J Rheum Dis.
2019 Jul;26(3):211-218. 10.4078/jrd.2019.26.3.211.
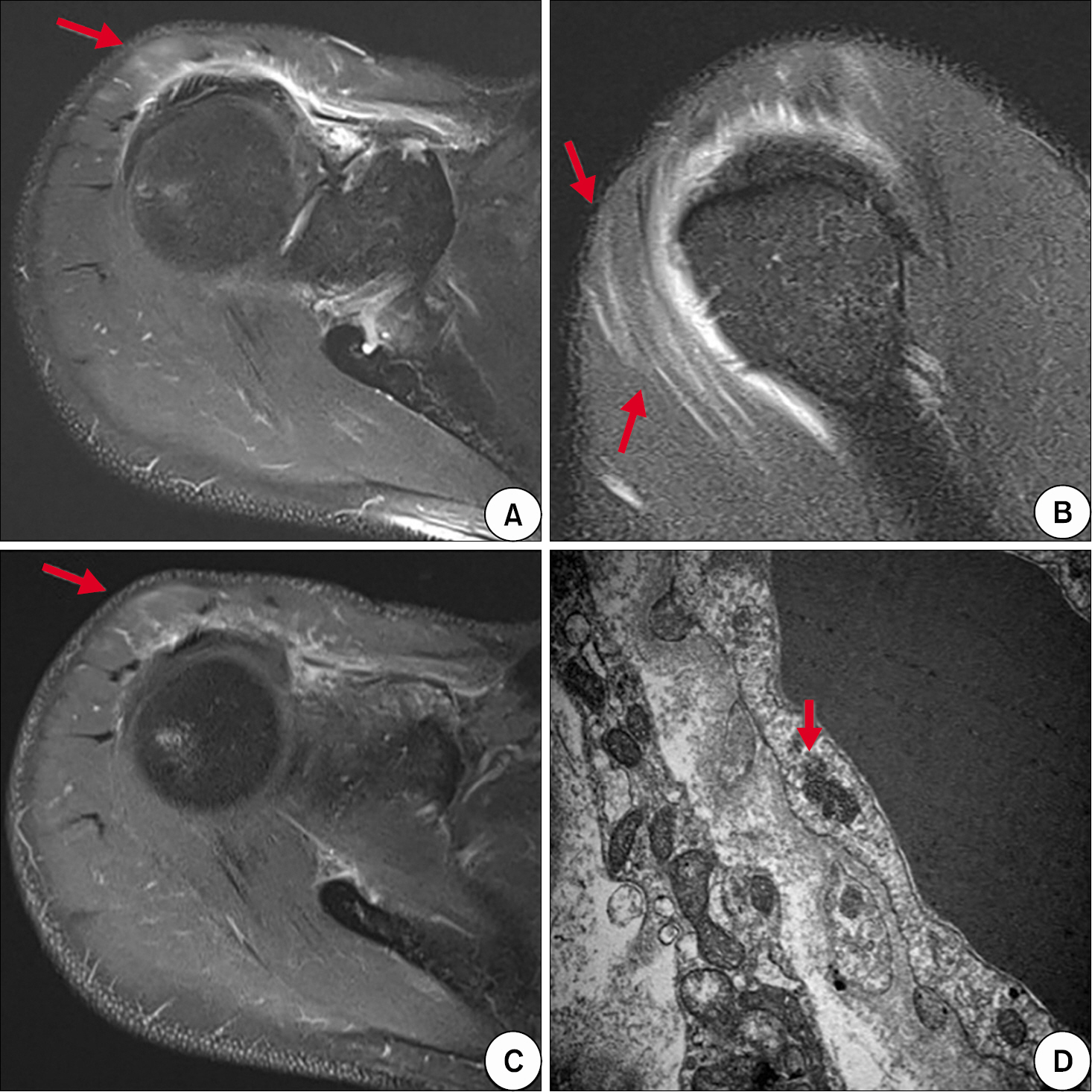
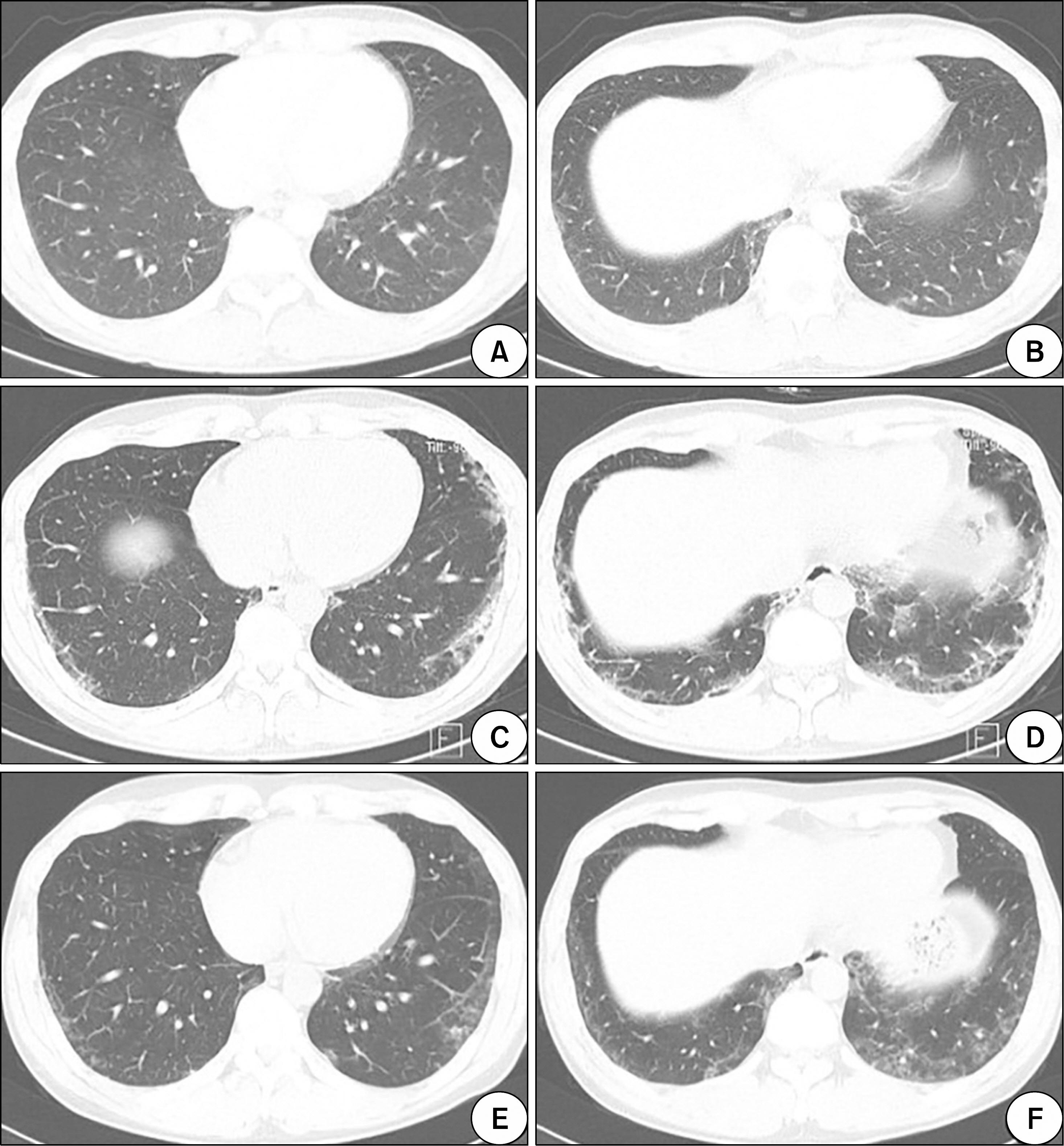
Neuromyositis: A Rare Extramuscular Manifestation of Dermatomyositis
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea. kangsw@cnuh.co.kr
- KMID: 2451514
- DOI: http://doi.org/10.4078/jrd.2019.26.3.211
Abstract
- Dermatomyositis (DM) and polymyositis (PM) are representative idiopathic inflammatory myopathies characterized by symmetric and progressive proximal muscle weakness. Especially, DM is identified by characteristic skin lesions and has many extramuscular manifestations including various cardiac abnormalities, interstitial lung disease, and malignancy. However, involvement of peripheral nervous system in DM/PM is very rare and less known. The term "Neuromyositis" was introduced by Senator in 1893 to describe the concomitant involvement of the peripheral nervous system in DM/PM. Since then, a very few cases of neuromyositis have been reported mainly in the United States and Europe. Therefore, the pathogenetic mechanism and disease progression are unclear. In recent years, a few more cases were reported in Asia, specifically, China and Japan; however, none in Korea. Here, we describe a case of DM-associated neuromyositis in a 42-year-old man in Korea and review previous publications through literature research.
MeSH Terms
Figure
Reference
-
1. Lundberg IE, de Visser M, Werth VP. Classification of myositis. Nat Rev Rheumatol. 2018; 14:269–78.
Article2. Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003; 362:971–82.
Article3. Callen JP. Dermatomyositis. Lancet. 2000; 355:53–7.
Article4. Senator H. Ueber acute polymyositis und neuromyositis. Deutsche Med Wochenschrift. 1893; 19:933–6.5. Onder H, GökcemYı ldız F, Temucin ÇM. Neuromyositis: clinical and electrophysiological study of 8 cases. Global Adv Res J Med Med Sci. 2015; 4:347–50.6. De Visser M, Emslie-Smith AM, Engel AG. Early ultra-structural alterations in adult dermatomyositis. Capillary abnormalities precede other structural changes in muscle. J Neurol Sci. 1989; 94:181–92.7. Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975; 292:344–7.8. Matsui N, Mitsui T, Endo I, Oshima Y, Kunishige M, Matsumoto T. Dermatomyositis with peripheral nervous system involvement: activation of vascular endothelial growth factor (VEGF) and VEGF receptor (VEGFR) in vasculitic lesions. Intern Med. 2003; 42:1233–9.
Article9. Wang Y, Cui LY, Chen L, Liu MS, Qi X, Li BH, et al. Nerve conduction studies in patients with dermatomyositis or polymyositis. Chin Med J (Engl). 2010; 123:523–6.10. Bohan A, Peter JB, Bowman RL, Pearson CM. Computer-assisted analysis of 153 patients with polymyositis and dermatomyositis. Medicine (Baltimore). 1977; 56:255–86.11. Vogelgesang SA, Gutierrez J, Klipple GL, Katona IM. Polyneuropathy in juvenile dermatomyositis. J Rheumatol. 1995; 22:1369–72.12. Nomura M, Watanabe T, Mikami H, Ishikawa H, Yasui K, Yamazaki T, et al. Adult dermatomyositis with severe polyneuropathy: does neuromyositis exist? Neurol Sci. 2010; 31:373–6.
Article13. Nguyen TP, Bangert C, Biliciler S, Athar P, Sheikh K. Dermatomyositis-associated sensory neuropathy: a unifying pathogenic hypothesis. J Clin Neuromuscul Dis. 2014; 16:7–11.14. Irie T, Shigeto H, Koge J, Yamaguchi H, Murai H, Kira JI. Dermatomyositis complicated with asymmetric peripheral neuritis on exacerbation: a case report and literature review. Clin Exp Neuroimmunol. 2016; 7:373–80.
Article15. Cojocaru IM, Socoliuc G, Sapira V, Bastian A, Alexianu M, Moldovan M. Dermatomyositis and polyradiculoneuritis, a rare association. Rom J Intern Med. 2011; 49:217–21.16. França MC Jr, Faria AV, Queiroz LS, Nucci A. Myositis with sensory neuronopathy. Muscle Nerve. 2007; 36:721–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perioperative Anesthetic Management of a Patient with Dermatomyositis
- A Case of Dermatomyositis Associated with Scarring Alopecic Patches
- Amyopathic Dermatomyositis with Interstitial Lung Disease: A Case Report
- Unusual Cutaneous Manifestions of Connective Tissue Disease: II. Multiple Cutaneous Ulcerations in Dermatomyositis
- Clinical Characteristics and Outcomes of Juvenile and Adult Dermatomyositis