J Clin Neurol.
2019 Jul;15(3):285-291. 10.3988/jcn.2019.15.3.285.
Clinical Usefulness of Intraoperative Motor-Evoked Potential Monitoring during Temporal Lobe Epilepsy Surgery
- Affiliations
-
- 1Department of Neurology, Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Neurology, Kosin University College of Medicine, Busan, Korea.
- 3Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. daewon@skku.edu
- KMID: 2451110
- DOI: http://doi.org/10.3988/jcn.2019.15.3.285
Abstract
- BACKGROUND AND PURPOSE
We aimed to determine the effectiveness of intraoperative neurophysiological monitoring focused on the transcranial motor-evoked potential (MEP) in patients with medically refractory temporal lobe epilepsy (TLE).
METHODS
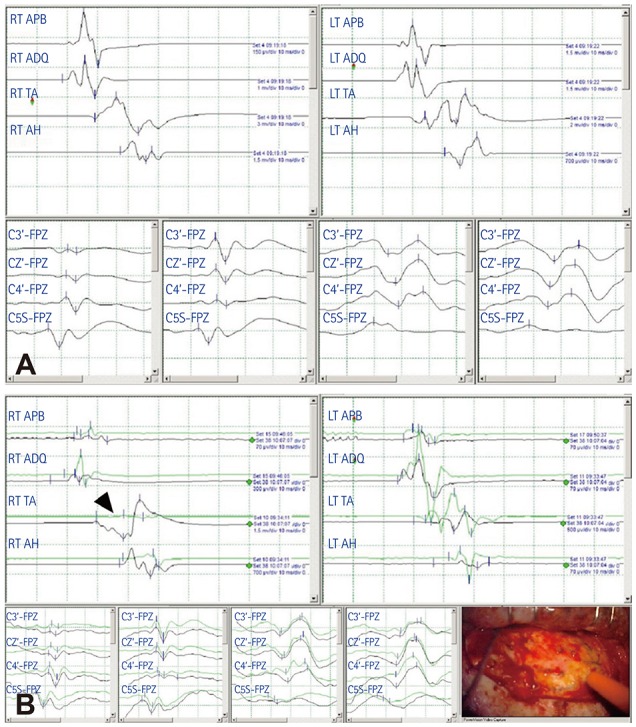
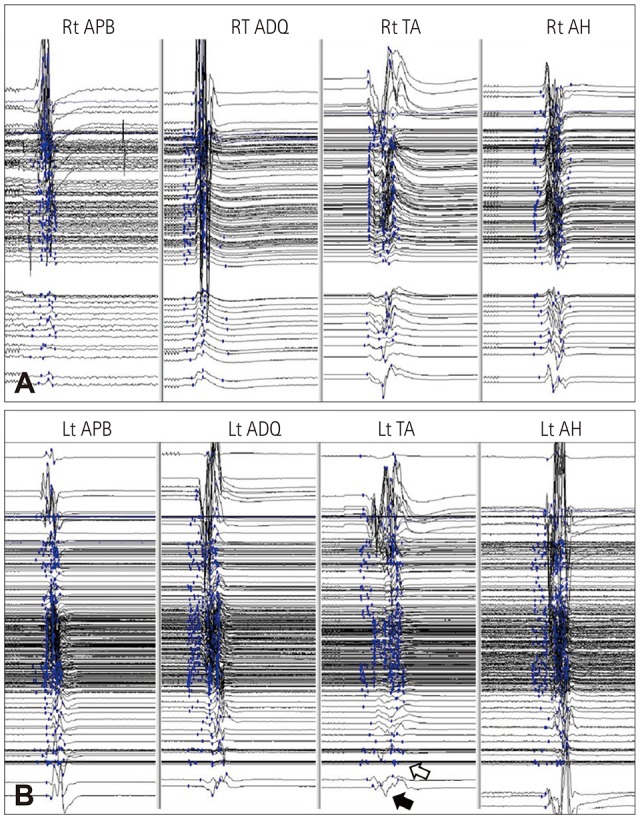
We compared postoperative neurological deficits in patients who underwent TLE surgery with or without transcranial MEPs combined with somatosensory evoked potential (SSEP) monitoring between January 1995 and June 2018. Transcranial motor stimulation was performed using subdermal electrodes, and MEP responses were recorded in the four extremity muscles. A decrease of more than 50% in the MEP or the SSEP amplitudes compared with baseline was used as a warning criterion.
RESULTS
In the TLE surgery group without MEP monitoring, postoperative permanent motor deficits newly developed in 7 of 613 patients. In contrast, no permanent motor deficit occurred in 279 patients who received transcranial MEP and SSEP monitoring. Ten patients who exhibited decreases of more than 50% in the MEP amplitude recovered completely, although two cases showed transient motor deficits that recovered within 3 months postoperatively.
CONCLUSIONS
Intraoperative transcranial MEP monitoring during TLE surgery allowed the prompt detection and appropriate correction of injuries to the motor nervous system or ischemic stroke. Intraoperative transcranial MEP monitoring is a reliable modality for minimizing motor deficits in TLE surgery.
MeSH Terms
Figure
Cited by 1 articles
-
Intraoperative monitoring of somatosensory and visual evoked potentials for detecting posterior cerebral artery infarction during anteromesial temporal resection
Suyeon Seo, Dong Jun Kim, Chae Young Lee
Ann Clin Neurophysiol. 2020;22(2):104-108. doi: 10.14253/acn.2020.22.2.104.
Reference
-
1. Wiebe S, Blume WT, Girvin JP, Eliasziw M. Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001; 345:311–318. PMID: 11484687.
Article2. Engel J Jr. The timing of surgical intervention for mesial temporal lobe epilepsy: a plan for a randomized clinical trial. Arch Neurol. 1999; 56:1338–1341. PMID: 10555652.3. Al-Otaibi F, Baeesa SS, Parrent AG, Girvin JP, Steven D. Surgical techniques for the treatment of temporal lobe epilepsy. Epilepsy Res Treat. 2012; 2012:374848. PMID: 22957228.
Article4. Muzumdar D, Patil M, Goel A, Ravat S, Sawant N, Shah U. Mesial temporal lobe epilepsy–An overview of surgical techniques. Int J Surg. 2016; 36:411–419. PMID: 27773861.5. Georgiadis I, Kapsalaki EZ, Fountas KN. Temporal lobe resective surgery for medically intractable epilepsy: a review of complications and side effects. Epilepsy Res Treat. 2013; 2013:752195. PMID: 24288602.
Article6. Kim SM, Kim SH, Seo DW, Lee KW. Intraoperative neurophysiologic monitoring: basic principles and recent update. J Korean Med Sci. 2013; 28:1261–1269. PMID: 24015028.
Article7. Ichikawa T, Suzuki K, Sasaki T, Matsumoto M, Sakuma J, Oinuma M, et al. Utility and the limit of motor evoked potential monitoring for preventing complications in surgery for cerebral arteriovenous malformation. Neurosurgery. 2010; 67(3 Suppl Operative):ons222–ons228. PMID: 20679926.
Article8. Maruta Y, Fujii M, Imoto H, Nomura S, Tanaka N, Inamura A, et al. Strategies and pitfalls of motor-evoked potential monitoring during supratentorial aneurysm surgery. J Stroke Cerebrovasc Dis. 2016; 25:484–495. PMID: 26639401.
Article9. Neuloh G, Pechstein U, Cedzich C, Schramm J. Motor evoked potential monitoring with supratentorial surgery. Neurosurgery. 2007; 61(1 Suppl):337–346. PMID: 18813156.
Article10. Szelényi A, Hattingen E, Weidauer S, Seifert V, Ziemann U. Intraoperative motor evoked potential alteration in intracranial tumor surgery and its relation to signal alteration in postoperative magnetic resonance imaging. Neurosurgery. 2010; 67:302–313. PMID: 20644415.
Article11. Mathon B, Navarro V, Bielle F, Nguyen-Michel VH, Carpentier A, Baulac M, et al. Complications after surgery for mesial temporal lobe epilepsy associated with hippocampal sclerosis. World Neurosurg. 2017; 102:639–650.e2. PMID: 28389411.
Article12. Girvin JP. Resection of intracranial lesions under local anesthesia. Int Anesthesiol Clin. 1986; 24:133–155.
Article13. Schuele SU, Lüders HO. Intractable epilepsy: management and therapeutic alternatives. Lancet Neurol. 2008; 7:514–524. PMID: 18485315.
Article14. Spencer S, Huh L. Outcomes of epilepsy surgery in adults and children. Lancet Neurol. 2008; 7:525–537. PMID: 18485316.
Article15. Erba G, Winston KR, Adler JR, Welch K, Ziegler R, Hornig GW. Temporal lobectomy for complex partial seizures that began in childhood. Surg Neurol. 1992; 38:424–432. PMID: 1298107.
Article16. Heller AC, Padilla RV, Mamelak AN. Complications of epilepsy surgery in the first 8 years after neurosurgical training. Surg Neurol. 2009; 71:631–637. PMID: 18514273.
Article17. Oertel J, Gaab MR, Runge U, Schroeder HW, Wagner W, Piek J. Neuronavigation and complication rate in epilepsy surgery. Neurosurg Rev. 2004; 27:214–217. PMID: 15048558.
Article18. Kombos T, Picht T, Derdilopoulos A, Suess O. Impact of intraoperative neurophysiological monitoring on surgery of high-grade gliomas. J Clin Neurophysiol. 2009; 26:422–425. PMID: 19952567.
Article19. Talacchi A, Turazzi S, Locatelli F, Sala F, Beltramello A, Alessandrini F, et al. Surgical treatment of high-grade gliomas in motor areas. The impact of different supportive technologies: a 171-patient series. J Neurooncol. 2010; 100:417–426. PMID: 20467787.
Article20. Zhong J, Dujovny M, Perlin AR, Perez-Arjona E, Park HK, Diaz FG. Brain retraction injury. Neurol Res. 2003; 25:831–838. PMID: 14669526.
Article21. Lyon R, Feiner J, Lieberman JA. Progressive suppression of motor evoked potentials during general anesthesia: the phenomenon of “anesthetic fade”. J Neurosurg Anesthesiol. 2005; 17:13–19. PMID: 15632537.22. Abboud T, Huckhagel T, Stork JH, Hamel W, Schwarz C, Vettorazzi E, et al. Why does threshold level change in transcranial motor-evoked potentials during surgery for supratentorial lesions? J Neurosurg Anesthesiol. 2017; 29:393–399. PMID: 27482981.
Article23. MacDonald DB. Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol. 2002; 19:416–429. PMID: 12477987.
Article24. Legatt AD, Emerson RG, Epstein CM, MacDonald DB, Deletis V, Bravo RJ, et al. ACNS guideline: transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol. 2016; 33:42–50. PMID: 26756258.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Detection of the Internal Capsule Infarction by Intraoperative Neuromonitoring in Mesial Temporal Epilepsy Surgery
- Intraoperative monitoring of somatosensory and visual evoked potentials for detecting posterior cerebral artery infarction during anteromesial temporal resection
- Morphological Alterations of Hippocampus in Temporal Lobe Epilepsy: Cell Loss, Synaptic Reorganization, Cell Birth
- Intraoperative Monitoring for Tethered Cord Syndrome Using Somatosensory Evoked Potential and Motor Evoked Potential: Report of three cases
- Intraoperative Monitoring of Hypoglossal Nerve Using Hypoglossal Motor Evoked Potential in Infratentorial Tumor Surgery: A Report of Two Cases