Hip Pelvis.
2019 Jun;31(2):102-109. 10.5371/hp.2019.31.2.102.
Hip Arthroscopy of a Painful Hip with Borderline Dysplasia
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chonbuk National University Medical School, Jeonju, Korea.
- 2Department of Orthopaedic Surgery, School of Medicine, Chosun University, Gwangju, Korea. jo.suenghwan@chosun.ac.kr
- KMID: 2448029
- DOI: http://doi.org/10.5371/hp.2019.31.2.102
Abstract
- PURPOSE
Hip arthroscopy has been considered for treating hip dysplasia; however, its efficacy is still a matter of controversy. Here, we report outcomes of patients with borderline dysplasia treated with a contemporary hip arthroscopy technique.
MATERIALS AND METHODS
Forty-seven hips with borderline hip dysplasia were treated using hip arthroscopy. Patients underwent procedures to correct torn labrums or ligamentum teres with additional procedure on the acetabular capsule. Patient outcomes were assessed using visual analogue scale (VAS), modified Harris Hip Score (mHHS), Nonarthritic Hip Score (NAHS) and patient satisfaction. Risk factors for poor prognosis were also investigated.
RESULTS
The mean follow up period was 25.9 months. At the last follow up, mean VAS score decreased from 6.1±1.6 to 3.5±2.8 (P=0.016). The mHHS and NHAS at the last follow up improved from 61.0±7.6 to 78.6±19.5 (P=0.001) and 62.1±7.5 to 80.0±18.5 (P=0.002), respectively. While significant improvement was observed in all patient reported outcome measures tested, 19 (40.4%) hips indicated that "the operation was unsatisfactory." The only factor shown to influence outcomes was preoperative VAS (i.e., worse scores potentially an indicator of poor outcomes).
CONCLUSION
The results of the current study indicate that arthroscopic management may be beneficial for a subset of patients with borderline dysplasia; however, the dissatisfaction rate associated with this treatment approach may be as high as 40%. The poor preoperative pain score appears to be the sole indicator for poor outcomes.
Keyword
MeSH Terms
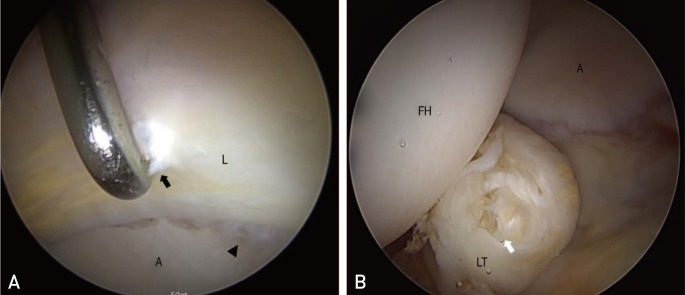
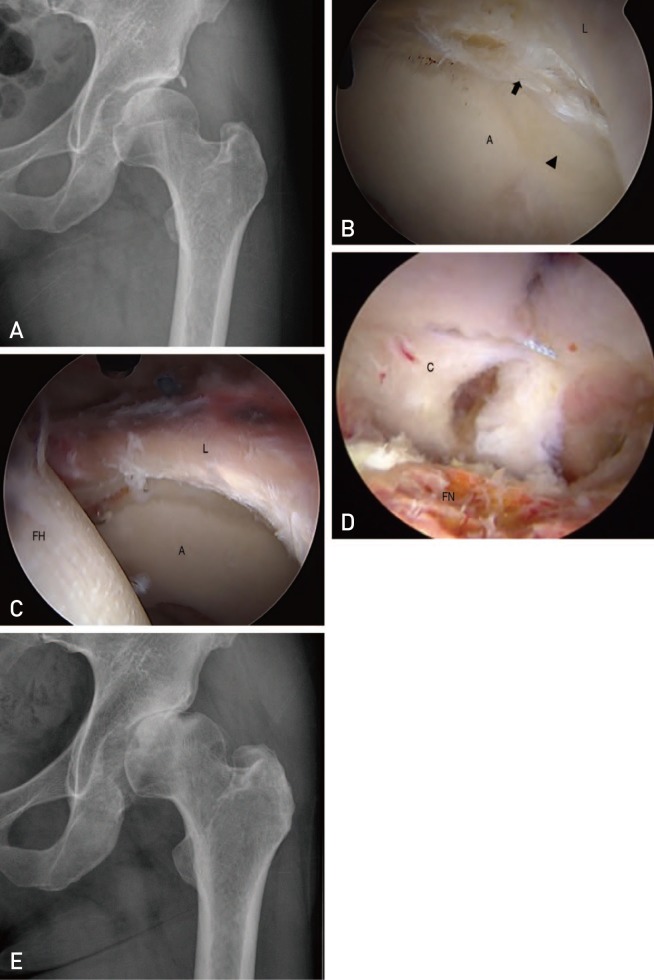
Figure
Cited by 1 articles
-
Hip Arthroscopy of a Painful Hip with Borderline Dysplasia: Letter to the Editor
Mingjin Zhong, Kan Ouyang
Hip Pelvis. 2019;31(3):174-175. doi: 10.5371/hp.2019.31.3.174.
Reference
-
1. Jo S, Lee SH, Wang SI, Smith B, O'Donnell J. The role of arthroscopy in the dysplastic hip-a systematic review of the intra-articular findings, and the outcomes utilizing hip arthroscopic surgery. J Hip Preserv Surg. 2016; 3:171–180. PMID: 27583155.
Article2. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016; 5:225–231. PMID: 27313136.3. Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995; 77:985–989. PMID: 7608241.
Article4. Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011; 93(Suppl 2):17–21. PMID: 21543683.
Article5. Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976; (119):39–47.6. Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003; 19:1055–1060. PMID: 14673446.
Article7. Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003; (406):75–83. PMID: 12579003.
Article8. Dawes P, Haslock I. Visual analogue scales. Ann Rheum Dis. 1982; 41:434–435. PMID: 7114926.
Article9. Henak CR, Abraham CL, Anderson AE, et al. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage. 2014; 22:210–217. PMID: 24269633.
Article10. Vafaeian B, Zonoobi D, Mabee M, et al. Finite element analysis of mechanical behavior of human dysplastic hip joints: a systematic review. Osteoarthritis Cartilage. 2017; 25:438–447. PMID: 27836678.
Article11. Henak CR, Ellis BJ, Harris MD, Anderson AE, Peters CL, Weiss JA. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011; 44:2201–2206. PMID: 21757198.
Article12. Lievense AM, Bierma-Zeinstra SM, Verhagen AP, Verhaar JA, Koes BW. Influence of hip dysplasia on the development of osteoarthritis of the hip. Ann Rheum Dis. 2004; 63:621–626. PMID: 15140766.13. Irie T, Takahashi D, Asano T, et al. Is there an association between borderline-to-mild dysplasia and hip osteoarthritis? Analysis of CT osteoabsorptiometry. Clin Orthop Relat Res. 2018; 476:1455–1465. PMID: 29698301.
Article14. Ding Z, Sun Y, Liu S, Chen J. Hip arthroscopic surgery in borderline developmental dysplastic hips: a systematic review. Am J Sports Med. Published online November 27, 2018. DOI: 10.1177/0363546518803367.
Article15. Edelson R, Burks RT, Bloebaum RD. Short-term effects of knee washout for osteoarthritis. Am J Sports Med. 1995; 23:345–349. PMID: 7661265.16. Lee YK, Ha YC, Hwang DS, Koo KH. Learning curve of basic hip arthroscopy technique: CUSUM analysis. Knee Surg Sports Traumatol Arthrosc. 2013; 21:1940–1944. PMID: 23073816.
Article17. Mehta N, Chamberlin P, Marx RG, et al. Defining the learning curve for hip arthroscopy: a threshold analysis of the volume-outcomes relationship. Am J Sports Med. 2018; 46:1284–1293. PMID: 29337602.
Article18. Schüttler KF, Schramm R, El-Zayat BF, Schofer MD, Efe T, Heyse TJ. The effect of surgeon's learning curve: complications and outcome after hip arthroscopy. Arch Orthop Trauma Surg. 2018; 138:1415–1421. PMID: 29802454.
Article19. Matosin N, Frank E, Engel M, Lum JS, Newell KA. Negativity towards negative results: a discussion of the disconnect between scientific worth and scientific culture. Dis Model Mech. 2014; 7:171–173. PMID: 24713271.
Article20. Fanelli D. Do pressures to publish increase scientists' bias? An empirical support from US States Data. PLoS One. 2010; 5:e10271. PMID: 20422014.
Article21. Kalore NV, Jiranek WA. Save the torn labrum in hips with borderline acetabular coverage. Clin Orthop Relat Res. 2012; 470:3406–3413. PMID: 22810161.
Article22. Parvizi J, Bican O, Bender B, et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009; 24(6 Suppl):110–113.
Article23. Chandrasekaran S, Darwish N, Martin TJ, Suarez-Ahedo C, Lodhia P, Domb BG. Arthroscopic capsular plication and labral seal restoration in borderline hip dysplasia: 2-year clinical outcomes in 55 cases. Arthroscopy. 2017; 33:1332–1340. PMID: 28408155.
Article24. Domb BG, Chaharbakhshi EO, Perets I, Yuen LC, Walsh JP, Ashberg L. Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med. 2018; 46:305–313. PMID: 29268026.
Article25. Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013; 41:2591–2598. PMID: 23956133.26. Jo S, Hooke AW, An KN, Trousdale RT, Sierra RJ. Contribution of the ligamentum teres to hip stability in the presence of an intact capsule: a cadaveric study. Arthroscopy. 2018; 34:1480–1487. PMID: 29397288.
Article27. Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy. 2015; 31:2371–2379. PMID: 26315056.
Article