Nutr Res Pract.
2019 Jun;13(3):247-255. 10.4162/nrp.2019.13.3.247.
Performance of mid-upper arm circumference to diagnose acute malnutrition in a cross-sectional community-based sample of children aged 6–24 months in Niger
- Affiliations
-
- 1Department of Public Health Sciences, Karolinska Institutet, Solnavägen 1, 171 77 Solna, Sweden. sarah.kate.marshall@outlook.com
- 2Coordination for Health Research. Christus LatAm Hub - Center for Excellence and Innovation, 66260 Monterrey, Nuevo León, Mexico.
- KMID: 2453289
- DOI: http://doi.org/10.4162/nrp.2019.13.3.247
Abstract
- BACKGROUND/OBJECTIVES
Accurate, early identification of acutely malnourished children has the potential to reduce related child morbidity and mortality. The current World Health Organisation (WHO) guidelines classify non-oedematous acute malnutrition among children under five using Mid-Upper Arm Circumference (MUAC) or Weight-for-Height Z-score (WHZ). However, there is ongoing debate regarding the use of current MUAC cut-offs. This study investigates the diagnostic performance of MUAC to identify children aged 6-24 months with global (GAM) or severe acute malnutrition (SAM).
SUBJECTS/METHODS
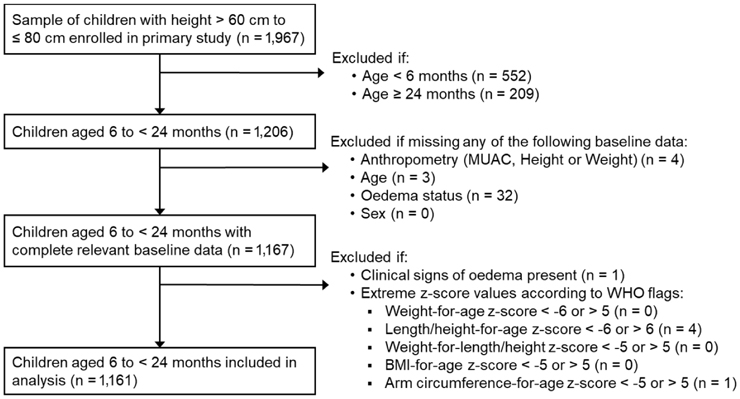
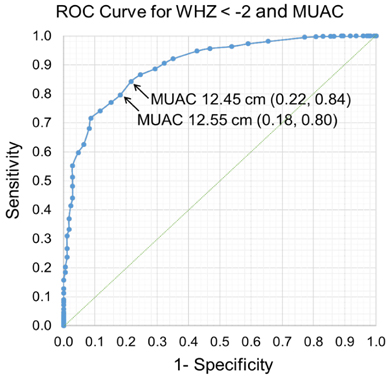
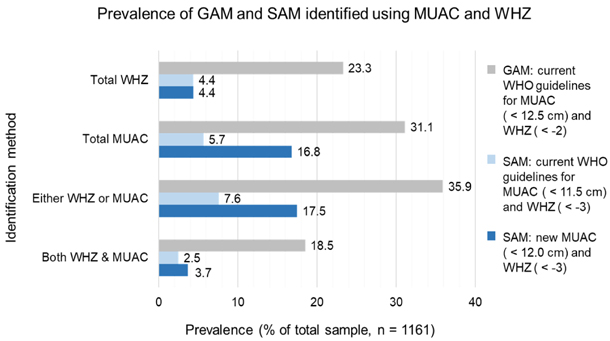
Cross-sectional, secondary data from a community sample of children aged 6-24 months in Niger were used for this study. Children with complete weight, height and MUAC data and without clinical oedema were included. Using WHO guidelines for GAM (WHZ <−2, MUAC < 12.5 cm) and SAM (WHZ <−3, MUAC < 11.5 cm), the sensitivity (Se), specificity (Sp), predictive values, Youden Index and Receiver Operating Characteristic (ROC) curves were calculated for MUAC when compared with the WHZ reference criterion.
RESULTS
Of 1161 children, 23.3% were diagnosed with GAM using WHZ, and 4.4% with SAM. Using current WHO cut-offs, the Se of MUAC to identify GAM was greater than for SAM (79 vs. 57%), yet the Sp was lower (84 vs. 97%). From inspection of the ROC curve and Youden Index, Se and Sp were maximised for MUAC < 12.5 cm to identify GAM (Se 79%, Sp 84%), and MUAC < 12.0 cm to identify SAM (Se 88%, Sp 81%).
CONCLUSIONS
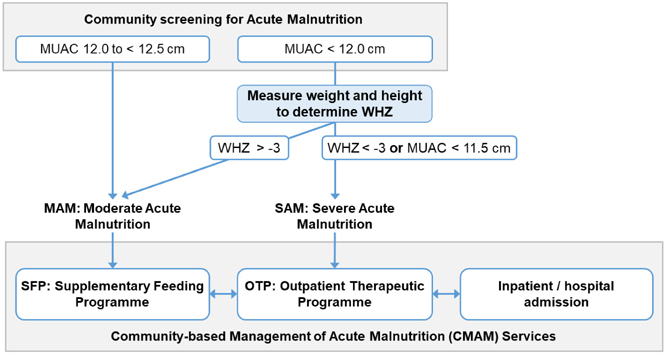
The current MUAC cut-off to identify GAM should continue to be used, but when screening for SAM, a higher cut-off could improve case identification. Community screening for SAM could use MUAC < 12.0 cm followed by appropriate treatment based on either MUAC < 11.5 cm or WHZ <−3, as in current practice. While the practicalities of implementation must be considered, the higher SAM MUAC cut-off would maximise early case-finding of high-risk acutely malnourished children.
MeSH Terms
Figure
Reference
-
1. United Nations Children's Fund. World Health Organization. World Bank Group. Levels and Trends in Child Malnutrition, UNICEF - WHO - World Bank Group Joint Child Malnutrition Estimates. Geneva: World Health Organization;2015.2. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, Uauy R. Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013; 382:427–451.
Article3. World Health Organization. United Nations Children's Fund. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: a Joint Statement. Geneva: World Health Organization;2009.4. World Health Organization. Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children. Geneva: World Health Organization;2013.5. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Geneva: World Health Organization;2006.6. The Sphere Project. Minimum standards in food security and nutrition. The Sphere Project. The Humanitarian Charter and Minimum Standards in Humanitarian Response. Geneva: The Sphere Project;2011. p. 139–238.7. UNHCR The United Nations Refugee Agency. Nutrition needs assessment. UNHCR. UNHCR Emergency Handbook. Geneva: UNHCR The United Nations Refugee Agency;2015. p. 296–298.8. Valid International. Community management of acute malnutrition (CMAM) [Internet]. Oxford: Valid International;2014. cited 2019 March 12. Available from: http://www.validinternational.org.9. Fernández MA, Delchevalerie P, Van Herp M. Accuracy of MUAC in the detection of severe wasting with the new WHO growth standards. Pediatrics. 2010; 126:e195–e201.
Article10. Fiorentino M, Sophonneary P, Laillou A, Whitney S, de Groot R, Perignon M, Kuong K, Berger J, Wieringa FT. Current MUAC cut-offs to screen for acute malnutrition need to be adapted to gender and age: the example of Cambodia. PLoS One. 2016; 11:e0146442.
Article11. Laillou A, Prak S, de Groot R, Whitney S, Conkle J, Horton L, Un SO, Dijkhuizen MA, Wieringa FT. Optimal screening of children with acute malnutrition requires a change in current WHO guidelines as MUAC and WHZ identify different patient groups. PLoS One. 2014; 9:e101159.
Article12. Talapalliwar MR, Garg BS. Diagnostic accuracy of mid-upper arm circumference (MUAC) for detection of severe and moderate acute malnutrition among tribal children in central India. Int J Med Sci Public Health. 2016; 5:1317–1321.
Article13. Dasgupta R, Sinha D, Jain SK, Prasad V. Screening for SAM in the community: is MUAC a simple tool? Indian Pediatr. 2013; 50:154–155.
Article14. Roberfroid D, Huybregts L, Lachat C, Vrijens F, Kolsteren P, Guesdon B. Inconsistent diagnosis of acute malnutrition by weight-for-height and mid-upper arm circumference: contributors in 16 cross-sectional surveys from South Sudan, the Philippines, Chad, and Bangladesh. Nutr J. 2015; 14:86.
Article15. Tripathy JP, Sharma A, Prinja S. Is mid-upper arm circumference alone sufficient to identify severe acute malnutrition correctly? Indian Pediatr. 2016; 53:166–167.16. Briend A, Khara T, Dolan C. Wasting and stunting-similarities and differences: policy and programmatic implications. Food Nutr Bull. 2015; 36:S15–S23.
Article17. Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006; 27:S7–S23.
Article18. Grellety E, Golden MH. Weight-for-height and mid-upper-arm circumference should be used independently to diagnose acute malnutrition: policy implications. BMC Nutr. 2016; 2:10.
Article19. UNICEF. WHO. World Bank. UN-DESA Population Division. Levels and Trends in Child Mortality 2015. Geneva: World Health Organization;2015.20. Institut National de la Statistique (INS) et ICF International. Enquête Démographique et de Santé et à Indicateurs Multiples du Niger 2012. Calverton (MA): INS et ICF International;2013.21. Blackwell N, Myatt M, Allafort-Duverger T, Balogoun A, Ibrahim A, Briend A. Mothers understand and can do it (MUAC): a comparison of mothers and community health workers determining mid-upper arm circumference in 103 children aged from 6 months to 5 years. Arch Public Health. 2015; 73:26.
Article22. Alé FG, Phelan KP, Issa H, Defourny I, Le Duc G, Harczi G, Issaley K, Sayadi S, Ousmane N, Yahaya I, Myatt M, Briend A, Allafort-Duverger T, Shepherd S, Blackwell N. Mothers screening for malnutrition by mid-upper arm circumference is non-inferior to community health workers: results from a large-scale pragmatic trial in rural Niger. Arch Public Health. 2016; 74:38.
Article23. Prudhon C, Langendorf C, Roederer T, Doyon S, Mamaty AA, Woi-Messe L, Manzo ML, de Pee S, Grais RF. Effect of ready-to-use foods for preventing child undernutrition in Niger: analysis of a prospective intervention study over 15 months of follow-up. Matern Child Nutr. 2017; 13.
Article24. Langendorf C, Roederer T, de Pee S, Brown D, Doyon S, Mamaty AA, Touré LW, Manzo ML, Grais RF. Preventing acute malnutrition among young children in crises: a prospective intervention study in Niger. PLoS Med. 2014; 11:e1001714.
Article25. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007; 4:e297.26. USAID Famine Early Warning Systems Network. Niger food security brief [Internet]. Washington, D.C.: USAID Famine Early Warning Systems Network;2014. cited 2019 January 10. Available from: http://www.fews.net/west-africa/niger/food-security-brief/may-2014.27. United Nations Development Programme. Human development index country profile Niger [Internet]. NewYork (NY): United Nations Development Programme;2015. cited 2019 April 4. Available from: http://hdr.undp.org/en/countries/profiles/NER.28. Crowe S, Seal A, Grijalva-Eternod C, Kerac M. Effect of nutrition survey ‘cleaning criteria’ on estimates of malnutrition prevalence and disease burden: secondary data analysis. PeerJ. 2014; 2:e380.
Article29. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Growth Velocity Based on Weight, Length and Head Circumference: Methods and Development. Geneva: World Health Organization;2009.30. World Health Organization. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: World Health Organization;2009.31. Youden WJ. Index for rating diagnostic tests. Cancer. 1950; 3:32–35.
Article32. Fluss R, Faraggi D, Reiser B. Estimation of the Youden index and its associated cutoff point. Biom J. 2005; 47:458–472.
Article33. Park SE, Kim S, Ouma C, Loha M, Wierzba TF, Beck NS. Community management of acute malnutrition in the developing world. Pediatr Gastroenterol Hepatol Nutr. 2012; 15:210–219.
Article34. Myatt M, Duffield A, Seal A, Pasteur F. The effect of body shape on weight-for-height and mid-upper arm circumference based case definitions of acute malnutrition in Ethiopian children. Ann Hum Biol. 2009; 36:5–20.
Article35. Briend A, Maire B, Fontaine O, Garenne M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-five children. Matern Child Nutr. 2012; 8:130–133.
Article36. World Health Organization. Integrated Management of Childhood Illness (IMCI) Chart Booklet. Geneva: World Health Organization;2014.37. Mwangome MK, Berkley JA. The reliability of weight-for-length/height Z scores in children. Matern Child Nutr. 2014; 10:474–480.
Article38. Saeed HA, Mogendi JB, Akparibo R, Kolsteren P. Reliability of mid-upper arm circumference measurements taken by community health nurses. Curr Res Nutr Food Sci. 2015; 3:26–35.
Article39. Mwangome MK, Fegan G, Mbunya R, Prentice AM, Berkley JA. Reliability and accuracy of anthropometry performed by community health workers among infants under 6 months in rural Kenya. Trop Med Int Health. 2012; 17:622–629.
Article40. Phelan KPQ, Lanusse C, van der Kam S, Delchevalerie P, Avril N, Hanson K. Simplifying the response to childhood malnutrition: MSF's experience with MUAC-based (and oedema) programming. Field Exch. 2015; 50:108–116.41. Rutjes AW, Reitsma JB, Di Nisio M, Smidt N, van Rijn JC, Bossuyt PM. Evidence of bias and variation in diagnostic accuracy studies. CMAJ. 2006; 174:469–476.
Article42. World Health Organization. Physical status: the use and interpretation of anthropometry [Internet]. Geneva: World Health Organization;1995. cited 2019 April 4. Available from: http://www.who.int/childgrowth/publications/physical_status/en.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of mid-upper arm circumference in identification, follow-up and discharge of malnourished children during nutrition rehabilitation
- Handgrip Strength and Its Associated Factors among Community-dwelling Elderly in Sri Lanka: A Cross-sectional Study
- Mid-upper-arm circumference as a screening measure for identifying children with elevated body mass index: a study for Pakistan
- A Case of Primary Cutaneous Infection of the Burn Scar by Aspergillus niger
- Status of Early Childhood and Maternal Nutrition in South Korea and North Korea