Anesth Pain Med.
2019 Apr;14(2):152-157. 10.17085/apm.2019.14.2.152.
The effect of endotracheal 1% lidocaine administration to reduce emergence phenomenon after general anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dankook University College of Medicine, Cheonan, Korea. anegwleeoo@gmail.com
- KMID: 2447962
- DOI: http://doi.org/10.17085/apm.2019.14.2.152
Abstract
- BACKGROUND
Endotracheal intubation often causes sore throat and coughing. The aim of this study was to decrease the incidence and severity of cough, sore throat, and hemodynamic changes after extubation by endotracheal administration of 1% lidocaine.
METHODS
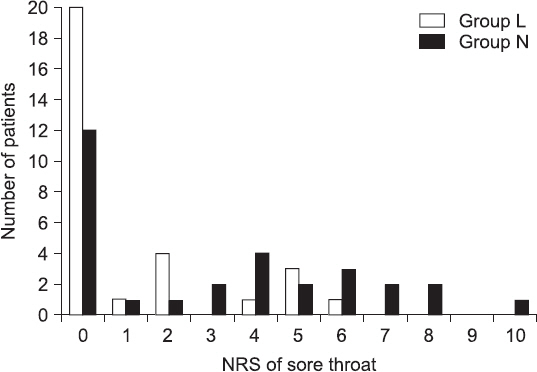
Sixty patients physical status American Society of Anesthesiologists classes I, II, and III who received a surgery under general anesthesia were randomly divided into two groups. L group was given 1% lidocaine 0.5 mg/kg by endotracheal administration. The other group, N group, received the same volume of normal saline. The number of cough, the severity of sore throat with numerical rating score (NRS), incidence of local anesthetic systemic toxic reaction, laryngospasm, and hoarseness were recorded. In addition, the number of coughs was divided into three levels by its severity, and it was converted into an indicator of cough score.
RESULTS
L group had a significantly lower number of cough and sore throat NRS (P value < 0.05) than the N group, and also hoarseness did not occur. The changes in the hemodynamic parameters, before and after the emergence of anesthesia, were more stable in the L group than those in the N group, but not statistically significant.
CONCLUSIONS
The results of this study suggest that endotracheal administration of 1% lidocaine is effective and safe method to reduce cough and sore throat caused by extubation.
Keyword
MeSH Terms
Figure
Reference
-
1. Leech P, Barker J, Fitch W. Proceedings: changes in intracranial pressure and systemic arterial pressure during the termination of anaesthesia. Br J Anaesth. 1974; 46:315–6. DOI: 10.1093/bja/46.4.315-a. PMID: 4451611.2. Asai T, Koga K, Vaughan RS. Respiratory complications associated with tracheal intubation and extubation. Br J Anaesth. 1998; 80:767–75. DOI: 10.1093/bja/80.6.767. PMID: 9771306.3. Holden R, Morsman CD, Butler J, Clark GS, Hughes DS, Bacon PJ. Intra-ocular pressure changes using the laryngeal mask airway and tracheal tube. Anaesthesia. 1991; 46:922–4. DOI: 10.1111/j.1365-2044.1991.tb09847.x. PMID: 1750590.4. Takita K, Morimoto Y, Kemmotsu O. Tracheal lidocaine attenuates the cardiovascular response to endotracheal intubation. Can J Anaesth. 2001; 48:732–6. DOI: 10.1007/BF03016686. PMID: 11546711.5. Jee D, Park SY. Lidocaine sprayed down the endotracheal tube attenuates the airway-circulatory reflexes by local anesthesia during emergence and extubation. Anesth Analg. 2003; 96:293–7. DOI: 10.1213/00000539-200301000-00058. PMID: 12505969.6. Ki YM, Kim NS, Lim SH, Kong MH, Kim HZ. The effect of lidocaine spray before endotracheal intubation on the incidence of cough and hemodynamics during emergence in children. Korean J Anesthesiol. 2007; 53:S1–6. DOI: 10.4097/kjae.2007.53.3.S1.7. McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999; 54:444–53. DOI: 10.1046/j.1365-2044.1999.00780.x.8. Bagchi D, Mandal MC, Das S, Sahoo T, Basu SR, Sarkar S. Efficacy of intravenous dexamethasone to reduce incidence of postoperative sore throat: a prospective randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2012; 28:477–80. DOI: 10.4103/0970-9185.101920. PMID: 23225928. PMCID: PMC3511945.9. Zhao G, Yin X, Li Y, Shao J. Continuous postoperative infusion of remifentanil inhibits the stress responses to tracheal extubation of patients under general anesthesia. J Pain Res. 2017; 10:933–9. DOI: 10.2147/JPR.S123423. PMID: 28458576. PMCID: PMC5402994.10. Soares SM, Arantes VM, Módolo MP, Dos Santos VJ, Vane LA, Navarro E, Lima LH, et al. The effects of tracheal tube cuffs filled with air, saline or alkalinised lidocaine on haemodynamic changes and laryngotracheal morbidity in children: a randomised, controlled trial. Anaesthesia. 2017; 72:496–503. DOI: 10.1111/anae.13764. PMID: 27987218.11. Bilotta F, Branca G, Lam A, Cuzzone V, Doronzio A, Rosa G. Endotracheal lidocaine in preventing endotracheal suctioning- induced changes in cerebral hemodynamics in patients with severe head trauma. Neurocrit Care. 2008; 8:241–6. DOI: 10.1007/s12028-007-9012-4. PMID: 17928962.12. Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999; 83:453–60. DOI: 10.1093/bja/83.3.453. PMID: 10655918.13. Frank SG, Lalonde DH. How acidic is the lidocaine we are injecting, and how much bicarbonate should we add? Can J Plast Surg. 2012; 20:71–3. DOI: 10.1177/229255031202000207. PMID: 23730153.14. Pelton DA, Daly M, Cooper PD, Conn AW. Plasma lidocaine concentrations following topical aerosol application to the trachea and bronchi. Can Anaesth Soc J. 1970; 17:250–5. DOI: 10.1007/BF03004603. PMID: 5512848.15. Herlevsen P, Bredahl C, Hindsholm K, Kruhøffer PK. Prophylactic laryngo-tracheal aerosolized lidocaine against postoperative sore throat. Acta Anaesthesiol Scand. 1992; 36:505–7. DOI: 10.1111/j.1399-6576.1992.tb03507.x. PMID: 1514331.16. Klemola UM, Saarnivaara L, Yrjölä H. Post-operative sore throat: effect of lignocaine jelly and spray with endotracheal intubation. Eur J Anaesthesiol. 1988; 5:391–9. PMID: 3240760.17. Oh YJ, Kim HK, Park DH. The effect of 10 % lidocaine spray on hemodynamics and postoperative sore throat accompanied by endotracheal intubation. Korean J Anesthesiol. 1996; 30:663–7. DOI: 10.4097/kjae.1996.30.6.663.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Lidocaine Spray before Endotracheal Intubation on the Incidence of Cough and Hemodynamics during Emergence in Children
- The Effect of Endotracheal Tube Cuff Filled with Lidocaine and Sodium Bicarbonate Mixture on Postoperative Sore Throat and Hoarseness Following General Endotracheal Anesthesia
- The Pharmacokinetics of Lidocaine after Tracheal Administration during General Anesthesia
- The Effect of Subtenons Lidocaine Injection and/or Preoperative Anxiety on Emergence Agitation after Sevoflurane Anesthesia in Pediatric Strabismus Surgery
- Effect of Intra-cuff 4% Lidocaine on the Dosage of Nitroglycerine Required to Maintain Hemodynamic Stability before and after Extubation in Patients with Hypertension