Adv Pediatr Surg.
2019 Jun;25(1):7-13. 10.13029/aps.2019.25.1.7.
Nonoperative Treatment of Appendicitis in the Pediatric Population: Stringent Patient Selection for Successful Application
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. 4hooni@gmail.com
- KMID: 2451062
- DOI: http://doi.org/10.13029/aps.2019.25.1.7
Abstract
- PURPOSE
Although nonoperative treatment of appendicitis (NOTA) in the pediatric population has been well reported recently, patient selection and treatment scheme varies among studies, making it difficult to establish treatment standards for NOTA.
METHODS
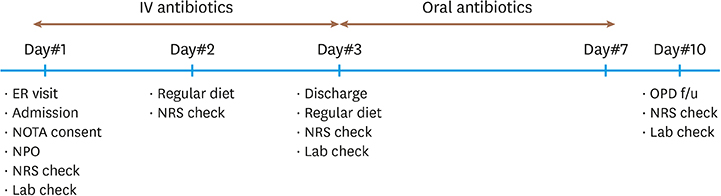
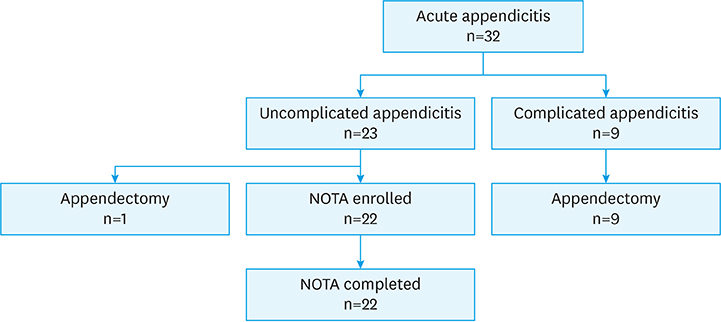
In a single medical center, patients younger than 18 years who were diagnosed with appendicitis: 1) with abdominal pain not exceeding 24 hours, 2) without radiologic evidence of appendicolith or appendiceal perforation or pelvic abscess, and 3) without signs of frank generalized peritonitis were offered NOTA, and their data were prospectively collected.
RESULTS
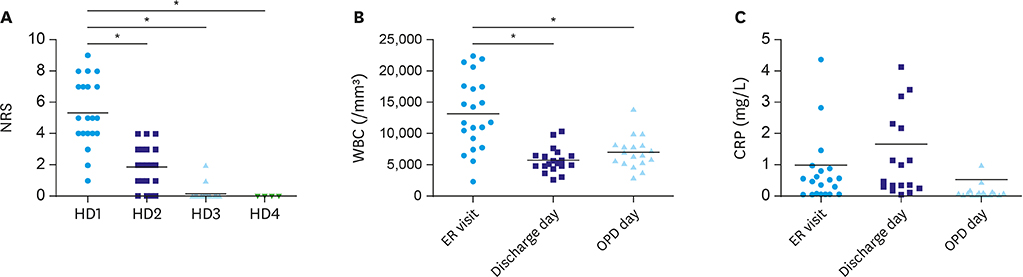
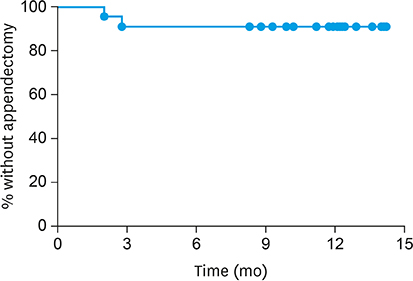
Twenty-two patients with uncomplicated appendicitis agreed to NOTA and were enrolled in the study. The initial success rate (resolution of abdominal pain and hospital discharge without appendectomy) was 100% (22 out of 22 patients). At a median follow-up period of 23.8 months, two patients had recurrence at two and three months after completion of NOTA. These patients underwent laparoscopic appendectomy.
CONCLUSION
Stringent patient selection may be necessary to apply NOTA safely for all children with uncomplicated appendicitis. Further studies concerning patient selection and conformed treatment protocols for NOTA are required.
Keyword
MeSH Terms
Figure
Reference
-
1. Coran AG, Adzick NS. Pediatric surgery. Philadelphia (PA): Elsevier/Saunders;2012.2. Svensson JF, Hall NJ, Eaton S, Pierro A, Wester T. A review of conservative treatment of acute appendicitis. Eur J Pediatr Surg. 2012; 22:185–194.
Article3. Abeş M, Petik B, Kazil S. Nonoperative treatment of acute appendicitis in children. J Pediatr Surg. 2007; 42:1439–1442.
Article4. Armstrong J, Merritt N, Jones S, Scott L, Bütter A. Non-operative management of early, acute appendicitis in children: is it safe and effective? J Pediatr Surg. 2014; 49:782–785.
Article5. Hartwich J, Luks FI, Watson-Smith D, Kurkchubasche AG, Muratore CS, Wills HE, et al. Nonoperative treatment of acute appendicitis in children: a feasibility study. J Pediatr Surg. 2016; 51:111–116.
Article6. Minneci PC, Mahida JB, Lodwick DL, Sulkowski JP, Nacion KM, Cooper JN, et al. Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg. 2016; 151:408–415.
Article7. Svensson JF, Patkova B, Almström M, Naji H, Hall NJ, Eaton S, et al. Nonoperative treatment with antibiotics versus surgery for acute nonperforated appendicitis in children: a pilot randomized controlled trial. Ann Surg. 2015; 261:67–71.8. Tanaka Y, Uchida H, Kawashima H, Fujiogi M, Takazawa S, Deie K, et al. Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J Pediatr Surg. 2015; 50:1893–1897.
Article9. Huang L, Yin Y, Yang L, Wang C, Li Y, Zhou Z. Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: a meta-analysis. JAMA Pediatr. 2017; 171:426–434.10. Xu J, Adams S, Liu YC, Karpelowsky J. Nonoperative management in children with early acute appendicitis: a systematic review. J Pediatr Surg. 2017; 52:1409–1415.
Article11. Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ. Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics. 2017; 139:e20163003.
Article12. Gorter RR, The SM, Gorter-Stam MA, Eker HH, Bakx R, van der Lee JH, et al. Systematic review of nonoperative versus operative treatment of uncomplicated appendicitis. J Pediatr Surg. 2017; 52:1219–1227.
Article13. Lietzén E, Mällinen J, Grönroos JM, Rautio T, Paajanen H, Nordström P, et al. Is preoperative distinction between complicated and uncomplicated acute appendicitis feasible without imaging? Surgery. 2016; 160:789–795.
Article14. Abou-Nukta F, Bakhos C, Arroyo K, et al. Effects of delaying appendectomy for acute appendicitis for 12 to 24 hours. Arch Surg. 2006; 141:504–506.
Article15. Yardeni D, Hirschl RB, Drongowski RA, Teitelbaum DH, Geiger JD, Coran AG. Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night? J Pediatr Surg. 2004; 39:464–469.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antibiotic therapy for appendicitis treatment
- The Feasibility of Nonoperative Management (NOM) in Pediatric Acute Appendicitis in the Era of Coronavirus Disease-2019 (COVID-19)
- To Reduce the Incidence of Postoperative Intraabdominal Abscess, the Application of Nonoperative Management Should be Circumspect Considering Patient Factors and the Nature of Acute Appendicitis
- A Case of Left Ureteral Obstruction due to Acute Appendicitis
- Acute Appendicitis in Children with Acute Leukemia: Experiences of a Single Institution in Korea