J Korean Acad Prosthodont.
2019 Jul;57(3):263-270. 10.4047/jkap.2019.57.3.263.
A noninvasive esthetic treatment of isolated microdontia using new high-translucent cubic-phase zirconia (5Y-PSZ) laminate veneers: A case report
- Affiliations
-
- 1Department of Prosthodontics, Institute of Oral Health Science, Ajou University School of Medicine, Suwon, Republic of Korea. denthk@ajou.ac.kr
- KMID: 2453781
- DOI: http://doi.org/10.4047/jkap.2019.57.3.263
Abstract
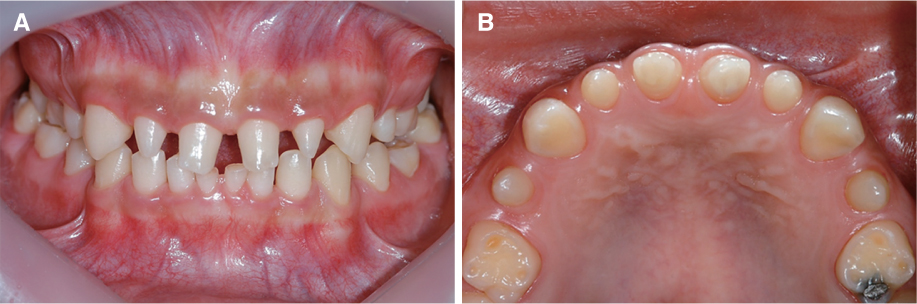
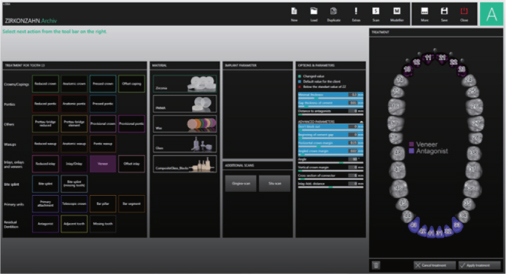
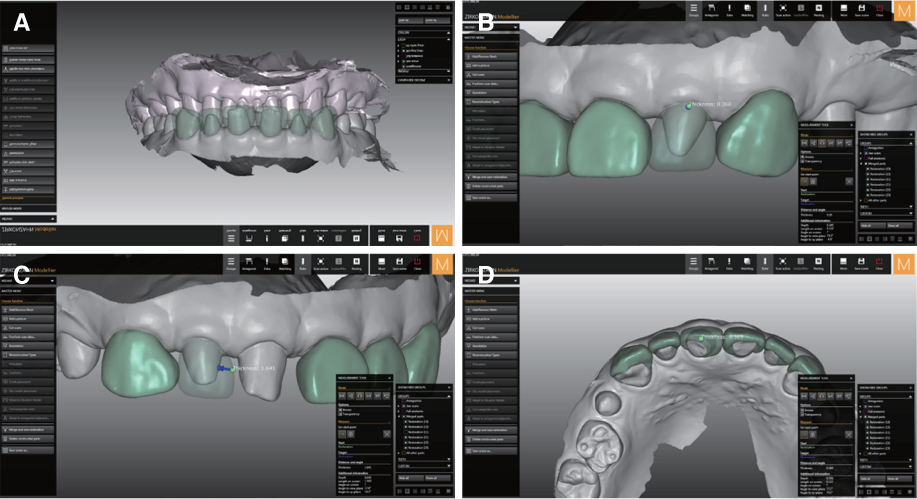
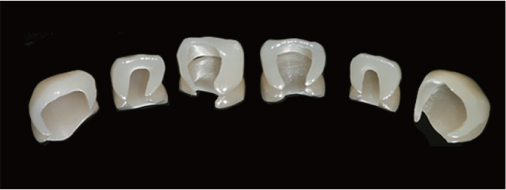
- Current trends in restorative dentistry focus on improving the esthetics and keeping the sound dental tissues as long as possible. The aims of this case report were to describe the successful outcome of cubic-phase zirconia laminate veneers for a patient with isolated microdontia by using a digital workflow, and to describe their clinical implications. A 15-year-old female who had isolated microdontia in combination with spacing visited Ajou University Dental Hospital for esthetic treatment. In this case, 6 maxillary anterior teeth were restored with cubic-phase zirconia laminate veneers without tooth structure removal by using a digital impression, computer-aided design (CAD) software, and computer-aided manufacturing (CAM) procedures. At 6-month follow-up, no distinct mechanical and biological complications were detected and the prostheses exhibited satisfactory esthetics and functions. Due to its favorable tissue responses and enhanced translucency, cubic-phase zirconia can be a suitable strategy for a noninvasive esthetic approach.
Keyword
MeSH Terms
Figure
Reference
-
1. Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. 1st ed. Philadelphia: W. B. Saunders Co.;1958. p. 26.2. Hua F, He H, Ngan P, Bouzid W. Prevalence of peg-shaped maxillary permanent lateral incisors: A meta-analysis. Am J Orthod Dentofacial Orthop. 2013; 144:97–109.
Article3. Arte S, Nieminen P, Apajalahti S, Haavikko K, Thesleff I, Pirinen S. Characteristics of incisor-premolar hypodontia in families. J Dent Res. 2001; 80:1445–1450.
Article4. Mupparapu M, Singer SR. A review of dens invaginatus (dens in dente) in permanent and primary teeth: report of a case in a microdontic maxillary lateral incisor. Quintessence Int. 2006; 37:125–129.5. Hobkirk JA, Goodman JR, Jones SP. Presenting complaints and findings in a group of patients attending a hypodontia clinic. Br Dent J. 1994; 177:337–339.
Article6. Veneziani M. Ceramic laminate veneers: clinical procedures with a multidisciplinary approach. Int J Esthet Dent. 2017; 12:426–448.7. Opdam N, Frankenberger R, Magne P. From ‘Direct versus indirect’ toward an integrated restorative concept in the posterior dentition. Oper Dent. 2016; 41:S27–S34.
Article8. Harada K, Raigrodski AJ, Chung KH, Flinn BD, Dogan S, Mancl LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J Prosthet Dent. 2016; 116:257–263.
Article9. Yan J, Kaizer MR, Zhang Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 2018; 88:170–175.
Article10. Baldissara P, Wandscher VF, Marchionatti AME, Parisi C, Monaco C, Ciocca L. Translucency of IPS e.max and cubic zirconia monolithic crowns. J Prosthet Dent. 2018; 120:269–275.
Article11. Carrabba M, Keeling AJ, Aziz A, Vichi A, Fabian Fonzar R, Wood D, Ferrari M. Translucent zirconia in the ceramic scenario for monolithic restorations: A flexural strength and translucency comparison test. J Dent. 2017; 60:70–76.
Article12. Kwon SJ, Lawson NC, McLaren EE, Nejat AH, Burgess JO. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018; 120:132–137.
Article13. Zhang F, Inokoshi M, Batuk M, Hadermann J, Naert I, Van Meerbeek B, Vleugels J. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater. 2016; 32:e327–e337.
Article14. van Noort R. The future of dental devices is digital. Dent Mater. 2012; 28:3–12.
Article15. Ahlholm P, Sipilä K, Vallittu P, Jakonen M, Kotiranta U. Digital versus conventional impressions in fixed prosthodontics: A review. J Prosthodont. 2018; 27:35–41.
Article16. Chochlidakis KM, Papaspyridakos P, Geminiani A, Chen CJ, Feng IJ, Ercoli C. Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. J Prosthet Dent. 2016; 116:184–190.
Article17. Mostafa NZ, Ruse ND, Ford NL, Carvalho RM, Wyatt CCL. Marginal fit of lithium disilicate crowns fabricated using conventional and digital methodology: A three-dimensional analysis. J Prosthodont. 2018; 27:145–152.
Article18. Friedman MJ. A 15-year review of porcelain veneer failurea clinician's observations. Compend Contin Educ Dent. 1998; 19:625–628.19. Rosenstiel SF, Ward DH, Rashid RG. Dentists' preferences of anterior tooth proportion-a web-based study. J Prosthodont. 2000; 9:123–136.
Article20. Vallittu P, Ozcan M. Clinical guide to principles of fiberreinforced composites in dentistry. Cambridge: W. P. Elsevier Ltd.;2017. p. 18.21. Papia E, Larsson C, du Toit M, Vult von Steyern P. Bonding between oxide ceramics and adhesive cement systems: a systematic review. J Biomed Mater Res B Appl Biomater. 2014; 102:395–413.
Article22. Varga S, Spalj S, Lapter Varga M, Anic Milosevic S, Mestrovic S, Slaj M. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthod. 2011; 33:427–433.
Article23. Yan J, Kaizer MR, Zhang Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 2018; 88:170–175.
Article24. Zhang Y, Kim JW, Bhowmick S, Thompson VP, Rekow ED. Competition of fracture mechanisms in monolithic dental ceramics: flat model systems. J Biomed Mater Res B Appl Biomater. 2009; 88:402–411.
Article25. Nakamura T, Wakabayashi K, Kinuta S, Nishida H, Miyamae M, Yatani H. Mechanical properties of new self-adhesive resin-based cement. J Prosthodont Res. 2010; 54:59–64.
Article26. Shimizu H, Inokoshi M, Takagaki T, Uo M, Minakuchi S. Bonding efficacy of 4-META/MMA-TBB resin to surfacetreated highly translucent dental zirconia. J Adhes Dent. 2018; 20:453–459.27. Yagawa S, Komine F, Fushiki R, Kubochi K, Kimura F, Matsumura H. Effect of priming agents on shear bond strengths of resin-based luting agents to a translucent zirconia material. J Prosthodont Res. 2018; 62:204–209.
Article28. Zhang Y, Lawn BR. Novel zirconia materials in dentistry. J Dent Res. 2018; 97:140–147.
Article29. Kale E, Seker E, Yilmaz B, Özcelik TB. Effect of cement space on the marginal fit of CAD-CAM-fabricated monolithic zirconia crowns. J Prosthet Dent. 2016; 116:890–895.
Article30. McLaren EA, Lawson N, Choi J, Kang J, Trujillo C. New high-translucent cubic-phase-containing zirconia: Clinical and laboratory considerations and the effect of air abrasion on strength. Compend Contin Educ Dent. 2017; 38:e13–e16.31. Inokoshi M, Shimizu H, Nozaki K, Takagaki T, Yoshihara K, Nagaoka N, Zhang F, Vleugels J, Van Meerbeek B, Minakuchi S. Crystallographic and morphological analysis of sandblasted highly translucent dental zirconia. Dent Mater. 2018; 34:508–508.
Article32. Kanemura N, Sano H, Tagami J. Tensile bond strength to and SEM evaluation of ground and intact enamel surfaces. J Dent. 1999; 27:523–530.
Article33. Senawongse P, Sattabanasuk V, Shimada Y, Otsuki M, Tagami J. Bond strengths of current adhesive systems on intact and ground enamel. J Esthet Restor Dent. 2004; 16:107–115.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Esthetic anterior restoration using 3M Lavaâ„¢ Esthetic monolithic zirconia
- Esthetic restorations of maxillary anterior teeth with orthodontic treatment and porcelain laminate veneers: a case report
- Mechanical behavior and microstructural characterization of different zirconia polycrystals in different thicknesses
- An experimental study on hydrothermal degradation of cubic-containing translucent zirconia
- Esthetic improvement in the patient with one missing maxillary central incisor restored with porcelain laminate veneers