Yonsei Med J.
2015 May;56(3):812-818. 10.3349/ymj.2015.56.3.812.
Predictors of Thyroid Gland Involvement in Hypopharyngeal Squamous Cell Carcinoma
- Affiliations
-
- 1Department of Otorhinolaryngology, Yonsei Head & Neck Cancer Center, Yonsei University College of Medicine, Seoul, Korea. eunchangmd@yuhs.ac
- 2Department of Surgery, Yonsei Head & Neck Cancer Center, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Thyroid Cancer Center, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2450358
- DOI: http://doi.org/10.3349/ymj.2015.56.3.812
Abstract
- PURPOSE
Decision to perform concurrent ipsilateral thyroidectomy on patients with hypopharyngeal cancer is important, and unnecessary thyroidectomy should be avoided if oncologically feasible. We hypothesized that concurrent ipsilateral thyroidectomy is not routinely required to prevent occult metastasis. This study aimed to determine the prevalence of histological thyroid invasion in patients with hypopharyngeal cancer, and to refine the indications for prophylactic ipsilateral thyroidectomy in patients with hypopharyngeal cancer.
MATERIALS AND METHODS
A retrospective review of the medical records from the Department of Otolaryngology at Yonsei University College of Medicine was conducted from January 1994 to December 2009. A total of 49 patients underwent laryngopharyngectomy with thyroidectomy as a primary treatment of hypopharyngeal cancer.
RESULTS
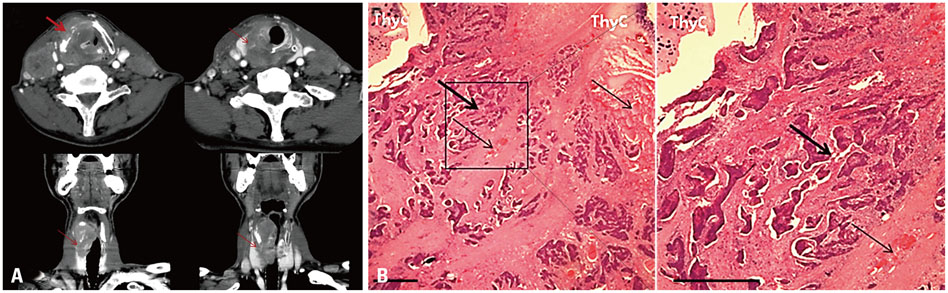
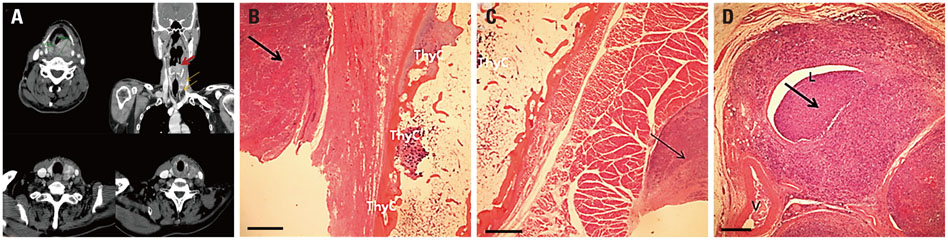
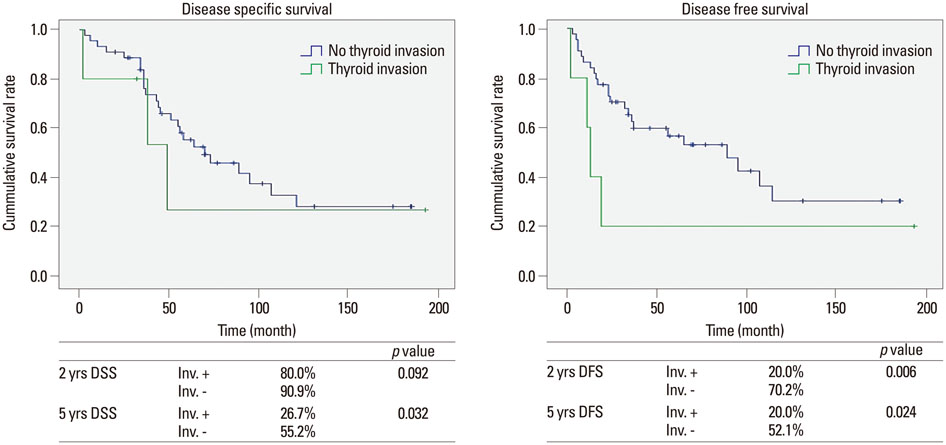
The incidence of thyroid gland involvement was 10.2%. The most common route of invasion was direct extension through the thyroid cartilage. Thyroid cartilage invasion (p=0.034) was the most significant factor associated with thyroid invasion. Disease-specific survival at 5 years was lower in patients with than without thyroid gland invasion (26.7% vs. 55.2%, respectively; p=0.032). Disease-free survival at 5 years was also lower in patients with than without thyroid gland invasion (20.0% vs. 52.1%, respectively; p=0.024).
CONCLUSION
Ipsilateral thyroidectomy in combination with total laryngopharyngectomy is indicated when invasion of the thyroid cartilage is suspected in patients with hypopharyngeal cancer.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Carcinoma, Squamous Cell/epidemiology/pathology/*surgery
Disease-Free Survival
Female
Humans
Hypopharyngeal Neoplasms/epidemiology/pathology/*surgery
Incidence
*Laryngectomy
Male
Middle Aged
Neoplasm Invasiveness
Neoplasms, Second Primary/epidemiology/pathology/surgery
*Pharyngectomy
Predictive Value of Tests
Prevalence
Republic of Korea/epidemiology
Retrospective Studies
Thyroid Gland/*pathology/surgery
Thyroid Neoplasms/epidemiology/*secondary
Thyroidectomy/*methods
Figure
Reference
-
1. Brennan JA, Meyers AD, Jafek BW. The intraoperative management of the thyroid gland during laryngectomy. Laryngoscope. 1991; 101:929–934.
Article2. Biel MA, Maisel RH. Indications for performing hemithyroidectomy for tumors requiring total laryngectomy. Am J Surg. 1985; 150:435–439.
Article3. Sparano A, Chernock R, Laccourreye O, Weinstein G, Feldman M. Predictors of thyroid gland invasion in glottic squamous cell carcinoma. Laryngoscope. 2005; 115:1247–1250.
Article4. Mendelson AA, Al-Khatib TA, Julien M, Payne RJ, Black MJ, Hier MP. Thyroid gland management in total laryngectomy: meta-analysis and surgical recommendations. Otolaryngol Head Neck Surg. 2009; 140:298–305.
Article5. Elliott MS, Odell EW, Tysome JR, Connor SE, Siddiqui A, Jeannon JP, et al. Role of thyroidectomy in advanced laryngeal and pharyngolaryngeal carcinoma. Otolaryngol Head Neck Surg. 2010; 142:851–855.
Article6. Kim JW, Han GS, Byun SS, Lee DY, Cho BH, Kim YM. Management of thyroid gland invasion in laryngopharyngeal cancer. Auris Nasus Larynx. 2008; 35:209–212.
Article7. Turgut OK, Erişen L, Coşkun H, Basut O, Onart S, Hizalan I. Hypothyroidism after primary surgical treatment for laryngeal and hypopharyngeal cancer. Kulak Burun Bogaz Ihtis Derg. 2008; 18:125–130.8. Dadas B, Uslu B, Cakir B, Ozdoğan HC, Caliş AB, Turgut S. Intraoperative management of the thyroid gland in laryngeal cancer surgery. J Otolaryngol. 2001; 30:179–183.
Article9. Montero EH, Trufero JM, Romeo JA, Terré FC. Comorbidity and prognosis in advanced hypopharyngeal-laryngeal cancer under combined therapy. Tumori. 2008; 94:24–29.
Article10. Wagner MM, Curé JK, Caudell JJ, Spencer SA, Nabell LM, Carroll WR, et al. Prognostic significance of thyroid or cricoid cartilage invasion in laryngeal or hypopharyngeal cancer treated with organ preserving strategies. Radiat Oncol. 2012; 7:219.
Article11. Eckel HE, Schröder U, Jungehülsing M, Guntinas-Lichius O, Markitz M, Raunik W. [Surgical treatment options in laryngeal and hypopharyngeal cancer]. Wien Med Wochenschr. 2008; 158:255–263.12. Ceylan A, Köybaşioğlu A, Yilmaz M, Uslu S, Asal K, Inal E. Thyroid gland invasion in advanced laryngeal and hypopharyngeal carcinoma. Kulak Burun Bogaz Ihtis Derg. 2004; 13:9–14.13. Lefebvre JL, Lartigau E. Preservation of form and function during management of cancer of the larynx and hypopharynx. World J Surg. 2003; 27:811–816.
Article14. Aimoni C, Scanelli G, D'agostino L, Pastore A. Thyroid function studies in patients with cancer of the larynx: preliminary evaluation. Otolaryngol Head Neck Surg. 2003; 129:733–738.
Article15. Fagan JJ, Kaye PV. Management of the thyroid gland with laryngectomy for cT3 glottic carcinomas. Clin Otolaryngol Allied Sci. 1997; 22:7–12.
Article16. Herranz J, Sarandeses A, Fernández MF, Barro CV, Vidal JM, Gavilán J. Complications after total laryngectomy in nonradiated laryngeal and hypopharyngeal carcinomas. Otolaryngol Head Neck Surg. 2000; 122:892–898.
Article17. Ozgursoy OB, Jacobs JR. Necessity of routine ipsilateral hemithyroidectomy during laryngopharyngectomy for pyriform sinus cancer. Am J Otolaryngol. 2012; 33:562–564.
Article18. Joshi P, Nair S, Chaturvedi P, Nair D, Shivakumar T, D'Cruz AK. Thyroid gland involvement in carcinoma of the hypopharynx. J Laryngol Otol. 2014; 128:64–67.
Article19. Gilbert J, Forastiere AA. Organ preservation trials for laryngeal cancer. Otolaryngol Clin North Am. 2002; 35:1035–1054.
Article20. Sessions DG. Surgical pathology of cancer of the larynx and hypopharynx. Laryngoscope. 1976; 86:814–839.
Article21. Alexander MV, Zajtchuk JT, Henderson RL. Hypothyroidism and wound healing: occurrence after head and neck radiation and surgery. Arch Otolaryngol. 1982; 108:289–291.
Article22. Chang HJ, Kim KW, Choi SH, Lim S, Park KU, Park do J, et al. Endothelial function is not changed during short-term withdrawal of thyroxine in patients with differentiated thyroid cancer and low cardiovascular risk. Yonsei Med J. 2010; 51:492–498.
Article23. Palmer BV, Gaggar N, Shaw HJ. Thyroid function after radiotherapy and laryngectomy for carcinoma of the larynx. Head Neck Surg. 1981; 4:13–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases with Squamous Cell Carcinoma of the Thyroid Gland
- A Case of Primary Squamous Cell Carcinoma of the Thyroid Gland
- Synchronous thyroid carcinoma and squamous cell carcinoma: A case report
- A Case of Synchronous Squamous Cell and Papillary Carcinoma of the Thyroid Gland
- A Patient with Mixed Squamous Cell and Papillary Thyroid Carcinoma