Hip Pelvis.
2019 Jun;31(2):95-101. 10.5371/hp.2019.31.2.95.
Clinical Outcomes of U-blade Gamma3 Nails Used to Treat Patients with Trochanteric Fractures: Retrospective Multicenter Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Hallym University Sacred Heart Hospital, Hallym University School of Medicine, Anyang, Korea.
- 2Department of Orthopaedic Surgery, Korea University Guro Hospital, Seoul, Korea.
- 3Department of Orthopaedic Surgery, Hallym University Gangnam Sacred Heart Hospital, Hallym University School of Medicine, Seoul, Korea. hwangjihyo7309@gmail.com
- KMID: 2448028
- DOI: http://doi.org/10.5371/hp.2019.31.2.95
Abstract
- PURPOSE
This study was performed to assess the radiologic and clinical results of U-blade Gamma3 nail use for the treatment of trochanteric fractures.
MATERIALS AND METHODS
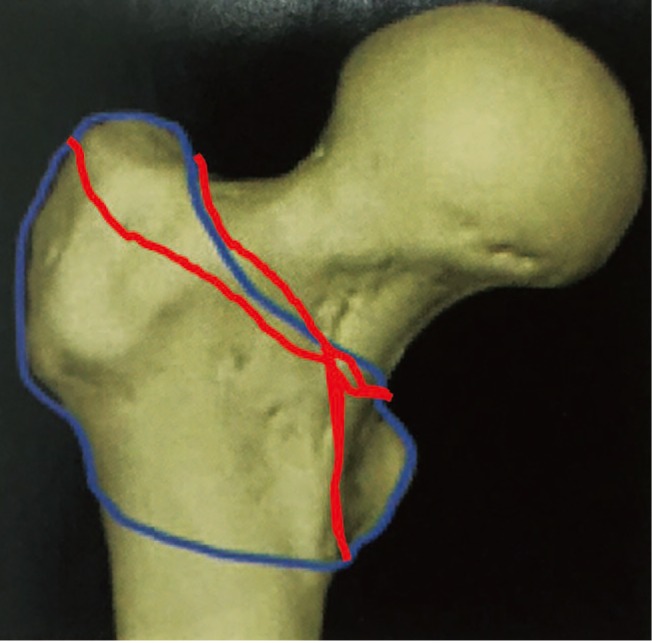
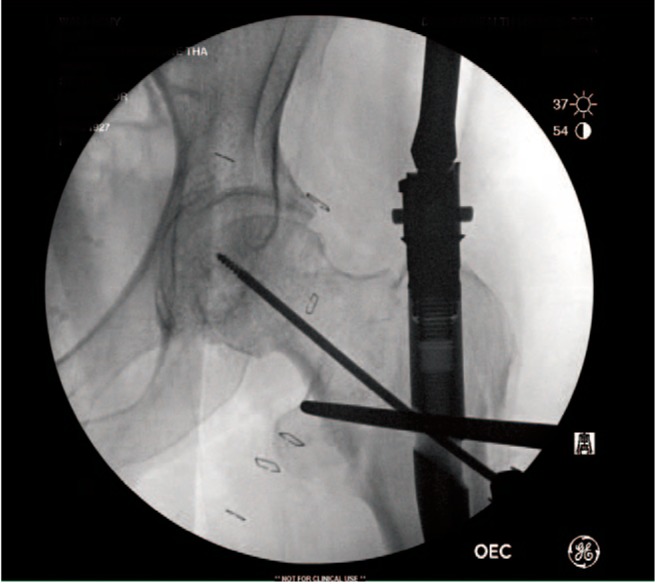
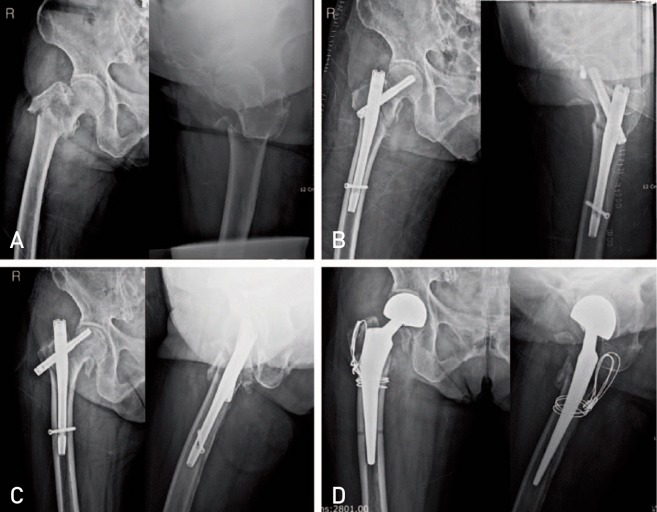
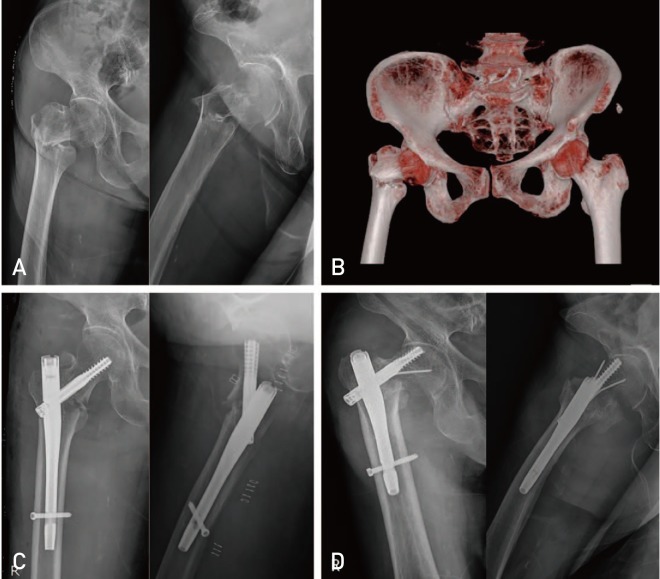
Between September 2015 and May 2018, all patients aged 65 years and older who underwent surgery with U-blade Gamma3 nails were analyzed. A total of 129 patients were selected based on having at least six months of follow-up. Image evaluations included bone quality (T-score), fracture classification on plain radiograph (AO/OTA), computed tomography configuration, union period, position of lag screw, anatomical reduction, tip apex distance (TAD), sliding extent of lag screw, change of neck shaft angle, and complications leading to reoperations were analyzed. Functional outcome were assessed using the Koval grade (ambulatory ability) at the final follow-up.
RESULTS
The mean time to union was 19.7 (range, 6-36) weeks. The screw position was centric (93 cases; 72.1%) and anatomical reduction was achieved in 74 cases (57.4%). The mean TAD was 20.3 (range, 12.3-38.1) mm. The mean sliding length of the lag screws was 3.8 (range, 0.1-12.6) mm. The mean change of neck shaft angle was 3.4° (range, 0-12.8°). Reoperations were required in two cases (1.6%) due to the cutting out of the lag screw (n=1) and metal failure with U-blade bending (n=1). Finally, Koval grades for 49.8% of patients reached preoperative status.
CONCLUSION
Overall, use of the U-blade Gamma3 nail led to favorable clinical results, suggesting that this system may be a good option for the treatment of trochanteric fractures.
Keyword
Figure
Cited by 1 articles
-
A Comparison of U-blade Gamma3 and Gamma3 Nails Used for the Treatment of Intertrochanteric Fractures
Hyung-Gon Ryu, Youn-Taek Choi, Sang-Min Kim, Jae-Sung Seo
Hip Pelvis. 2020;32(1):50-57. doi: 10.5371/hp.2020.32.1.50.
Reference
-
1. Stapert JW, Geesing CL, Jacobs PB, de Wit RJ, Vierhout PA. First experience and complications with the long Gamma nail. J Trauma. 1993; 34:394–400. PMID: 8483181.
Article2. Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008; 90:1862–1868. PMID: 18762645.
Article3. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; (310):150–159.4. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD. Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; (348):37–41. PMID: 9553531.5. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015; 135:811–818. PMID: 25840887.
Article6. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992; 74:340–344. PMID: 1587873.
Article7. Rosenblum SF, Zuckerman JD, Kummer FJ, Tam BS. A biomechanical evaluation of the Gamma nail. J Bone Joint Surg Br. 1992; 74:352–357. PMID: 1587875.
Article8. Williams WW, Parker BC. Complications associated with the use of the gamma nail. Injury. 1992; 23:291–292. PMID: 1644453.
Article9. Hesse B, Gachter A. Complications following the treatment of trochanteric fractures with the gamma nail. Arch Orthop Trauma Surg. 2004; 124:692–698. PMID: 15517321.
Article10. Kim SS, Lee KY, Kim CH, et al. Comparison of the Dyna locking trochanteric nail, proximal femoral nail antirotation and gamma 3 nail in treatment of intertrochanteric fracture of the femur. Hip Pelvis. 2013; 25:211–219.
Article11. Lang NW, Arthold C, Joestl J, et al. Does an additional antirotation U-Blade (RC) lag screw improve treatment of AO/OTA 31 A1-3 fractures with gamma 3 nail? Injury. 2016; 47:2733–2738. PMID: 27832831.
Article12. Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachie N. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury. 2009; 40:428–432. PMID: 19230885.
Article13. Chinzei N, Hiranaka T, Niikura T, et al. Comparison of the sliding and femoral head rotation among three different femoral head fixation devices for trochanteric fractures. Clin Orthop Surg. 2015; 7:291–297. PMID: 26330949.
Article14. Chevalley F, Gamba D. Gamma nailing of pertrochanteric and subtrochanteric fractures: clinical results of a series of 63 consecutive cases. J Orthop Trauma. 1997; 11:412–415. PMID: 9314147.
Article15. Goldhagen PR, O'Connor DR, Schwarze D, Schwartz E. A prospective comparative study of the compression hip screw and the gamma nail. J Orthop Trauma. 1994; 8:367–372. PMID: 7996318.
Article16. Friedl W, Colombo-Benkmann M, Dockter S, Machens HG, Mieck U. [Gamma nail osteosynthesis of per- and subtrochanteric femoral fractures. 4 years experiences and their consequences for further implant development]. Chirurg. 1994; 65:953–963. German. PMID: 7821076.17. Forthomme JP, Costenoble V, Soete P, Docquier J. [Treatment of trochanteric fractures of the femur using the gamma nail (apropos of a series of 92 cases)]. Acta Orthop Belg. 1993; 59:22–29. French. PMID: 8484318.18. Robinson CM, Adams CI, Craig M, Doward W, Clarke MC, Auld J. Implant-related fractures of the femur following hip fracture surgery. J Bone Joint Surg Am. 2002; 84:1116–1122. PMID: 12107309.
Article19. Wang CJ, Brown CJ, Yettram AL, Procter P. Intramedullary femoral nails: one or two lag screws? A preliminary study. Med Eng Phys. 2000; 22:613–624. PMID: 11259930.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of U-blade Gamma3 and Gamma3 Nails Used for the Treatment of Intertrochanteric Fractures
- Comparison of the U-Blade Gamma3 Nail and the Zimmer Natural Nail for the Treatment of Intertrochanteric Fracture
- Unstable Trochanteric Fractures of the Femur Treated with a Condylar Blade Plate
- Subtrochanteric Femoral Fracture during Trochanteric Nailing for the Treatment of Femoral Shaft Fracture
- Trochanteric Fixation Nail® with Helical Blade Compared with Femoral Neck Screw for Operative Treatment of Intertrochanteric Femoral Fractures