Pediatr Gastroenterol Hepatol Nutr.
2019 Jul;22(4):377-386. 10.5223/pghn.2019.22.4.377.
Same-Day versus Overnight Observation after Outpatient Pediatric Percutaneous Liver Biopsy: A Retrospective Cohort Study
- Affiliations
-
- 1Department of Medicine, Pediatric Residency Program, Johns Hopkins All Children's Hospital, St. Petersburg, FL, USA.
- 2Division of Pediatric Critical Care Medicine, Johns Hopkins All Children's Hospital, St. Petersburg, FL, USA.
- 3Division of Pediatric Gastroenterology, Johns Hopkins All Children's Hospital, St. Petersburg, FL, USA. mwilsey1@jhmi.edu
- KMID: 2451578
- DOI: http://doi.org/10.5223/pghn.2019.22.4.377
Abstract
- PURPOSE
Percutaneous liver biopsy (PLB), a diagnostic procedure to identify several hepatobiliary disorders, is considered safe with low incidence of associated complications. While postoperative monitoring guidelines are suggested for adults, selection of procedural recovery time for children remains at the discretion of individual operators. We aim to determine if differences exist in frequency of surgical complications, unplanned admissions, and healthcare cost for children undergoing outpatient PLB for cohorts with same-day vs. overnight observation.
METHODS
We performed a retrospective cohort study in children 1 month to 17 years of age undergoing ultrasound-guided PLB from January 2009 to August 2017 at a tertiary care, pediatric referral center. Cohorts were defined by postprocedural observation duration: same-day (≤8 hours) vs. overnight observation. Outcomes included surgical complications, medical interventions, unscheduled hospitalization within 7 days, and total encounter costs.
RESULTS
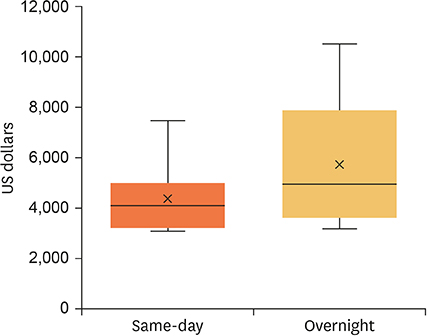
One hundred and twelve children met study criteria of which 18 (16.1%) were assigned to same-day observation. No differences were noted in demographics, anthropometrics, comorbidities, biopsy indications, or preoperative coagulation profiles. No major complications or acute hospitalizations after PLB were observed. Administration of analgesia and fluid boluses were isolated and given within 8 hours. Compared to overnight monitoring, same-day observation accrued less total costs (US $992 less per encounter).
CONCLUSION
Same-day observation after PLB in children appears well-tolerated with only minor interventions and complications observed within 8 hours of procedure. We recommend a targeted risk assessment prior to selection of observation duration. Same-day observation appears an appropriate recovery strategy in otherwise low-risk children undergoing outpatient PLB.
Keyword
MeSH Terms
Figure
Reference
-
1. Bilreiro C, Noruegas MJ, Gonçalves I, Moreira Â. Ultrasound-guided liver biopsies in children: a single-center experience and risk factors for minor bleeding. J Pediatr Gastroenterol Nutr. 2017; 65:137–140.
Article2. Copel L, Sosna J, Kruskal JB, Kane RA. Ultrasound-guided percutaneous liver biopsy: indications, risks, and technique. Surg Technol Int. 2003; 11:154–160.3. Bolia R, Matta J, Malik R, Hardikar W. Outpatient liver biopsy in children: safety, feasibility, and economic impact. J Pediatr Gastroenterol Nutr. 2017; 65:86–88.
Article4. Gonzalez-Vallina R, Alonso EM, Rand E, Black DD, Whitington PF. Outpatient percutaneous liver biopsy in children. J Pediatr Gastroenterol Nutr. 1993; 17:370–375.
Article5. Weigand K, Weigand K. Percutaneous liver biopsy: retrospective study over 15 years comparing 287 inpatients with 428 outpatients. J Gastroenterol Hepatol. 2009; 24:792–799.
Article6. Strassburg CP, Manns MP. Approaches to liver biopsy techniques--revisited. Semin Liver Dis. 2006; 26:318–327.
Article7. Amarapurkar D, Amarapurkar A. Indications of liver biopsy in the era of noninvasive assessment of liver fibrosis. J Clin Exp Hepatol. 2015; 5:314–319.
Article8. Fox VL, Cohen MB, Whitington PF, Colletti RB. Outpatient liver biopsy in children: a medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 1996; 23:213–216.
Article9. Galante D, Pellico G, Federico A, Schiraldi R, Matella M, Milillo R, et al. Postextubation adverse events in children undergoing general anesthesia. Paediatr Anaesth. 2007; 17:192.10. Coté CJ, Wilson S. American Academy of Pediatrics. American Academy of Pediatric Dentistry. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures: update 2016. Pediatrics. 2016; 138:e20161212.
Article11. Dezsőfi A, Baumann U, Dhawan A, Durmaz O, Fischler B, Hadzic N, et al. Liver biopsy in children: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2015; 60:408–420.12. Westheim BH, Østensen AB, Aagenæs I, Sanengen T, Almaas R. Evaluation of risk factors for bleeding after liver biopsy in children. J Pediatr Gastroenterol Nutr. 2012; 55:82–87.
Article13. Govender P, Jonas MM, Alomari AI, Padua HM, Dillon BJ, Landrigan-Ossar MF, et al. Sonography-guided percutaneous liver biopsies in children. AJR Am J Roentgenol. 2013; 201:645–650.
Article14. Amaral JG, Schwartz J, Chait P, Temple M, John P, Smith C, et al. Sonographically guided percutaneous liver biopsy in infants: a retrospective review. AJR Am J Roentgenol. 2006; 187:W644–W649.
Article15. Westheim BH, Aagenæs I, Østensen AB, Sanengen T, Almaas R. Effect of operator experience and frequency of procedure performance on complication rate after ultrasound-guided percutaneous liver biopsies. J Pediatr Gastroenterol Nutr. 2013; 57:638–643.
Article16. Scheimann AO, Barrios JM, Al-Tawil YS, Gray KM, Gilger MA. Percutaneous liver biopsy in children: impact of ultrasonography and spring-loaded biopsy needles. J Pediatr Gastroenterol Nutr. 2000; 31:536–539.
Article17. Sornsakrin M, Helmke K, Briem-Richter A, Ganschow R. Value of ultrasound-guided percutaneous liver biopsy in children following liver transplantation. J Pediatr Gastroenterol Nutr. 2010; 51:635–637.
Article18. Kader HA, Bellah R, Maller ES, Mamula P, Piccoli DA, Markowitz JE. The utility of ultrasound site selection for pediatric percutaneous liver biopsy. J Pediatr Gastroenterol Nutr. 2003; 36:364–367.
Article19. Short SS, Papillon S, Hunter CJ, Stanley P, Kerkar N, Wang L, et al. Percutaneous liver biopsy: pathologic diagnosis and complications in children. J Pediatr Gastroenterol Nutr. 2013; 57:644–648.20. Potter C, Hogan M, Henry-Kendjorsky K, Balint J, Barnard J. Safety of pediatric percutaneous liver biopsy performed by interventional radiologists. J Pediatr Gastroenterol Nutr. 2011; 53:202–206.
Article21. Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 2009; 49:1017–1044.
Article22. Nodarse-Pérez PO, Pérez-Menéndez R, Heredia-Andrade ED, Noa-Pedroso G, Araluce-Cordoví R, Fernández-Sotolongo J. Safety of reducing the recovery time after percutaneous and laparoscopic liver biopsy. Cir Cir. 2016; 84:196–202.
Article23. Banerjee S, Bishop W, Valim C, Mahoney L, Lightdale J. Percutaneous liver biopsy practice patterns among pediatric gastroenterologists in North America. J Pediatr Gastroenterol Nutr. 2007; 45:84–89.
Article24. Garra G, Singer AJ, Taira BR, Chohan J, Cardoz H, Chisena E, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010; 17:50–54.
Article25. Lipscomb J, Yabroff KR, Brown ML, Lawrence W, Barnett PG. Health care costing: data, methods, current applications. Med Care. 2009; 47:S1–6.
Article26. Lauder GR. Total intravenous anesthesia will supercede inhalational anesthesia in pediatric anesthetic practice. Paediatr Anaesth. 2015; 25:52–64.
Article27. Mani V, Morton NS. Overview of total intravenous anesthesia in children. Paediatr Anaesth. 2010; 20:211–222.
Article28. Almeida P, Schreiber RA, Liang J, Mujawar Q, Guttman OR. Clinical characteristics and complications of pediatric liver biopsy: a single centre experience. Ann Hepatol. 2017; 16:797–801.
Article29. Potretzke TA, Saling LJ, Middleton WD, Robinson KA. Bleeding complications after percutaneous liver biopsy: do subscapular lesions pose a higher risk? AJR Am J Roentgenol. 2018; 211:204–210.
Article30. Kitchin DR, Del Rio AM, Woods M, Ludeman L, Hinshaw JL. Percutaneous liver biopsy and revised coagulation guidelines: a 9-year experience. Abdom Radiol (NY). 2018; 43:1494–1501.
Article31. Starczewska MH, Mon W, Shirley P. Anaesthesia in patients with liver disease. Curr Opin Anaesthesiol. 2017; 30:392–398.
Article32. Wasson NR, Deer JD, Suresh S. Anesthetic management of pediatric liver and kidney transplantation. Anesthesiol Clin. 2017; 35:421–438.
Article33. Kamat PP, McCracken CE, Gillespie SE, Fortenberry JD, Stockwell JA, Cravero JP, et al. Pediatric critical care physician-administered procedural sedation using propofol: a report from the Pediatric Sedation Research Consortium Database. Pediatr Crit Care Med. 2015; 16:11–20.
Article34. Tsai TC, Orav EJ, Jha AK. Patient satisfaction and quality of surgical care in US hospitals. Ann Surg. 2015; 261:2–8.
Article35. Nichol JR, Fu R, French K, Momberger J, Handel DA. Association between patient and emergency department operational characteristics and patient satisfaction scores in a pediatric population. Pediatr Emerg Care. 2016; 32:139–141.
Article36. Sochet AA, Cartron AM, Nyhan A, Spaeder MC, Song X, Brown AT, et al. Surgical site infection after pediatric cardiothoracic surgery: impact on hospital cost and length of stay. World J Pediatr Congenit Heart Surg. 2017; 8:7–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety of outpatient ultrasound guided percutaneous liver biopsy as a day care procedure
- A case of intraluminal gallbladder hematoma and subsequent cholecystitis after percutaneous liver biopsy
- A Case of Acute Cholangitis with Intraluminal Gallbladder Hematoma after Percutaneous Liver Biopsy
- A Case of Intraluminal Gallbladder Hematoma after Percutaneous Liver Biopsy
- How Long Should We Monitor the Patient for Bleeding after Percutaneous Renal Biopsy?