Anesth Pain Med.
2019 Apr;14(2):123-134. 10.17085/apm.2019.14.2.123.
Anesthetic management for interventional neuroradiology
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Dongguk University Ilsan Hospital, Goyang, Korea. cjanes@naver.com
- KMID: 2447959
- DOI: http://doi.org/10.17085/apm.2019.14.2.123
Abstract
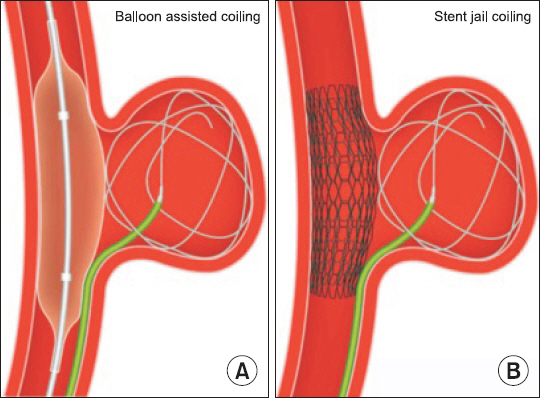
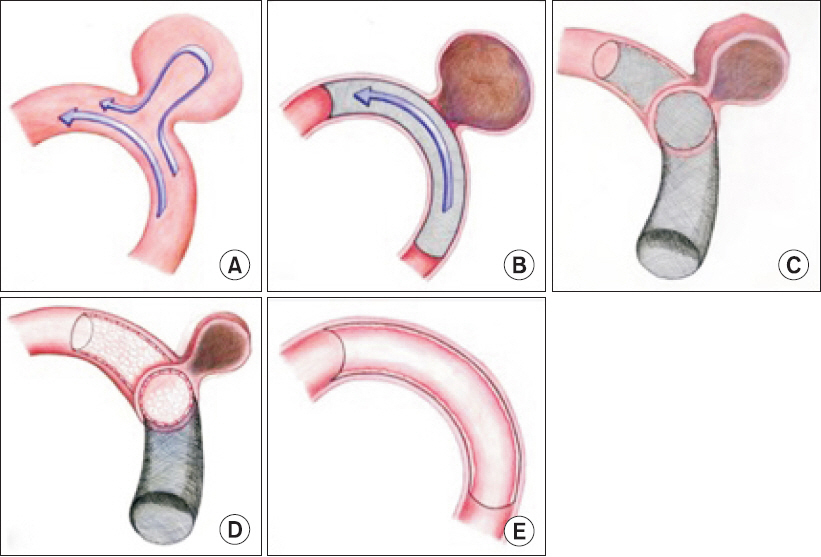
- With the field of neuroradiological procedures consistently expanding, breaking the border between the medical and surgical treatment, anesthetic involvement in those procedures is also increasing, which underscores the importance of related anesthesia management. The objective of this study is to review the closing or open endovascular procedures for intracranial aneurysm, arteriovenous malformation, acute ischemic stroke, and carotid stenosis and related anesthetic implications.
Keyword
MeSH Terms
Figure
Reference
-
1. Anastasian ZH, Strozyk D, Meyers PM, Wang S, Berman MF. Radiation exposure of the anesthesiologist in the neurointerventional suite. Anesthesiology. 2011; 114:512–20. DOI: 10.1097/ALN.0b013e31820c2b81. PMID: 21285864.2. Brinjikji W, Pasternak J, Murad MH, Cloft HJ, Welch TL, Kallmes DF, et al. Anesthesia-related outcomes for endovascular stroke revascularization: a systematic review and meta-analysis. Stroke. 2017; 48:2784–91. DOI: 10.1161/STROKEAHA.117.017786. PMID: 28904228.3. Simonsen CZ, Yoo AJ, Sørensen LH, Juul N, Johnsen SP, Andersen G, et al. Effect of general anesthesia and conscious sedation during endovascular therapy on infarct growth and clinical outcomes in acute ischemic stroke: a randomized clinical trial. JAMA Neurol. 2018; 75:470–7. DOI: 10.1001/jamaneurol.2017.4474. PMID: 29340574. PMCID: PMC5885172.4. Davenport MS, McDonald RJ, Asch D, Mervak B, Cavallo J, Mody R, et al. ACR manual on contrast media [serial on the Internet]. 2018. [2019 Jan 21]. Available from https://www.acr.org/-/media/ ACR/Files/Clinical-Resources/Contrast_Media.pdf#page=7 .5. Teitelbaum GP, Larsen DW, Zelman V, Lysachev AG, Likhterman LB. A tribute to Dr. Fedor A. Serbinenko, founder of endovascular neurosurgery. Neurosurgery. 2000; 46:462–9. DOI: 10.1097/00006123-200002000-00037. PMID: 10690736.6. Guglielmi G, Viñuela F, Dion J, Duckwiler G. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Pre- liminary clinical experience. J Neurosurg. 1991; 75:8–14. DOI: 10.3171/jns.1991.75.1.0008. PMID: 2045924.7. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002; 360:1267–74. DOI: 10.1016/S0140-6736(02)11314-6.8. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet. 2015; 385:691–7. DOI: 10.1016/S0140-6736(14)60975-2. PMID: 2546511. PMCID: PMC4356153.9. McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, et al. The barrow ruptured aneurysm trial. J Neurosurg. 2012; 116:135–44. DOI: 10.3171/2011.8.JNS101767. PMID: 22054213.10. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; 362:103–10. DOI: 10.1016/S0140-6736(03)13860-3.11. Naggara ON, White PM, Guilbert F, Roy D, Weill A, Raymond J. Endovascular treatment of intracranial unruptured aneurysms: systematic review and meta-analysis of the literature on safety and efficacy. Radiology. 2010; 256:887–97. DOI: 10.1148/radiol.10091982. PMID: 20634431.12. Pierot L, Spelle L, Vitry F. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach: results of the ATENA study. Stroke. 2008; 39:2497–504. DOI: 10.1161/STROKEAHA.107.512756. PMID: 18617659.13. Molyneux AJ, Kerr RS, Birks J, Ramzi N, Yarnold J, Sneade M, et al. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol. 2009; 8:427–33. DOI: 10.1016/S1474-4422(09)70080-8. PMID: 19329361. PMCID: PMC2669592.14. Schaafsma JD, Sprengers ME, van Rooij WJ, Sluzewski M, Majoie CB, Wermer MJ, et al. Long-term recurrent subarachnoid hemorrhage after adequate coiling versus clipping of ruptured intracranial aneurysms. Stroke. 2009; 40:1758–63. DOI: 10.1161/STROKEAHA.108.524751. PMID: 19286603.15. Taki W. PRESAT group. Factors predicting retreatment and residual aneurysms at 1 year after endovascular coiling for ruptured cerebral aneurysms: Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) in Japan. Neuroradiology. 2012; 54:597–606. DOI: 10.1007/s00234-011-0945-0. PMID: 21861080.16. Eskridge JM, Song JK. Endovascular embolization of 150 basilar tip aneurysms with Guglielmi detachable coils: results of the Food and Drug Administration multicenter clinical trial. J Neurosurg. 1998; 89:81–6. DOI: 10.3171/jns.1998.89.1.0081. PMID: 9647176.17. Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years’ experience. J Neurosurg. 2003; 98:959–66. DOI: 10.3171/jns.2003.98.5.0959. PMID: 12744354.18. Bohman LE, Winn HR, LeRoux PD. Surgical decision making for the treatment of intracranial aneurysms. Youmans and Winn neurological surgery. 7th ed. Winn HR, editor. Philadelphia: Elservier;2017. p. 3248–56.19. Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G. European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 2013; 35:93–112. DOI: 10.1159/000346087. PMID: 23406828.20. White PM, Lewis SC, Gholkar A, Sellar RJ, Nahser H, Cognard C, et al. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet. 2011; 377:1655–62. DOI: 10.1016/S0140-6736(11)60408-X. PMID: 21571149.21. Molyneux AJ, Clarke A, Sneade M, Mehta Z, Coley S, Roy D, et al. Cerecyte coil trial: angiographic outcomes of a prospective randomized trial comparing endovascular coiling of cerebral aneurysms with either cerecyte or bare platinum coils. Stroke. 2012; 43:2544–50. DOI: 10.1161/STROKEAHA.112.657254. PMID: 22836352.22. McDougall CG, Johnston SC, Gholkar A, Barnwell SL, Vazquez Suarez JC, MassóRomero J, et al. Bioactive versus bare platinum coils in the treatment of intracranial aneurysms: the MAPS (Matrix and Platinum Science) trial. AJNR Am J Neuroradiol. 2014; 35:935–42. DOI: 10.3174/ajnr.A3857. PMID: 24481333.23. Bechan RS, Sprengers ME, Majoie CB, Peluso JP, Sluzewski M, van Rooij WJ. Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. AJNR Am J Neuroradiol. 2016; 37:502–7. DOI: 10.3174/ajnr.A4542. PMID: 26405089.24. Zhao J, Lin H, Summers R, Yang M, Cousins B, Tsui J. Current treatment strategies for intracranial aneurysms: an overview. Angiology. 2018; 69:17–30. DOI: 10.1177/0003319717700503. PMID: 28355880. PMCID: PMC5724574.25. Jiang B, Paff M, Colby GP, Coon AL, Lin LM. Cerebral aneurysm treatment: modern neurovascular techniques. Stroke Vasc Neurol. 2016; 1:93–100. DOI: 10.1136/svn-2016-000027. PMID: 28959469. PMCID: PMC5435202.26. Cagnazzo F, di Carlo DT, Cappucci M, Lefevre PH, Costalat V, Perrini P. Acutely ruptured intracranial aneurysms treated with flow-diverter stents: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2018; 39:1669–75. DOI: 10.3174/ajnr.A5804. DOI: 10.3174/ajnr.A5730. PMID: 30049721.27. Gawlitza M, Januel AC, Tall P, Bonneville F, Cognard C. Flow diversion treatment of complex bifurcation aneurysms beyond the circle of Willis: a single-center series with special emphasis on covered cortical branches and perforating arteries. J Neurointerv Surg. 2016; 8:481–7. DOI: 10.1136/neurintsurg-2015-011682. PMID: 25878068.28. Chang HW, Shin SH, Suh SH, Kim BS, Rho MH. Cost-effectiveness analysis of endovascular coiling versus neurosurgical clipping for intracranial aneurysms in Republic of Korea. Neurointervention. 2016; 11:86–91. DOI: 10.5469/neuroint.2016.11.2.86. PMID: 27621944. PMCID: PMC5018553.29. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012; 43:1711–37. DOI: 10.1161/STR.0b013e3182587839. PMID: 22556195.30. van Rooij WJ, Sluzewski M, Beute GN, Nijssen PC. Procedural complications of coiling of ruptured intracranial aneurysms: incidence and risk factors in a consecutive series of 681 patients. AJNR Am J Neuroradiol. 2006; 27:1498–501. PMID: 16908567.31. Shigematsu T, Fujinaka T, Yoshimine T, Imamura H, Ishii A, Sakai C, et al. Endovascular therapy for asymptomatic unruptured intracranial aneurysms. JR-NET and JR-NET2 findings. Stroke. 2013; 44:2735–42. DOI: 10.1161/STROKEAHA.111.000609. PMID: 23899916.32. Athar MK, Levine JM. Treatment options for cerebral vasospasm in aneurysmal subarachnoid hemorrhage. Neurotherapeutics. 2012; 9:37–43. DOI: 10.1007/s13311-011-0098-1. PMID: 22215324. PMCID: PMC3271157.33. Rosenwasser RH, Armonda RA, Thomas JE, Benitez RP, Gannon PM, Harrop J. Therapeutic modalities for the management of cerebral vasospasm: timing of endovascular options. Neurosurgery. 1999; 44:975–9. DOI: 10.1097/00006123-199905000-00022. PMID: 10232530.34. Chalouhi N, Tjoumakaris S, Thakkar V, Theofanis T, Hammer C, Hasan D, et al. Endovascular management of cerebral vasospasm following aneurysm rupture: outcomes and predictors in 116 patients. Clin Neurol Neurosurg. 2014; 118:26–31. DOI: 10.1016/j.clineuro.2013.12.012. PMID: 24529225.35. Lv X, Wu Z, Li Y, Jiang C, Yang X, Zhang J. Cerebral arteriovenous malformations associated with flow-related and circle of Willis aneurysms. World Neurosurg. 2011; 76:455–8. DOI: 10.1016/j.wneu.2011.04.015. PMID: 22152575.36. D’Aliberti G, Talamonti G, Cenzato M, La Camera A, Debernardi A, Valvassori L, et al. Arterial and venous aneurysms associated with arteriovenous malformations. World Neurosurg. 2015; 83:188–96. DOI: 10.1016/j.wneu.2014.05.037. PMID: 24915068.37. Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 2014; 383:614–21. DOI: 10.1016/S0140-6736(13)62302-8. PMID: 24268105. PMCID: PMC4119885.38. Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 2008; 108:186–93. DOI: 10.3171/JNS/2008/108/01/0186. PMID: 18173333.39. Spetzler RF, Ponce FA. A 3-tier classification of cerebral arteriovenous malformations. Clinical article. J Neurosurg. 2011; 114:842–9. DOI: 10.3171/2010.8.JNS10663. PMID: 20932095.40. Elsenousi A, Aletich VA, Alaraj A. Neurological outcomes and cure rates of embolization of brain arteriovenous malformations with n-butyl cyanoacrylate or Onyx: a meta-analysis. J Neurointerv Surg. 2016; 8:265–72. DOI: 10.1136/neurintsurg-2014-011427. PMID: 25540177.41. Derdeyn CP, Zipfel GJ, Albuquerque FC, Cooke DL, Feldmann E, Sheehan JP, et al. Management of brain arteriovenous malformations: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017; 48:e200–24. DOI: 10.1161/STR.0000000000000134. PMID: 28642352.42. Krings T, Hans FJ, Geibprasert S, Terbrugge K. Partial “targeted” embolisation of brain arteriovenous malformations. Eur Radiol. 2010; 20:2723–31. DOI: 10.1007/s00330-010-1834-3. PMID: 20535613. PMCID: PMC2948167.43. Saatci I, Geyik S, Yavuz K, Cekirge HS. Endovascular treatment of brain arteriovenous malformations with prolonged intranidal Onyx injection technique: long-term results in 350 consecutive patients with completed endovascular treatment course. J Neurosurg. 2011; 115:78–88. DOI: 10.3171/2011.2.JNS09830. PMID: 21476804.44. van Rooij WJ, Jacobs S, Sluzewski M, van der Pol B, Beute GN, Sprengers ME. Curative embolization of brain arteriovenous malformations with onyx: patient selection, embolization technique, and results. AJNR Am J Neuroradiol. 2012; 33:1299–304. DOI: 10.3174/ajnr.A2947. PMID: 22383233.45. Pierot L, Cognard C, Herbreteau D, Fransen H, van Rooij WJ, Boccardi E, et al. Endovascular treatment of brain arteriovenous malformations using a liquid embolic agent: results of a prospective, multicentre study (BRAVO). Eur Radiol. 2013; 23:2838–45. DOI: 10.1007/s00330-013-2870-6. PMID: 23652849.46. Yoo AJ, Andersson T. Thrombectomy in acute ischemic stroke: challenges to procedural success. J Stroke. 2017; 19:121–30. DOI: 10.5853/jos.2017.00752. PMID: 28592779. PMCID: PMC5466290.47. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–110. DOI: 10.1161/STR.0000000000000172. PMID: 29669864.48. Leonardi-Bee J, Bath PM, Phillips SJ, Sandercock PA. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke. 2002; 33:1315–20. DOI: 10.1161/01.STR.0000014509.11540.66. PMID: 11988609.49. Talke PO, Sharma D, Heyer EJ, Bergese SD, Blackham KA, Ste-vens RD. Society for Neuroscience in Anesthesiology and Critical Care Expert consensus statement: anesthetic management of endovascular treatment for acute ischemic stroke: endorsed by the Society of NeuroInterventional Surgery and the Neurocritical Care Society. J Neurosurg Anesthesiol. 2014; 26:95–108. DOI: 10.1097/ANA.0000000000000042. PMID: 24594652.50. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014; 129:e28–292. DOI: 10.1161/01.cir.0000441139.02102.80. PMID: 24352519. PMCID: PMC5408159.51. Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001; 32:2735–40. DOI: 10.1161/hs1201.100209. PMID: 11739965.52. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004; 351:1493–501. DOI: 10.1056/NEJMoa040127. PMID: 15470212.53. Mantese VA, Timaran CH, Chiu D, Begg RJ, Brott TG. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): stenting versus carotid endarterectomy for carotid disease. Stroke. 2010; 41:S31–4. DOI: 10.1161/STROKEAHA.110.595330. PMID: 20876500. PMCID: PMC3058352.54. Naylor AR, Ricco JB, de Borst GJ, Debus S, de Haro J, Halliday A, et al. Editor's choice management of atherosclerotic carotid and vertebral artery disease: 2017 clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2018; 55:3–81. DOI: 10.1016/j.ejvs.2017.06.021. PMID: 28851594.55. Munich SA, Mokin M, Krishna C, Siddiqui AH. Carotid artery angioplasty and stenting. Youmans and Winn neurological surgery. 7th ed. Winn HR, editor. Philadelphia: Elservier;2017. p. 3113.56. Dumont TM, Rughani AI. National trends in carotid artery revascularization surgery. J Neurosurg. 2012; 116:1251–7. DOI: 10.3171/2012.3.JNS111320. PMID: 22482791.57. Cho SS, Joh JH, Ahn HJ, Park HC. National trends in carotid end-arterectomy and stenting in Korea from 2004 to 2013. Exp Ther Med. 2016; 12:2639–43. DOI: 10.3892/etm.2016.3637. PMID: 27698767. PMCID: PMC5038473.58. Huibers AE, Westerink J, de Vries EE, Hoskam A, den Ruijter HM, Moll FL, et al. Editor's choice cerebral hyperperfusion syndrome after carotid artery stenting: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2018; 56:322–33. DOI: 10.1016/j.ejvs.2018.05.012. PMID: 30196814.59. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365:993–1003. DOI: 10.1056/NEJMoa1105335. PMID: 21899409. PMCID: PMC3552515.60. Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS, et al. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMM- PRIS): the final results of a randomised trial. Lancet. 2014; 383:333–41. DOI: 10.1016/S0140-6736(13)62038-3. PMID: 24168957. PMCID: PMC3971471.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic Consideration for Neurointerventional Procedures
- Erratum: Susceptibility Vessel Sign in the ASTER Trial: Higher Recanalization Rate and More Favourable Clinical Outcome after First Line Stent Retriever Compared to Contact Aspiration
- Perspectives on Fellowship Training Standard in Interventional Neuroradiology
- The optimal anesthetic depth for interventional neuroradiology: comparisons between light anesthesia and deep anesthesia
- The Value of Transcranial Doppler Sonography in Hyperperfusion Syndrome after Carotid Artery Stenting: A Nationwide Prospective Study