Ann Rehabil Med.
2018 Dec;42(6):833-837. 10.5535/arm.2018.42.6.833.
Improvement of Peak Cough Flow After the Application of a Mechanical In-exsufflator in Patients With Neuromuscular Disease and Pneumonia: A Pilot Study
- Affiliations
-
- 1Department of Rehabilitation Medicine and Rehabilitation Institute of Neuromuscular Disease, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. kswoong@yuhs.ac
- 2Department of Physical Medicine and Rehabilitation, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 3Pulmonary Rehabilitation Center, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2448904
- DOI: http://doi.org/10.5535/arm.2018.42.6.833
Abstract
OBJECTIVE
To investigate and demonstrate persistent increase of peak cough flow after mechanical in-exsufflator application, in patients with neuromuscular diseases and pneumonia.
METHODS
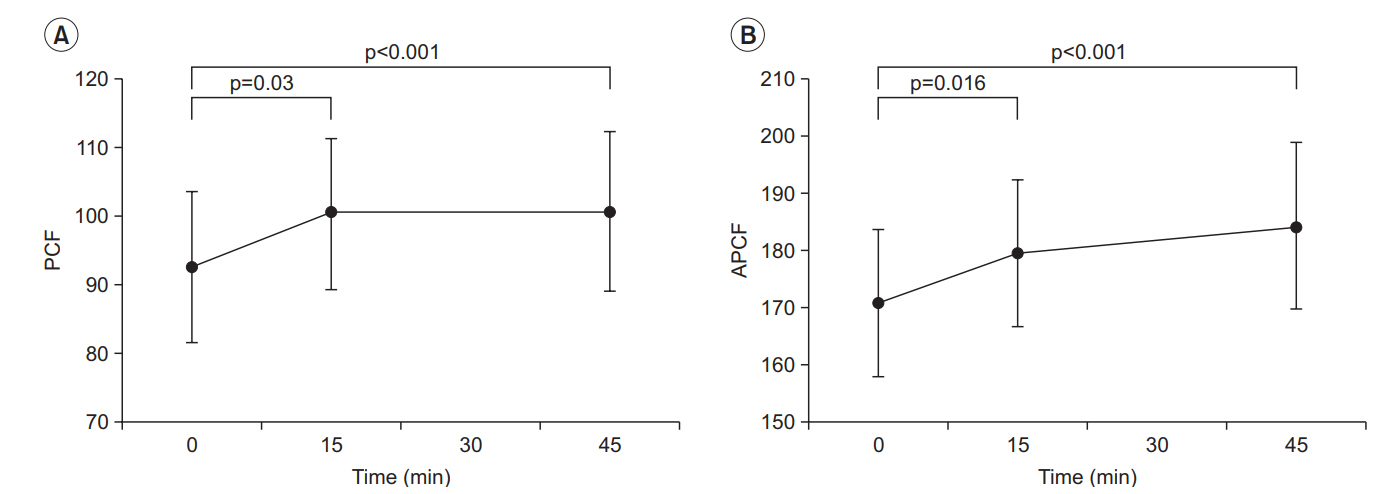
A mechanical in-exsufflator was applied with patients in an upright or semi-upright sitting position (pressure setting, +40 and −40 cmH2O; in-exsufflation times, 2-3 and 1-2 seconds, respectively). Patients underwent five cycles, with 20-30 second intervals to prevent hyperventilation. Peak cough flow without and with assistive maneuvers, was evaluated before, and 15 and 45 minutes after mechanical in-exsufflator application.
RESULTS
Peak cough flow was 92.6 L/min at baseline, and 100.4 and 100.7 L/min at 15 and 45 minutes after mechanical in-exsufflator application, respectively. Assisted peak cough flow at baseline, 15 minutes, and 45 minutes after mechanical in-exsufflator application was 170.7, 179.3, and 184.1 L/min, respectively. While peak cough flow and assisted peak cough flow increased significantly at 15 minutes after mechanical in-exsufflator application compared with baseline (p=0.030 and p=0.016), no statistical difference was observed between 15 and 45 minutes.
CONCLUSION
Increased peak cough flow after mechanical in-exsufflator application persists for at least 45 minutes.
Figure
Reference
-
1. Bach JR, Ishikawa Y, Kim H. Prevention of pulmonary morbidity for patients with Duchenne muscular dystrophy. Chest. 1997; 112:1024–8.
Article2. Lechtzin N, Wiener CM, Clawson L, Chaudhry V, Diette GB. Hospitalization in amyotrophic lateral sclerosis: causes, costs, and outcomes. Neurology. 2001; 56:753–7.
Article3. Andersen PM, Borasio GD, Dengler R, Hardiman O, Kollewe K, Leigh PN, et al. EFNS task force on management of amyotrophic lateral sclerosis: guidelines for diagnosing and clinical care of patients and relatives. Eur J Neurol. 2005; 12:921–38.4. Bach JR. Amyotrophic lateral sclerosis: prolongation of life by noninvasive respiratory AIDS. Chest. 2002; 122:92–8.5. Inkley SR, Oldenburg FC, Vignos PJ Jr. Pulmonary function in Duchenne muscular dystrophy related to stage of disease. Am J Med. 1974; 56:297–306.
Article6. Rideau Y, Gatin G, Bach J, Gines G. Prolongation of life in Duchenne’s muscular dystrophy. Acta Neurol (Napoli). 1983; 5:118–24.7. Vignos PJ Jr. Respiratory function and pulmonary infection in Duchenne muscular dystrophy. Isr J Med Sci. 1977; 13:207–14.
Article8. Bach JR. Amyotrophic lateral sclerosis: predictors for prolongation of life by noninvasive respiratory aids. Arch Phys Med Rehabil. 1995; 76:828–32.
Article9. Bach JR. Mechanical insufflation-exsufflation. Comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest. 1993; 104:1553–62.10. Chatwin M, Ross E, Hart N, Nickol AH, Polkey MI, Simonds AK. Cough augmentation with mechanical insufflation/exsufflation in patients with neuromuscular weakness. Eur Respir J. 2003; 21:502–8.
Article11. Sancho J, Servera E, Díaz J, Marin J. Efficacy of mechanical insufflation-exsufflation in medically stable patients with amyotrophic lateral sclerosis. Chest. 2004; 125:1400–5.
Article12. Winck JC, Goncalves MR, Lourenco C, Viana P, Almeida J, Bach JR. Effects of mechanical insufflationexsufflation on respiratory parameters for patients with chronic airway secretion encumbrance. Chest. 2004; 126:774–80.
Article13. Fauroux B, Guillemot N, Aubertin G, Nathan N, Labit A, Clement A, et al. Physiologic benefits of mechanical insufflation-exsufflation in children with neuromuscular diseases. Chest. 2008; 133:161–8.
Article14. Bach JR. Update and perspective on noninvasive respiratory muscle aids. Part 2. The expiratory aids. Chest. 1994; 105:1538–44.15. Sinha R, Bergofsky EH. Prolonged alteration of lung mechanics in kyphoscoliosis by positive pressure hyperinflation. Am Rev Respir Dis. 1972; 106:47–57.16. Lechtzin N, Shade D, Clawson L, Wiener CM. Supramaximal inflation improves lung compliance in subjects with amyotrophic lateral sclerosis. Chest. 2006; 129:1322–9.
Article17. Chatwin M. How to use a mechanical insufflator–exsufflator “cough assist machine”. Breathe. 2008; 4:320–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of Pulmonary Rehabilitation Using Mechanical In-Exsufflator in Cervical Cord Injured Patients
- A Comparison of Cough Assistance Techniques in Patients with Respiratory Muscle Weakness
- Clinical Implication of Air Stacking Exercise in Patients with Neuromuscular Diseases
- Non-invasive Intermittent Positive Pressure Ventilation Apply to Complete Tetraplegia due to C1 Spinal Cord Injury: A case report
- Neuromuscular Electrical Stimulation for Dysphagia