Ann Rehabil Med.
2018 Dec;42(6):814-821. 10.5535/arm.2018.42.6.814.
Needle Entry Angle to Prevent Carotid Sheath Injury for Fluoroscopy-Guided Cervical Transforaminal Epidural Steroid Injection
- Affiliations
-
- 1Department of Rehabilitation Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. minkhrm@gmail.com
- 2Department of Radiology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- KMID: 2448902
- DOI: http://doi.org/10.5535/arm.2018.42.6.814
Abstract
OBJECTIVE
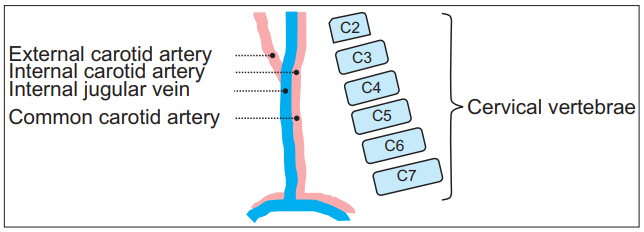
To suggest rotation angles of fluoroscopy that can bypass the carotid sheath according to vertebral levels for cervical transforaminal epidural steroid injection (TFESI).
METHODS
Patients who underwent cervical spine magnetic resonance imaging (MRI) from January 2009 to October 2017 were analyzed. In axial sections of cervical spine MRI, three angles to the vertical line (α, angle not to insult carotid sheath; β, angle for the conventional TFESI; γ, angle not to penetrate carotid artery) were measured.
RESULTS
Alpha (α) angles tended to increase for upper cervical levels (53.3° in C6-7, 65.2° in C5-6, 75.3° in C4-5, 82.3° in C3-4). Beta (β) angles for conventional TFESI showed a constant value of 45° to 47° (47.5° in C6-7, 47.4° in C5-6, 45.7° in C4-5, 45.0° in C3-4). Gamma (γ) angles increased at higher cervical levels as did α angles (25.2° in C6-7, 33.6° in C5-6, 43.0° in C4-5, 56.2° in C3-4).
CONCLUSION
The risk of causing injury by penetrating major vessels in the carotid sheath tends to increase at upper cervical levels. Therefore, prior to cervical TFESI, measuring the angle is necessary to avoid carotid vessels in the axial section of CT or MRI, thus contributing to a safer procedure.
Keyword
MeSH Terms
Figure
Reference
-
1. Van Zundert J, Huntoon M, Patijn J, Lataster A, Mekhail N, van Kleef M, et al. 4. Cervical radicular pain. Pain Pract. 2010; 10:1–17.
Article2. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004; 100:1595–600.
Article3. Kang JD, Stefanovic-Racic M, McIntyre LA, Georgescu HI, Evans CH. Toward a biochemical understanding of human intervertebral disc degeneration and herniation. Contributions of nitric oxide, interleukins, prostaglandin E2, and matrix metalloproteinases. Spine (Phila Pa 1976). 1997; 22:1065–73.4. House LM, Barrette K, Mattie R, McCormick ZL. Cervical Epidural steroid injection: techniques and evidence. Phys Med Rehabil Clin N Am. 2018; 29:1–17.5. Diwan S, Manchikanti L, Benyamin RM, Bryce DA, Geffert S, Hameed H, et al. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician. 2012; 15:E405–34.6. Engel A, King W, MacVicar J; Standards Division of the International Spine Intervention Society. The effectiveness and risks of fluoroscopically guided cervical transforaminal injections of steroids: a systematic review with comprehensive analysis of the published data. Pain Med. 2014; 15:386–402.
Article7. El-Yahchouchi CA, Plastaras CT, Maus TP, Carr CM, McCormick ZL, Geske JR, et al. Adverse event rates associated with transforaminal and interlaminar epidural steroid injections: a multi-institutional study. Pain Med. 2016; 17:239–49.
Article8. Huston CW. Cervical epidural steroid injections in the management of cervical radiculitis: interlaminar versus transforaminal: a review. Curr Rev Musculoskelet Med. 2009; 2:30–42.
Article9. Manchikanti L, Falco FJ, Benyamin RM, Gharibo CG, Candido KD, Hirsch JA. Epidural steroid injections safety recommendations by the Multi-Society Pain Workgroup (MPW): more regulations without evidence or clarification. Pain Physician. 2014; 17:E575–88.10. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidencebased review. Reg Anesth Pain Med. 2013; 38:175–200.11. Stojanovic MP, Vu TN, Caneris O, Slezak J, Cohen SP, Sang CN. The role of fluoroscopy in cervical epidural steroid injections: an analysis of contrast dispersal patterns. Spine (Phila Pa 1976). 2002; 27:509–14.12. Lee JH, Lee SH. Comparison of clinical efficacy between interlaminar and transforaminal epidural injection in patients with axial pain due to cervical disc herniation. Medicine (Baltimore). 2016; 95:e2568.
Article13. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine (Phila Pa 1976). 2007; 32:1249–56.14. Schneider BJ, Maybin S, Sturos E. Safety and complications of cervical epidural steroid injections. Phys Med Rehabil Clin N Am. 2018; 29:155–69.
Article15. Strub WM, Brown TA, Ying J, Hoffmann M, Ernst RJ, Bulas RV. Translaminar cervical epidural steroid injection: short-term results and factors influencing outcome. J Vasc Interv Radiol. 2007; 18:1151–5.
Article16. Furman MB, Berkwits L, Cohen I, Goodman B, Kirschner J, Lee TS, et al. Atlas of image-guided spinal procedures. 2nd ed. Philadelphia: Elsevier;2018. p. 243–9.17. Chen B, Rispoli L, Stitik TP, Foye PM, Georgy JS. Optimal needle entry angle for cervical transforaminal epidural injections. Pain Physician. 2014; 17:139–44.18. Dawley JD, Moeller-Bertram T, Wallace MS, Patel PM. Intra-arterial injection in the rat brain: evaluation of steroids used for transforaminal epidurals. Spine (Phila Pa 1976). 2009; 34:1638–43.19. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001; 344:898–906.
Article20. Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995; 45:1517–22.
Article21. Biousse V, D’Anglejan-Chatillon J, Massiou H, Bousser MG. Head pain in non-traumatic carotid artery dissection: a series of 65 patients. Cephalalgia. 1994; 14:33–6.
Article22. Biousse V, D’Anglejan-Chatillon J, Touboul PJ, Amarenco P, Bousser MG. Time course of symptoms in extracranial carotid artery dissections: a series of 80 patients. Stroke. 1995; 26:235–9.23. Stewart HD, Quinnell RC, Dann N. Epidurography in the management of sciatica. Br J Rheumatol. 1987; 26:424–9.
Article24. Fitzgerald RT, Bartynski WS, Collins HR. Vertebral artery position in the setting of cervical degenerative disease: implications for selective cervical transforaminal epidural injections. Interv Neuroradiol. 2013; 19:425–31.
Article25. Kim HJ, Nemani VM, Piyaskulkaew C, Vargas SR, Riew KD. Cervical radiculopathy: incidence and treatment of 1,420 consecutive cases. Asian Spine J. 2016; 10:231–7.
Article26. Wilbourn AJ, Aminoff MJ. AAEM minimonograph 32: the electrodiagnostic examination in patients with radiculopathies. American Association of Electrodiagnostic Medicine. Muscle Nerve. 1998; 21:1612–31.27. Carette S, Fehlings MG. Clinical practice: cervical radiculopathy. N Engl J Med. 2005; 353:392–9.28. Karm MH, Park JY, Kim DH, Cho HS, Lee JY, Kwon K, et al. New optimal needle entry angle for cervical transforaminal epidural steroid injections: a retrospective study. Int J Med Sci. 2017; 14:376–81.
Article29. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–74.
Article30. Batzdorf U, Batzdorff A. Analysis of cervical spine curvature in patients with cervical spondylosis. Neurosurgery. 1988; 22:827–36.
Article31. Lo A, Oehley M, Bartlett A, Adams D, Blyth P, Al-Ali S. Anatomical variations of the common carotid artery bifurcation. ANZ J Surg. 2006; 76:970–2.
Article32. Shoja MM, Ardalan MR, Tubbs RS, Loukas M, Vahedinia S, Jabbary R, et al. The relationship between the internal jugular vein and common carotid artery in the carotid sheath: the effects of age, gender and side. Ann Anat. 2008; 190:339–43.
Article33. Bouthillier A, van Loveren HR, Keller JT. Segments of the internal carotid artery: a new classification. Neurosurgery. 1996; 38:425–33.
Article34. Gordon AC, Saliken JC, Johns D, Owen R, Gray RR. US-guided puncture of the internal jugular vein: complications and anatomic considerations. J Vasc Interv Radiol. 1998; 9:333–8.
Article35. Nishio I. Cervical transforaminal epidural steroid injections: a proposal for optimizing the preprocedural evaluation with available imaging. Reg Anesth Pain Med. 2014; 39:546–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of incidence of intravascular injections during transforaminal epidural steroid injection using different needle types
- CT Guided Cervical Transforaminal Steroid Injection: 2 Months Follow-up
- Epidural hematoma treated by aspiration after transforaminal epidural steroid injection - A case report -
- Analysis of Influencing Factors to Depth of Epidural Space for Lumbar Transforaminal Epidural Block in Korean
- Oblique interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: A case report