J Korean Foot Ankle Soc.
2019 Jun;23(2):52-57. 10.14193/jkfas.2019.23.2.52.
Short-Term Surgical Outcome of the Partial Nail Extraction in Ingrown Nail of Military Trainee: Is Matrixectomy Necessary?
- Affiliations
-
- 1Department of Orthopedic Surgery, Armed Forces Daejeon Hospital, Daejeon, Korea.
- 2Department of Orthopedic Surgery, Inje University Seoul Paik Hospital, Seoul, Korea. 20vvin@naver.com
- KMID: 2449672
- DOI: http://doi.org/10.14193/jkfas.2019.23.2.52
Abstract
- PURPOSE
An ingrown nail is common in military trainees who are exposed to highly demanding activities. Although the matrixectomy procedure has been the main treatment modality, several drawbacks may follow after the procedure, such as infection, periostitis, and continued pain that causes a delayed return to duty. This study examined the outcomes of a simple partial nail extraction with the hypothesis that this procedure may bring an earlier return to duty, lower the perioperative complications, and produce a comparable recurrence rate.
MATERIALS AND METHODS
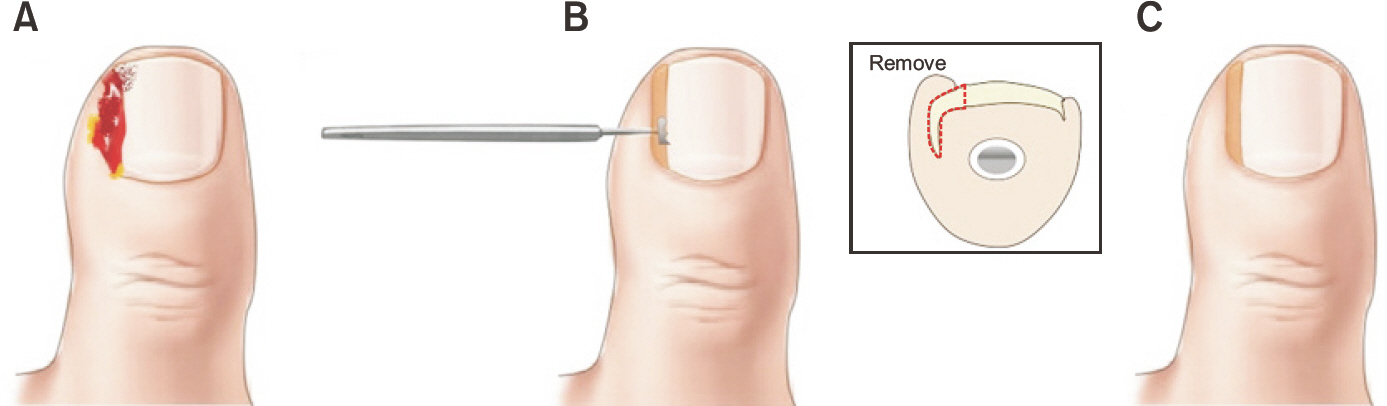
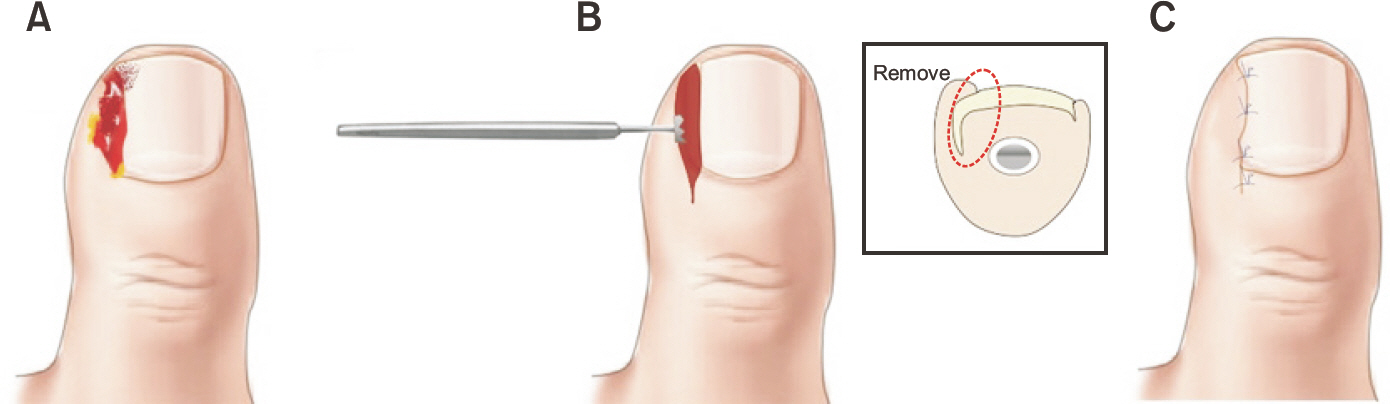
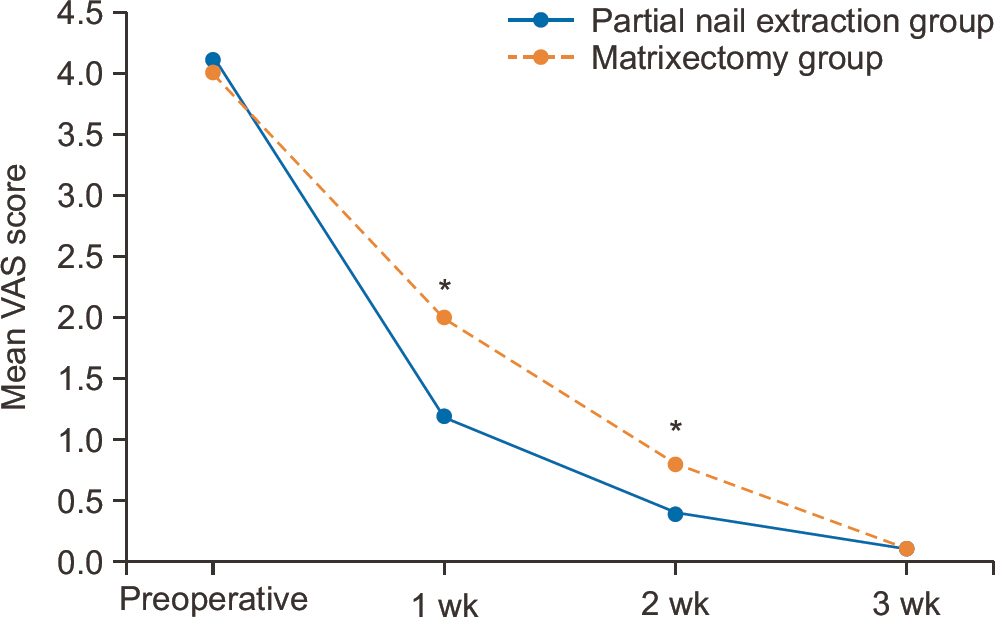
The medical records of patients who had surgical treatment for an ingrown nail in the authors' institution between April 2016 and December 2017 were reviewed retrospectively. Under the inclusion and exclusion criteria, 28 patients with a simple partial nail extraction (group A) and 29 patients with a partial nail extraction with matrixectomy (group B) were investigated. As the clinical outcome, the visual analogue scale (VAS) and satisfaction score, time to return to duty, complications, and recurrence rate were checked and compared between the groups.
RESULTS
The VAS scores of group B were significantly higher during the first (p<0.001) and second (p=0.026) follow-up week than group A. The time to return to duty was shorter in group A (7.8 days) than group B (10.1 days), and this difference was significant (p<0.001). Group B had five patients with complications, whereas group A had none (p=0.028). No differences in the recurrence rate (p=0.197) and patient satisfaction (p=0.764) were found between the groups.
CONCLUSION
In this study, simple partial nail extraction in military trainees resulted in lower postoperative pain, lower complication rates, and earlier return to duty than the procedure with matrixectomy. Military trainees are temporarily exposed to highly demanding activities. Thus, a satisfactory outcome would be expected with simple partial nail extraction without performing a radical procedure, such as a matrixectomy.
MeSH Terms
Figure
Reference
-
1.DeLauro TM. Onychocryptosis. Clin Podiatr Med Surg. 1995. 12:201–13.
Article2.Heidelbaugh JJ., Lee H. Management of the ingrown toenail. Am Fam Physician. 2009. 79:303–8.3.Parrinello JF., Japour CJ., Dykyj D. Incurvated nail. Does the phalanx determine nail plate shape? J Am Podiatr Med Assoc. 1995. 85:696–8. DOI: doi: 10.7547/87507315-85-11-696.4.Günal I., Koşay C., Veziroğlu A., Balkan Y., Ilhan F. Relationship between onychocryptosis and foot type and treatment with toe spacer. A preliminary investigation. J Am Podiatr Med Assoc. 2003. 93:33–6. 4725.2007.34012.x.5.Eekhof JA., Van Wijk B., Knuistingh Neven A., van der Wouden JC. Interventions for ingrowing toenails. Cochrane Database Syst Rev. 2012. 4:CD001541. DOI: doi: 10.1002/14651858.CD001541. pub3.
Article6.Persichetti P., Simone P., Li Vecchi G., Di Lella F., Cagli B., Marangi GF. Wedge excision of the nail fold in the treatment of ingrown toenail. Ann Plast Surg. 2004. 52:617–20. DOI: doi: 10.1097/01. sap.0000095436.08812.67.
Article7.Haneke E. Controversies in the treatment of ingrown nails. Dermatol Res Pract. 2012. 2012:783924. DOI: doi: 10.1155/2012/783924.
Article8.Khunger N., Kandhari R. Ingrown toenails. Indian J Dermatol Ve-nereol Leprol. 2012. 78:279–89. DOI: doi: 10.4103/0378-6323.95442.
Article9.Haricharan RN., Masquijo J., Bettolli M. Nail-fold excision for the treatment of ingrown toenail in children. J Pediatr. 2013. 162:398–402. DOI: doi: 10.1016/j.jpeds.2012.07.056.
Article10.Mousavi SR., Khoshnevice J. A new surgical technique for ingrown toenail. ISRN Surg. 2012. 2012:438915. DOI: doi: 10.5402/2012/438915. 72.DOI: doi: 10.7547/87507315-76-8-469.
Article11.Shih YH., Huang CY., Lee CC., Lee WR. Nail brace application: a noninvasive treatment for ingrown nails in pediatric patients. Dermatol Surg. 2019. 45:323–6. DOI: doi: 10.1097/DSS.0000000000001530.
Article12.Zaraa I., Dorbani I., Hawilo A., Mokni M., Ben Osman A. Segmental phenolization for the treatment of ingrown toenails: technique report, follow up of 146 patients, and review of the literature. Dermatol Online J. 2013. 19:18560.
Article13.Aksakal AB., Oztas P., Atahan C., Gurer MA. Decompression for the management of onychocryptosis. J Dermatolog Treat. 2004. 15:108–11. DOI: doi: 10.1080/09546630310016817.
Article14.Noël B. Surgical treatment of ingrown toenail without matri-cectomy. Dermatol Surg. 2008. 34:79–83. DOI: doi: 10.1111/j.1524.15.Heifetz CJ. Ingrown toe-nail: a clinical study. Am J Surg. 1937. 38:298–315. DOI: doi: 10.1016/S0002-9610(37)90439-2.16.Kaufman KR., Brodine S., Shaffer R. Military training-related injuries: surveillance, research, and prevention. Am J Prev Med. 2000. 18(3 Suppl):54–63. DOI: doi: 10.1016/S0749-3797(00)00114-8.
Article17.Şenel E., Doğruer Şenel S., Salmanoğlu M. Prevalence of skin diseases in civilian and military population in a Turkish military hospital in the central Black Sea region. J R Army Med Corps. 2015. 161:112–5. DOI: doi: 10.1136/jramc-2014-000267.
Article18.Guler O., Tuna H., Mahirogullari M., Erdil M., Mutlu S., Isyar M. Nail braces as an alternative treatment for ingrown toenails: results from a comparison with the Winograd technique. J Foot Ankle Surg. 2015. 54:620–4. DOI: doi: 10.1053/j.jfas.2015.04.013.
Article19.Gilles GA., Dennis KJ., Harkless LB. Periostitis associated with phenol matricectomies. J Am Podiatr Med Assoc. 1986. 76:469-.
Article20.Isik C., Cakici H., Cagri Kose K., Goksugur N. Comparison of partial matrixectomy and combination treatment (partial ma-trixectomy + phenol) in ingrown toenail. Med Glas (Zenica). 2013. 10:81–5.21.Grieg JD., Anderson JH., Ireland AJ., Anderson JR. The surgical treatment of ingrowing toenails. J Bone Joint Surg Br. 1991. 73:131–3.
Article22.Palmer BV., Jones A. Ingrowing toenails: the results of treatment. Br J Surg. 1979. 66:575–6. DOI: doi: 10.1002/bjs.1800660818.
Article23.Kim M., Song IG., Kim HJ. Partial removal of nail matrix in the treatment of ingrown nails: prospective randomized control study between curettage and electrocauterization. Int J Low Ex-trem Wounds. 2015. 14:192–5. DOI: doi: 10.1177/1534734614550685.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Success Rates of Multiple Treatments for Ingrown Nails
- The Effectiveness of Surgical Correction of Pincer Nails Using Nail Bed Flap and Bilateral Partial Matrixectomy, with or without Osteophyte Removal
- A Study of Nail-splinting Technique with Flexible Plastic Tube in Ingrown Nail
- Effectiveness of matricectomy with carbon dioxide laser ablation for ingrown toenail in Republic of Korea: a retrospective study
- Treatment of Ingrowing Toenails: Comparision of Surgery and Conservative Method Using Memory Alloy