Diabetes Metab J.
2018 Dec;42(6):513-518. 10.4093/dmj.2018.0006.
Association between Serum Cystatin C and Vascular Complications in Type 2 Diabetes Mellitus without Nephropathy
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Soonchunhyang University Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. hkpark@schmc.ac.kr
- KMID: 2449628
- DOI: http://doi.org/10.4093/dmj.2018.0006
Abstract
- BACKGROUND
Recent studies have correlated serum cystatin C (CysC) with vascular complications, but few studies have investigated this correlation in diabetes patients without nephropathy. This study aimed to evaluate if higher serum CysC levels increase the risk for vascular complications in type 2 diabetes mellitus patients with normal renal function or mild renal impairment.
METHODS
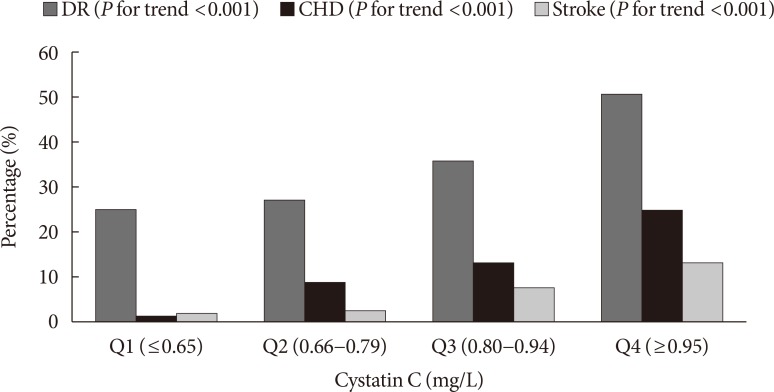
A total of 806 consecutive patients with type 2 diabetes mellitus who were admitted to the diabetes center of Soonchunhyang University Hospital for blood glucose control were retrospectively reviewed. Patients with nephropathy were excluded. Subjects were categorized into quartiles of serum CysC levels (Q1, ≤0.65 mg/L; Q2, 0.66 to 0.79 mg/L; Q3, 0.80 to 0.94 mg/L; and Q4, ≥0.95 mg/L).
RESULTS
The proportion of patients with diabetic retinopathy (DR) (P for trend < 0.001), coronary heart disease (CHD) (P for trend < 0.001), and stroke (P for trend < 0.001) increased across the serum CysC quartiles. After adjustment for confounding factors, the highest serum CysC level remained a significant risk factor for DR (odds ratio [OR], 1.929; 95% confidence interval [CI], 1.007 to 4.144; P=0.040). Compared with Q1, a significant positive association was observed between serum CysC and CHD in Q2 (OR, 7.321; 95% CI, 1.114 to 48.114; P=0.012), Q3 (OR, 6.027; 95% CI, 0.952 to 38.161; P=0.020), and Q4 (OR, 8.122; 95% CI, 1.258 to 52.453; P=0.007). No associations were observed between CysC and stroke after additional adjustment for confounding variables.
CONCLUSION
Serum CysC levels are independently associated with DR and CHD, suggesting that CysC may be useful for identifying type 2 diabetes mellitus patients without nephropathy who are at high risk for vascular complications.
MeSH Terms
Figure
Reference
-
1. World Health Organization: 10 Facts on diabetes. updated 2016 Apr. Available from: http://www.who.int/features/factfiles/diabetes/en/.2. Mussap M, Plebani M. Biochemistry and clinical role of human cystatin C. Crit Rev Clin Lab Sci. 2004; 41:467–550. PMID: 15603510.
Article3. Pucci L, Triscornia S, Lucchesi D, Fotino C, Pellegrini G, Pardini E, Miccoli R, Del Prato S, Penno G. Cystatin C and estimates of renal function: searching for a better measure of kidney function in diabetic patients. Clin Chem. 2007; 53:480–488. PMID: 17259236.
Article4. Liu J, Sukhova GK, Sun JS, Xu WH, Libby P, Shi GP. Lysosomal cysteine proteases in atherosclerosis. Arterioscler Thromb Vasc Biol. 2004; 24:1359–1366. PMID: 15178558.
Article5. Domingueti CP, Fuzatto JA, Foscolo RB, Reis JS, Dusse LM, Carvalho MDG, Gomes KB, Fernandes AP. Association between Von Willebrand factor, disintegrin and metalloproteinase with thrombospondin type 1 motif member 13, d-Dimer and cystatin C levels with retinopathy in type 1 diabetes mellitus. Clin Chim Acta. 2016; 459:1–4. PMID: 27208743.6. He R, Shen J, Zhao J, Zeng H, Li L, Zhao J, Liu F, Jia W. High cystatin C levels predict severe retinopathy in type 2 diabetes patients. Eur J Epidemiol. 2013; 28:775–778. PMID: 23918210.
Article7. Wong CW, Teo BW, Lamoureux E, Ikram MK, Wang JJ, Tai ES, Sethi S, Wong TY, Sabanayagam C. Serum cystatin C, markers of chronic kidney disease, and retinopathy in persons with diabetes. J Diabetes Res. 2015; 2015:404280. PMID: 26576434.
Article8. Koenig W, Twardella D, Brenner H, Rothenbacher D. Plasma concentrations of cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: more than simply a marker of glomerular filtration rate. Clin Chem. 2005; 51:321–327. PMID: 15563478.
Article9. Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007; 115:173–179. PMID: 17190862.10. Triki S, Fekih O, Hellara I, Neffati F, Douki W, Hamda KB, Maatouk F, Najjar MF. Association between serum cystatin C levels and cardiovascular disease in type 2 diabetic patients. Ann Biol Clin (Paris). 2013; 71:438–442. PMID: 23906571.
Article11. Xu Z, Leng C, Yang B, Wang H, Sun J, Liu Z, Yang L, Ge W, Zhu J. Serum cystatin C is associated with large cerebral artery stenosis in acute ischemic stroke. Oncotarget. 2017; 8:67181–67188. PMID: 28978025.
Article12. Aiello LP, Gardner TW, King GL, Blankenship G, Cavallerano JD, Ferris FL 3rd, Klein R. Diabetic retinopathy. Diabetes Care. 1998; 21:143–156. PMID: 9538986.
Article13. Paraoan L, Hiscott P, Gosden C, Grierson I. Cystatin C in macular and neuronal degenerations: implications for mechanism(s) of age-related macular degeneration. Vision Res. 2010; 50:737–742. PMID: 19917302.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients
- Usefulness of Serum Cystatin C for the Evaluation of Renal Function in Diabetic Patient
- Spot Urine Albumin to Creatinine Ratio and Serum Cystatin C are Effective for Detection of Diabetic Nephropathy in Childhood Diabetic Patients
- Plasma Paraoxonase Activities in Type 2 Diabetes Mellitus
- Serum Cystatin C Reflects the Progress of Albuminuria