling program matched with a transtheoretical model for overweight and obese females in Thailand. Nutr Res Pract. 2017; 11:319–326.
Article40. Kim BR, Seo SY, Oh NG, Seo JS. Effect of nutrition counseling program on weight control in obese university students. Clin Nutr Res. 2017; 6:7–17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relative Importance of Fitness and Fatness in Obesity Intervention
- Large for Gestational Age and Obesity-Related Comorbidities
- Changes in body composition, body balance, metabolic parameters and eating behavior among overweight and obese women due to adherence to the Pilates exercise program
- The Effects of a Physical Activity-Behavior Modification Combined Intervention(PABM-intervention) on Metabolic Risk Factors in Overweight and Obese Elementary School Children
- The Parental Control Over Their Child's Weight among Elementary School Children Being Overweight or Obese