Anesth Pain Med.
2019 Apr;14(2):230-235. 10.17085/apm.2019.14.2.230.
Analysis of the characteristics of unplanned admission to the intensive care unit after general surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. s2248@paik.ac.kr
- KMID: 2447975
- DOI: http://doi.org/10.17085/apm.2019.14.2.230
Abstract
- BACKGROUND
Unplanned intensive care unit admission (UIA) is associated with perioperative morbidity and mortality, and can be used as a surrogate marker for patient safety. This study aimed to compare the characteristics of planned and unplanned intensive care unit (ICU) admission groups.
METHODS
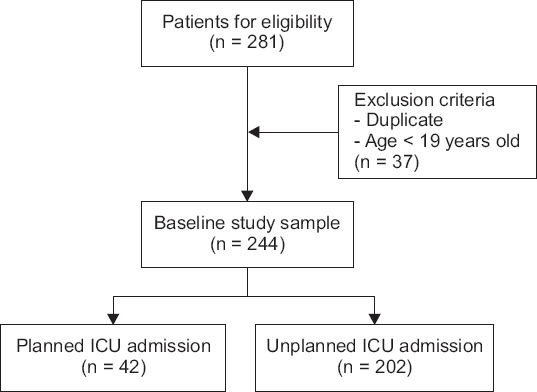
We retrospectively reviewed the electronic medical records of adult patients admitted to the ICU after abdominal and thyroid surgery under general anesthesia between 2016 and 2017. Preoperative, intraoperative, and postoperative information of enrolled patients was recorded. We compared patients' characteristics and outcomes between the unplanned and planned admission groups.
RESULTS
In the total cohort, the proportion of UIA was 82.8% (202/244). In the unplanned admission group, total hospital stay was significantly shorter and ICU stay longer than that in the planned admission group (19.0 and 3.0 days, respectively vs. 28.5 and 2.0 days, respectively). In-hospital mortality rates were 21.3% and 7.1% in the unplanned and planned groups, respectively (P = 0.055). Patients in the UIA group showed higher Acute Physiology And Chronic Health Evaluation II scores, higher American Society of Anesthesiologist physical status class, and more co-morbidities than those in the planned group. There were significant differences in the incidence of UIA among surgery types.
CONCLUSIONS
The UIA group had a relatively high mortality rate and longer ICU stay. More critically ill patients tended to be admitted to the ICU without planning.
MeSH Terms
Figure
Reference
-
1. Goldman R. Development of a Veterans Administration occurrence screening program. QRB Qual Rev Bull. 1989; 15:315–9. DOI: 10.1016/S0097-5990(16)30309-8.2. Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991; 324:370–6. DOI: 10.1056/NEJM199102073240604. PMID: 1987460.3. Haller G, Myles PS, Wolfe R, Weeks AM, Stoelwinder J, McNeil J. Validity of unplanned admission to an intensive care unit as a measure of patient safety in surgical patients. Anesthesiology. 2005; 103:1121–9. DOI: 10.1097/00000542-200512000-00004. PMID: 16306722.4. Quinn TD, Gabriel RA, Dutton RP, Urman RD. Analysis of unplanned postoperative admissions to the intensive care unit. J Intensive Care Med. 2017; 32:436–43. DOI: 10.1177/0885066615622124. PMID: 26721638.5. Frost SA, Alexandrou E, Bogdanovski T, Salamonson Y, Parr MJ, Hillman KM. Unplanned admission to intensive care after emergency hospitalisation: risk factors and development of a nomogram for individualising risk. Resuscitation. 2009; 80:224–30. DOI: 10.1016/j.resuscitation.2008.10.030. PMID: 19084319.6. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29. DOI: 10.1097/00003246-198510000-00009. PMID: 3928249.7. R Core Team. R: a language and environment for statistical computing. R Core Team [serial on the Internet]. [2017 Mar 6]. Available from https://www.R-project.org/ .8. Goldhill DR, Sumner A. Outcome of intensive care patients in a group of British intensive care units. Crit Care Med. 1998; 26:1337–45. DOI: 10.1097/00003246-199808000-00017.9. Hillman K. Critical care without walls. Curr Opin Crit Care. 2002; 8:594–9. DOI: 10.1097/00075198-200212000-00019. PMID: 12454548.10. Ugochukwu O, Jerome A. An audit of intensive care unit admission in a pediatric cardio-thoracic population in Enugu, Nigeria. Pan Afr Med J. 2010; 6:10. DOI: 10.4314/pamj.v6i1.69077.11. Cullen DJ, Nemeskal AR, Cooper JB, Zaslavsky A, Dwyer MJ. Effect of pulse oximetry, age, and ASA physical status on the frequency of patients admitted unexpectedly to a postoperative intensive care unit and the severity of their anesthesia-related complications. Anesth Analg. 1992; 74:181–8. DOI: 10.1213/00000539-199202000-00002. PMID: 1731535.12. Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012; 380:1059–65. DOI: 10.1016/S0140-6736(12)61148-9. PMID: 22998715. PMCID: PMC3493988.13. Swann D, Houston P, Goldberg J. Audit of intensive care unit admissions from the operating room. Can J Anaesth. 1993; 40:137–41. DOI: 10.1007/BF03011311. PMID: 8443852.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case Control Study Identifying the Predictors of Unplanned Intensive Care Unit Readmission After Discharge
- Comparison of Related Characteristics between Unplanned and Planned Extubation of Patients in Medical Intensive Unit
- Incidence of Unplanned Extubation and Related Factors of Reintubation in the Neonatal Intensive Care Unit
- Predictors for Reintubation after Unplanned Endotracheal Extubation in Multidisciplinary Intensive Care Unit
- Risk Factors and Clinical Outcomes of Unplanned Reintubation after Planned Extubation in Adult Patients admitted to the Intensive Care Unit after Cardiac Surgery