Anesth Pain Med.
2019 Apr;14(2):135-140. 10.17085/apm.2019.14.2.135.
Evaluation of suitability of fluid management using stroke volume variation in patients with prone position during lumbar spinal surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ansan Hospital, Korea University College of Medicine, Ansan, Korea. minware2@nate.com
- KMID: 2447960
- DOI: http://doi.org/10.17085/apm.2019.14.2.135
Abstract
- BACKGROUND
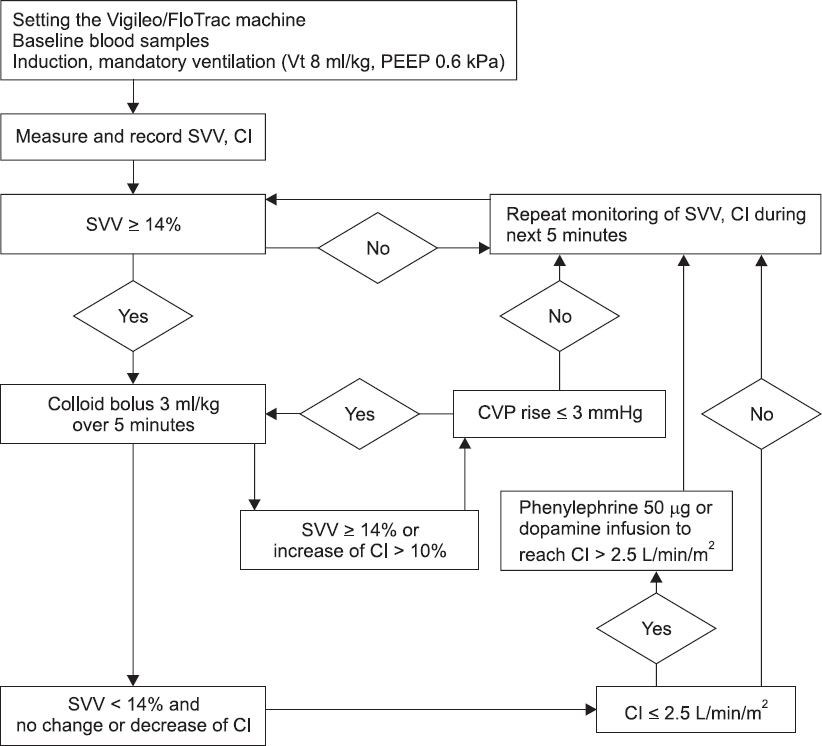
Static parameters such as central venous pressure and pulmonary artery occlusion pressure, have limitation in evaluation of patients' volume status. Dynamic parameters such as stroke volume variation (SVV), have been used to evaluate intraoperative hemodynamic volume status, in various operations. We examined if SVV is also effective for patients undergoing operation with prone position for fluid management.
METHODS
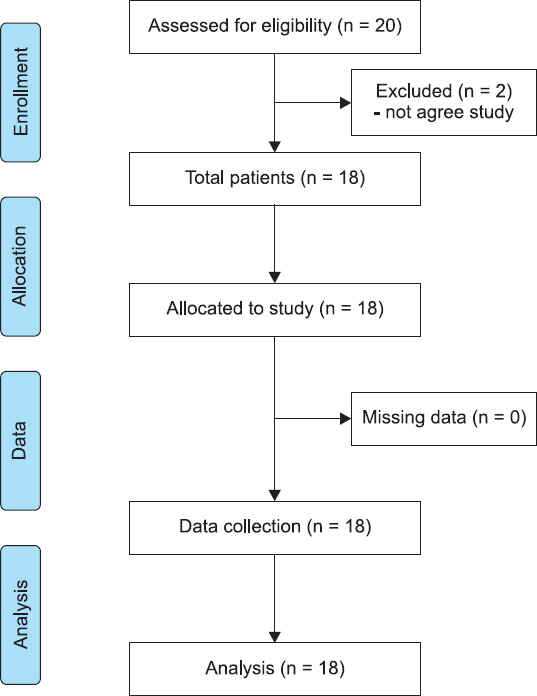
Eighteen patients that received spinal surgery under prone position November 2015 to May 2016, were enrolled. Patients were kept at an SVV value less than 14% during surgery. Changes of pre-, post-operative volume status were evaluated, using transthoracic echocardiography.
RESULTS
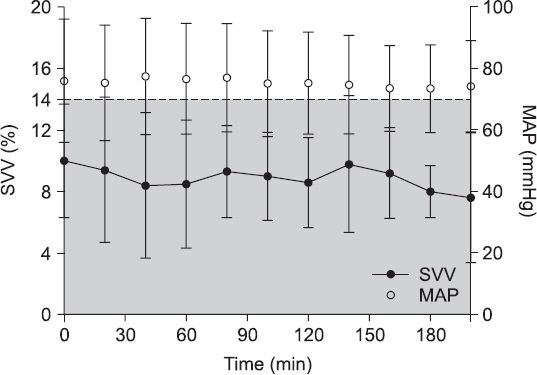
Mean fluid administered was 1,731.97 ± 792.38 ml. Left ventricular end-diastolic volume was 72.85 ± 13.50 ml before surgery, and 70.84 ± 15.00 ml after surgery (P value = 0.594). Right ventricular end-diastolic area was 15.56 ± 1.71 cm² before surgery, and 13.52 ± 2.65 cm² after surgery (P value = 0.110). Inferior vena cava diameter was 14.99 ± 1.74 mm before surgery, and 13.57 ± 2.83 mm after surgery (P value = 0.080).
CONCLUSIONS
We can confirm that fluid management based on SVV is effective, even in prone position surgery. So, SVV, that can be measured by continuous arterial pressure, can be considered a guideline for effective fluid management in spinal surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Cole R. Does central venous pressure predict fluid responsiveness? Chest. 2008; 134:1351–2. DOI: 10.1378/chest.08-1846. PMID: 19059974.2. Kumar A, Anel R, Bunnell E, Habet K, Zanotti S, Marshall S, et al. Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med. 2004; 32:691–9. DOI: 10.1097/01.CCM.0000114996.68110.C9. PMID: 15090949.3. Kim SH, Hwang GS, Kim SO, Kim YK. Is stroke volume variation a useful preload index in liver transplant recipients?A retrospective analysis. Int J Med Sci. 2013; 10:751–7. DOI: 10.7150/ijms.6074. PMID: 23630440. PMCID: PMC3638299.4. Kim YK, Shin WJ, Song JG, Jun IG, Hwang GS. Does stroke volume variation predict intraoperative blood loss in living right donor hepatectomy? Transplant Proc. 2011; 43:1407–11. DOI: 10.1016/j.transproceed.2011.02.056. PMID: 21693206.5. Gelman S. Venous function and central venous pressure: a physiologic story. Anesthesiology. 2008; 108:735–48. DOI: 10.1097/ALN.0b013e3181672607. PMID: 18362606.6. Toyoda D, Fukuda M, Iwasaki R, Terada T, Sato N, Ochiai R, et al. The comparison between stroke volume variation and filling pressure as an estimate of right ventricular preload in patients undergoing renal transplantation. J Anesth. 2015; 29:40–6. DOI: 10.1007/s00540-014-1870-2. PMID: 24962946.7. Drvar Z, Pavlek M, Drvar V, Tomasević B, Baronica R, Perić M. [Stroke volume and pulse pressure variation are good predictors of fluid responsiveness in sepsis patients]. Acta Med Croatica. 2013; 67:407–14. Croatian. PMID: 24979881.8. Dudeja RK. Predictability of stroke volume variation. Br J Anaesth. 2015; 114:346–7. DOI: 10.1093/bja/aeu474. PMID: 25596224.9. Bahlool SA. Respiratory stroke volume variation and fluid responsiveness: how applicable is this? Br J Anaesth. 2015; 114:169. DOI: 10.1093/bja/aeu427. PMID: 25500407.10. Peng K, Li J, Cheng H, Ji FH. Goal-directed fluid therapy based on stroke volume variations improves fluid management and gastrointestinal perfusion in patients undergoing major orthopedic surgery. Med Princ Pract. 2014; 23:413–20. DOI: 10.1159/000363573. PMID: 24994571. PMCID: PMC5586912.11. Kreit JW. Systolic blood pressure variation during mechanical ventilation. Ann Am Thorac Soc. 2014; 11:462–5. DOI: 10.1513/AnnalsATS.201312-439CC. PMID: 24673702.12. Hong JQ, He HF, Chen ZY, Du ZS, Liu WF, Weng PQ, et al. Comparison of stroke volume variation with pulse pressure variation as a diagnostic indicator of fluid responsiveness in mechanically ventilated critically ill patients. Saudi Med J. 2014; 35:261–8. PMID: 24623206.13. Slagt C, Malagon I, Groeneveld AB. Systematic review of uncalibrated arterial pressure waveform analysis to determine cardiac output and stroke volume variation. Br J Anaesth. 2014; 112:626–37. DOI: 10.1093/bja/aet429. PMID: 24431387.14. Benes J, Chytra I, Altmann P, Hluchy M, Kasal E, Svitak R, et al. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care. 2010; 14:R118. DOI: 10.1186/cc9070. PMID: 20553586. PMCID: PMC2911766.15. Meregalli A, Oliveira RP, Friedman G. Occult hypoperfusion is associated with increased mortality in hemodynamically stable, high-risk, surgical patients. Crit Care. 2004; 8:R60–5. DOI: 10.1186/cc2423. PMID: 15025779. PMCID: PMC420024.16. Davies SJ, Wilson RJ. Preoperative optimization of the high-risk surgical patient. Br J Anaesth. 2004; 93:121–8. DOI: 10.1093/bja/aeh164. PMID: 15121729.17. Tote SP, Grounds RM. Performing perioperative optimization of the high-risk surgical patient. Br J Anaesth. 2006; 97:4–11. DOI: 10.1093/bja/ael102. PMID: 16751640.18. Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445]. Crit Care. 2005; 9:R687–93. DOI: 10.1186/cc3887. PMID: 16356219. PMID: PMC1414018.19. Daihua Y, Wei C, Xude S, Linong Y, Changjun G, Hui Z. The effect of body position changes on stroke volume variation in 66 mechanically ventilated patients with sepsis. J Crit Care. 2012; 27:416.e7–12. DOI: 10.1016/j.jcrc.2012.02.009. PMID: 22459159.20. Berger K, Francony G, Bouzat P, Halle C, Genty C, Oddoux M, et al. Prone position affects stroke volume variation performance in predicting fluid responsiveness in neurosurgical patients. Minerva Anestesiol. 2015; 81:628–35. PMID: 25263024.21. Biais M, Bernard O, Ha JC, Degryse C, Sztark F. Abilities of pulse pressure variations and stroke volume variations to predict fluid responsiveness in prone position during scoliosis surgery. Br J Anaesth. 2010; 104:407–13. DOI: 10.1093/bja/aeq031. PMID: 20190260.22. Ilyas A, Ishtiaq W, Assad S, Ghazanfar H, Mansoor S, Haris M, et al. Correlation of IVC diameter and collapsibility index with central venous pressure in the assessment of intravascular volume in critically ill patients. Cureus. 2017; 9:e1025. DOI: 10.7759/cureus.1025. PMID: 2834894. PMCID: PMC5346017.23. Aurich M, André F, Keller M, Greiner S, Hess A, Buss SJ, et al. Assessment of left ventricular volumes with echocardiography and cardiac magnetic resonance imaging: real-life evaluation of standard versus new semiautomatic methods. J Am Soc Echocardiogr. 2014; 27:1017–24. DOI: 10.1016/j.echo.2014.07.006. PMID: 25129394.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Effects of Free Movement of Abdominal Muscle in Prone Positioning during General Anesthesia
- Changes in the hemodynamic parameters between the prone and supine positions measured by an arterial pulse contour cardiac output monitoring system
- Effect of Volume on Hypobaric Spinal Anesthesia for Perianal Surgery with Prone Jacknife Position
- Comparative Study of Isobaric Bupivacaine Spinal Anesthesia in the Supine and Prone Positions
- Comparison between isobaric and hypobaric spinal anesthesia with tetracaine for lumbar laminectomy in prone position