Korean Circ J.
2019 Jul;49(7):559-567. 10.4070/kcj.2019.0160.
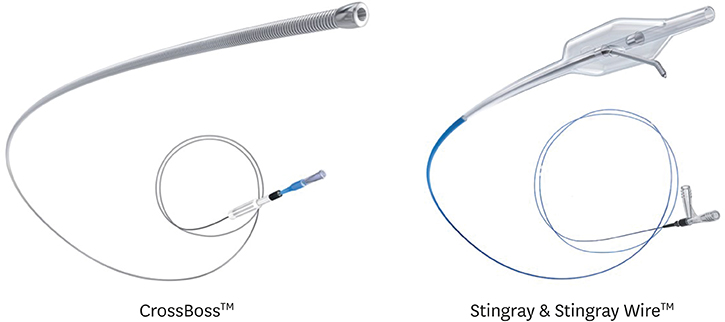
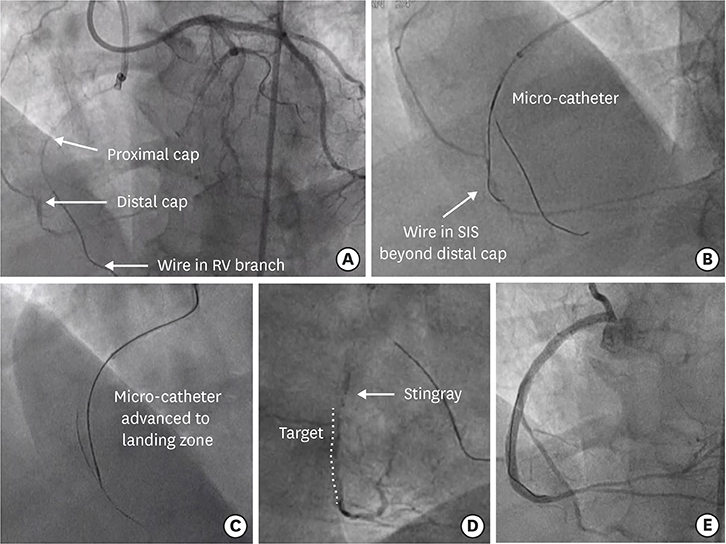
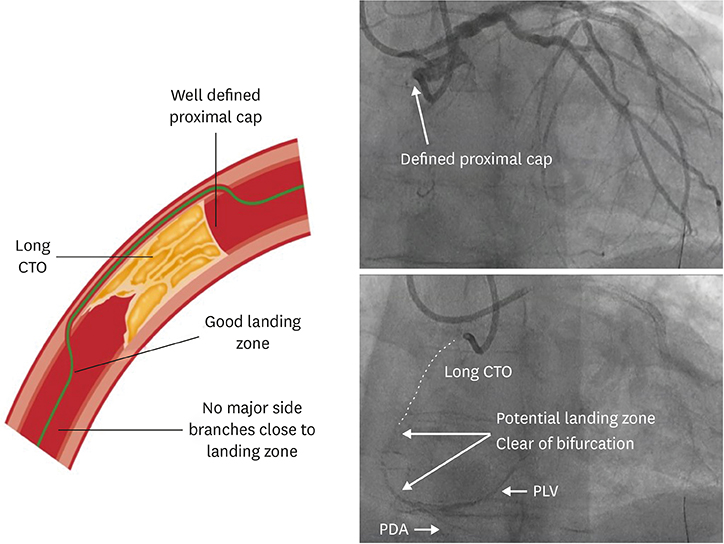
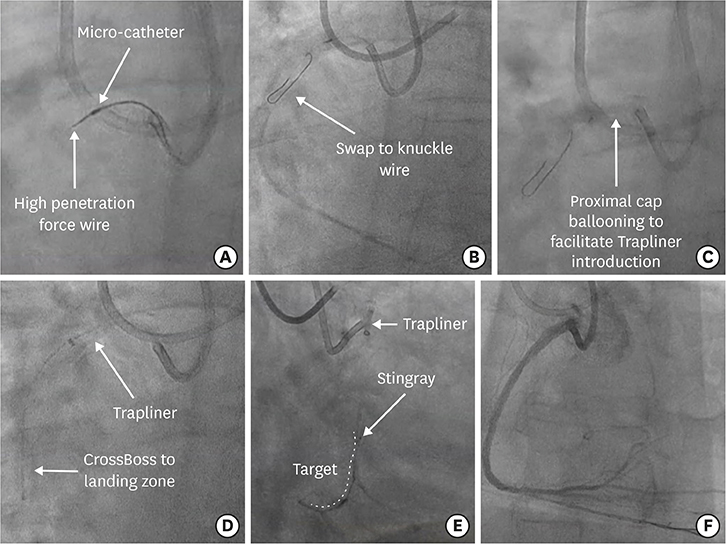
A Technical Focus on Antegrade Dissection and Re-entry for Coronary Chronic Total Occlusions: a Practice Update for 2019
- Affiliations
-
- 1Belfast Health and Social Care Trust, Royal Victoria Hospital, Belfast, United Kingdom. simon.j.walsh@btinternet.com
- 2St George's University Hospital, London, United Kingdom.
- KMID: 2450387
- DOI: http://doi.org/10.4070/kcj.2019.0160
Abstract
- Coronary chronic total occlusions (CTOs) are a commonly encountered lesion. These present in a diverse patient population with variable anatomy. Technical success rates of ~90% are achievable for CTO lesions in centers with appropriate expertise. Many lesions can be crossed with wire-based techniques. However, the most anatomically complex and technically challenging lesions will often require more advanced approaches such as retrograde access and/or the application of blunt dissection techniques in the vessel to safely navigate long and/or ambiguous CTO segments. Retrograde dissection and re-entry (RDR) and antegrade dissection and re-entry (ADR) strategies are often needed to treat such lesions. In many circumstances, ADR offers a safe and efficient means to successfully cross a CTO lesion. Therefore, operators must remain cognizant of the risks and benefits of differing technical approaches during CTO percutaneous coronary intervention, particularly when both ADR and RDR are feasible. This article provides an overview of the ADR technique in addition to updated approaches in contemporary clinical practice.
Keyword
Figure
Cited by 1 articles
-
Before Coronary CTO PCI: Burden or Location?
Woong Gil Choi
Korean Circ J. 2022;52(2):162-165. doi: 10.4070/kcj.2021.0393.
Reference
-
1. Song L, Maehara A, Finn MT, et al. Intravascular ultrasound analysis of intraplaque versus subintimal tracking in percutaneous intervention for coronary chronic total occlusions and association with procedural outcomes. JACC Cardiovasc Interv. 2017; 10:1011–1021.
Article2. Tsujita K, Maehara A, Mintz GS, et al. Intravascular ultrasound comparison of the retrograde versus antegrade approach to percutaneous intervention for chronic total coronary occlusions. JACC Cardiovasc Interv. 2009; 2:846–854.
Article3. Muhammad KI, Lombardi WL, Christofferson R, Whitlow PL. Subintimal guidewire tracking during successful percutaneous therapy for chronic coronary total occlusions: insights from an intravascular ultrasound analysis. Catheter Cardiovasc Interv. 2012; 79:43–48.
Article4. Colombo A, Mikhail GW, Michev I, et al. Treating chronic total occlusions using subintimal tracking and reentry: the STAR technique. Catheter Cardiovasc Interv. 2005; 64:407–411.
Article5. Carlino M, Godino C, Latib A, Moses JW, Colombo A. Subintimal tracking and re-entry technique with contrast guidance: a safer approach. Catheter Cardiovasc Interv. 2008; 72:790–796.6. Galassi AR, Tomasello SD, Costanzo L, et al. Mini-STAR as bail-out strategy for percutaneous coronary intervention of chronic total occlusion. Catheter Cardiovasc Interv. 2012; 79:30–40.
Article7. Godino C, Latib A, Economou FI, et al. Coronary chronic total occlusions: mid-term comparison of clinical outcome following the use of the guided-STAR technique and conventional anterograde approaches. Catheter Cardiovasc Interv. 2012; 79:20–27.8. Valenti R, Vergara R, Migliorini A, et al. Predictors of reocclusion after successful drug-eluting stent-supported percutaneous coronary intervention of chronic total occlusion. J Am Coll Cardiol. 2013; 61:545–550.
Article9. Galassi AR, Boukhris M, Tomasello SD, et al. Long-term clinical and angiographic outcomes of the mini-STAR technique as a bailout strategy for percutaneous coronary intervention of chronic total occlusion. Can J Cardiol. 2014; 30:1400–1406.
Article10. Azzalini L, Dautov R, Brilakis ES, et al. Procedural and longer-term outcomes of wire- versus device-based antegrade dissection and re-entry techniques for the percutaneous revascularization of coronary chronic total occlusions. Int J Cardiol. 2017; 231:78–83.
Article11. Whitlow PL, Burke MN, Lombardi WL, et al. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques: results of the FAST-CTOs (Facilitated Antegrade Steering Technique in Chronic Total Occlusions) trial. JACC Cardiovasc Interv. 2012; 5:393–401.12. Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012; 5:367–379.
Article13. Harding SA, Wu EB, Lo S, et al. A new algorithm for crossing chronic total occlusions from the Asia Pacific chronic total occlusion club. JACC Cardiovasc Interv. 2017; 10:2135–2143.
Article14. Maeremans J, Dens J, Spratt JC, et al. Antegrade dissection and reentry as part of the hybrid chronic total occlusion revascularization strategy: a subanalysis of the RECHARGE registry (registry of CrossBoss and hybrid procedures in France, the Netherlands, Belgium and United Kingdom). Circ Cardiovasc Interv. 2017; 10:e004791.
Article15. Maeremans J, Walsh S, Knaapen P, et al. The hybrid algorithm for treating chronic total occlusions in Europe: the RECHARGE registry. J Am Coll Cardiol. 2016; 68:1958–1970.16. Wilson WM, Walsh SJ, Yan AT, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016; 102:1486–1493.
Article17. Tajti P, Karmpaliotis D, Alaswad K, et al. The hybrid approach to chronic total occlusion percutaneous coronary intervention: update from the PROGRESS CTO registry. JACC Cardiovasc Interv. 2018; 11:1325–1335.18. Azzalini L, Dautov R, Brilakis ES, et al. Impact of crossing strategy on midterm outcomes following percutaneous revascularisation of coronary chronic total occlusions. EuroIntervention. 2017; 13:978–985.
Article19. Wilson WM, Walsh SJ, Bagnall A, et al. One-year outcomes after successful chronic total occlusion percutaneous coronary intervention: the impact of dissection re-entry techniques. Catheter Cardiovasc Interv. 2017; 90:703–712.
Article20. Maeremans J, Avran A, Walsh S, et al. One-year clinical outcomes of the hybrid CTO revascularization strategy after hospital discharge: a subanalysis of the multicenter RECHARGE registry. J Invasive Cardiol. 2018; 30:62–70.21. Walsh SJ, Hanratty CG, Spratt JC. Optimal approach to percutaneous intervention for CTO in 2017: a hybrid strategy is now the preferred choice. EuroIntervention. 2017; 12:e1805–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iteration of Reverse Controlled Antegrade and Retrograde Tracking for Coronary Chronic Total Occlusion Intervention: a Current Appraisal
- The Outback(R) LTDtrade mark Catheter: The Novel Re-Entry Technique in Recanalization of Chronic Inflow Occlusion of the Superficial Femoral Arteries in 3 Cases
- Results of percutaneous transluminal coronary angioplasty of chronic total occlusion.
- Procedural and Early Outcomes of Two Re-entry Devices for Subintimal Recanalization of Aortoiliac and Femoropopliteal Chronic Total Occlusions
- Successful Recanalization of a Long Superficial Femoral Artery Occlusion by Retrograde Subintimal Angioplasty After a Failed Antegrade Subintimal Approach