J Korean Assoc Oral Maxillofac Surg.
2019 Jun;45(3):167-172. 10.5125/jkaoms.2019.45.3.167.
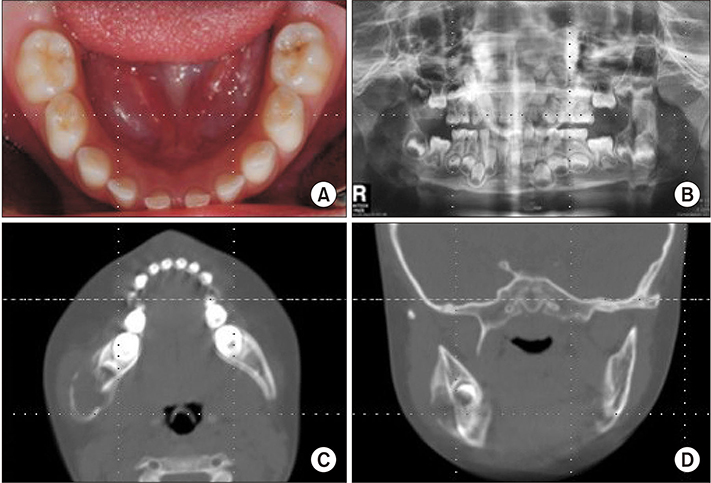
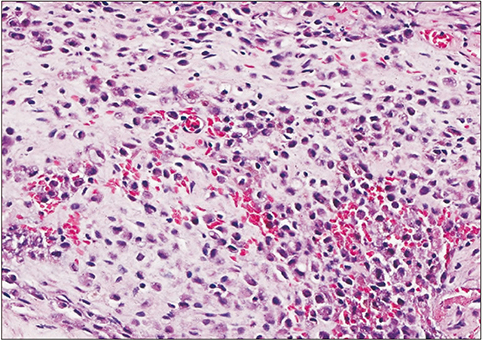
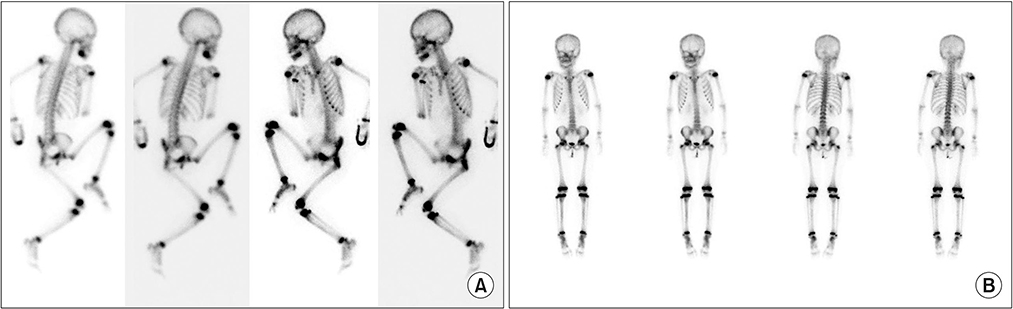
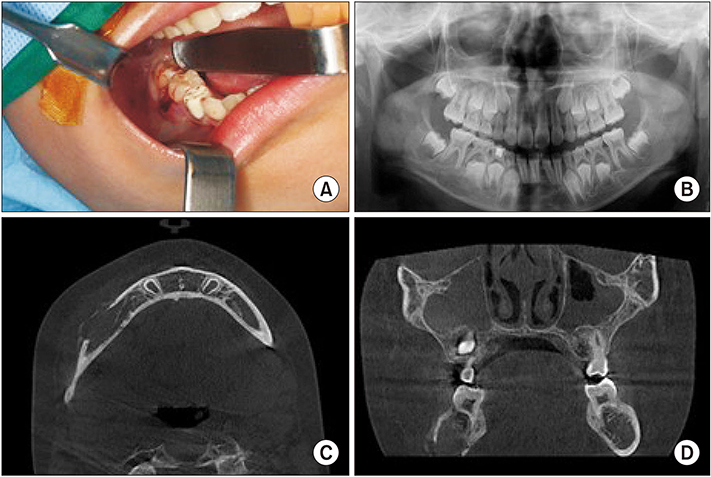
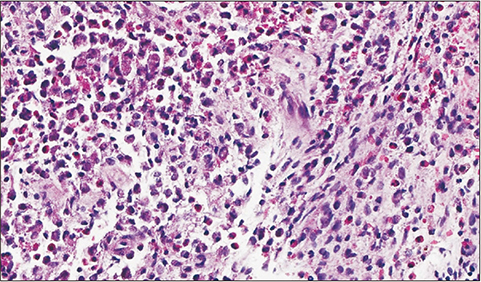
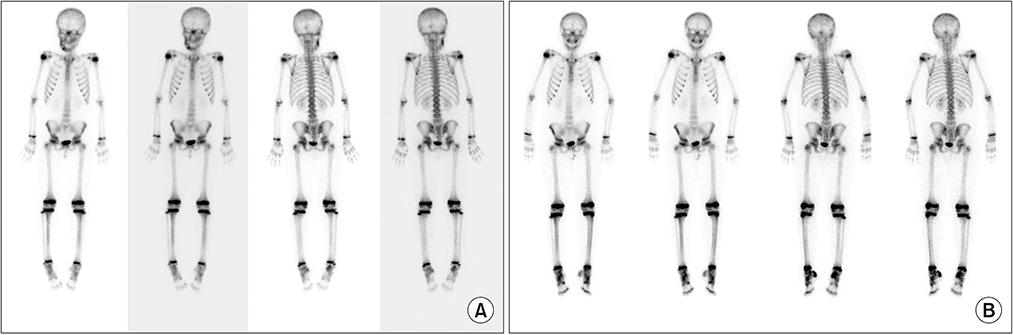
Langerhans cell histiocytosis of the mandible: two case reports and literature review
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Pusan National University, Yangsan, Korea. ljs5332@hanmail.net
- 2Department of Translational Dental Science, School of Dentistry, Pusan National University, Yangsan, Korea.
- KMID: 2451324
- DOI: http://doi.org/10.5125/jkaoms.2019.45.3.167
Abstract
- Langerhans cell histiocytosis (LCH) is a rare disorder characterized by the proliferation of dendritic cells resulting in local or systemic symptoms. The clinical symptoms of patients with Langerhans cell histiocytosis depend on the site and the degree of involvement. This article describes two case histories of unifocal bony Langerhans cell histiocytosis with mandibular involvement and further discusses the appropriate management of such via a review of the literature.
Figure
Reference
-
1. Favara BE, Feller AC, Pauli M, Jaffe ES, Weiss LM, Arico M, et al. Contemporary classification of histiocytic disorders. The WHO Committee On Histiocytic/Reticulum Cell Proliferations. Reclassification Working Group of the Histiocyte Society. Med Pediatr Oncol. 1997; 29:157–166.2. Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, et al. Risk factors for diabetes insipidus in langerhans cell histiocytosis. Pediatr Blood Cancer. 2006; 46:228–233.
Article3. Hartman KS. Histiocytosis X: a review of 114 cases with oral involvement. Oral Surg Oral Med Oral Pathol. 1980; 49:38–54.
Article4. Ardekian L, Peled M, Rosen D, Rachmiel A, Abu el-Naaj I, Laufer D. Clinical and radiographic features of eosinophilic granuloma in the jaws: review of 41 lesions treated by surgery and low-dose radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:238–242.
Article5. Guiglia R, Pizzo G, Aricò M, Maresi E, Compilato D, Campisi G. Bifocal manifestation of eosinophilic granuloma in a pediatric patient. Med Sci Monit. 2009; 15:CS95–CS99.6. Dagenais M, Pharoah MJ, Sikorski PA. The radiographic characteristics of histiocytosis X. A study of 29 cases that involve the jaws. Oral Surg Oral Med Oral Pathol. 1992; 74:230–236.7. Kim BE, Koh KN, Suh JK, Im HJ, Song JS, Lee JW, et al. Korea Histiocytosis Working Party. Clinical features and treatment outcomes of Langerhans cell histiocytosis: a nationwide survey from Korea Histiocytosis Working Party. J Pediatr Hematol Oncol. 2014; 36:125–133.
Article8. Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010; 116:1919–1923.
Article9. Yasko AW, Fanning CV, Ayala AG, Carrasco CH, Murray JA. Percutaneous techniques for the diagnosis and treatment of localized Langerhans-cell histiocytosis (eosinophilic granuloma of bone). J Bone Joint Surg Am. 1998; 80:219–228.
Article10. Karagoz Guzey F, Bas NS, Emel E, Alatas I, Kebudi R. Polyostotic monosystemic calvarial and spinal langerhans' cell histiocytosis treated by surgery and chemotherapy. Pediatr Neurosurg. 2003; 38:206–211.
Article11. Gadner H, Minkov M, Grois N, Pötschger U, Thiem E, Aricò M, et al. Therapy prolongation improves outcome in multisystem Langerhans cell histiocytosis. Blood. 2013; 121:5006–5014.
Article12. Haupt R, Minkov M, Astigarraga I, Schäfer E, Nanduri V, Jubran R, et al. ; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013; 60:175–184.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Langerhans cell histiocytosis of bilateral temporal bone
- Fine Needle Aspiration Cytology of Langerhans Cell Histiocytosis of Mandible: A Case Report
- Spontaneous Pneumothorax due to Pulmonary Invasion in Multisystemic Langerhans Cell Histiocytosis: A case report
- A Case of Orbital Langerhans' cell histiocytosis
- A Case of Gastric Langerhans Cell Histiocytosis Showing Hypertrophic Folds