Neurointervention.
2019 Mar;14(1):17-26. 10.5469/neuroint.2019.00045.
Influence of Anesthesia Type on Outcomes after Endovascular Treatment in Acute Ischemic Stroke: Meta-Analysis
- Affiliations
-
- 1Department of Neurology, Hallym University College of Medicine, Chuncheon, Korea.
- 2Department of Emergency Medicine, Seoul Emergency Operations Center, Seoul, Korea.
- 3Department of Neurosurgery, Hallym University College of Medicine, Chuncheon, Korea. jjs6553@daum.net
- 4Institute of New Frontier Stroke Research, Hallym University College of Medicine, Chuncheon, Korea.
- 5Genetic and Research, Hallym University College of Medicine, Chuncheon, Korea.
- KMID: 2446778
- DOI: http://doi.org/10.5469/neuroint.2019.00045
Abstract
- PURPOSE
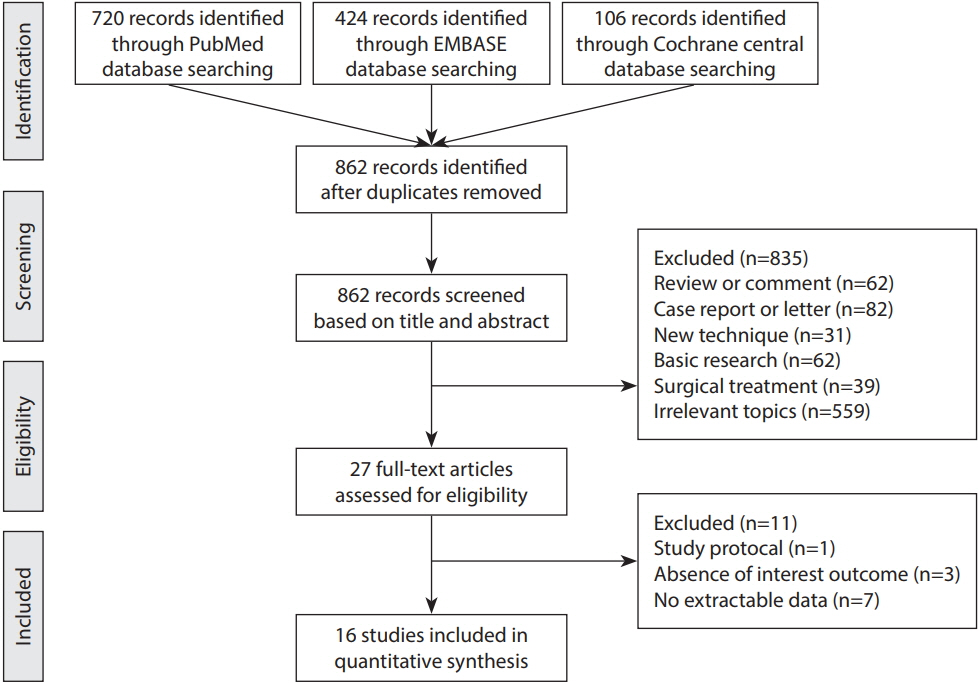
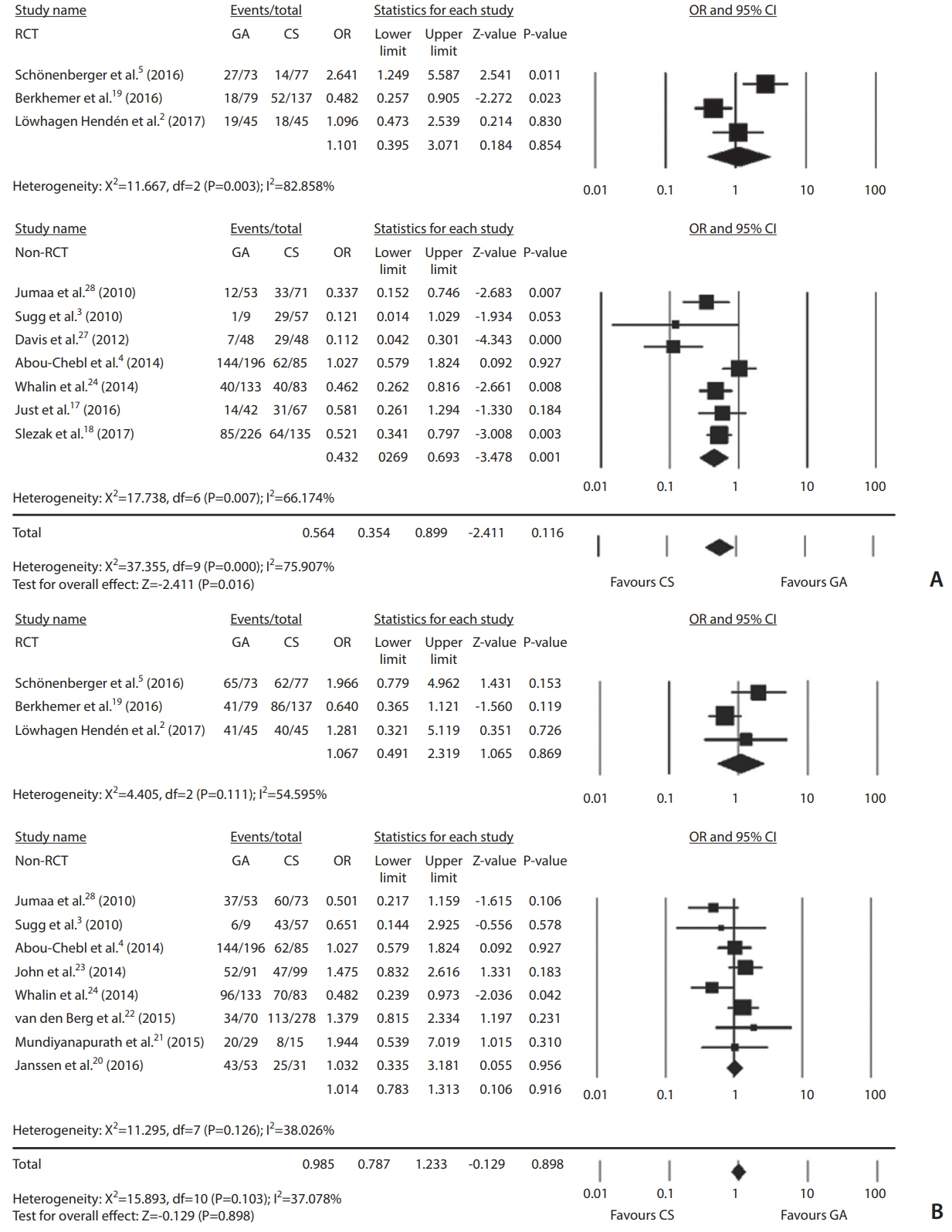
To assess clinical and angiographic outcomes after endovascular treatment (EVT) in ischemic stroke patients according to anesthesia types (general anesthesia vs. conscious sedation). MATERIALS AND METHODS: A systematic literature review through an online data base between January 1990 and September 2017 was performed. A fixed effect model was used in cases of <50% heterogeneity. The primary outcomes were good clinical outcome at the 3-month follow-up and successful recanalization. A meta-regression analysis was done to estimate primary outcomes of log odds ratio (OR) on onset-to-puncture time (OTP) differences. Publication bias was determined using Begg's funnel plot and additional the Trim and Fill method.
RESULTS
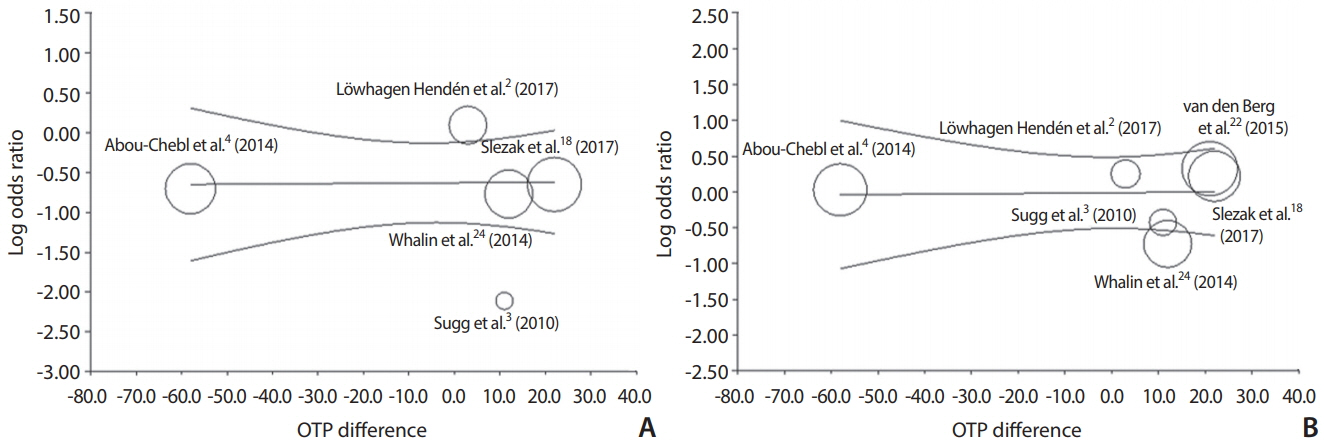
Sixteen articles including 2,662 patients (general anesthesia, n=1,275; conscious sedation, n=1,387) were included. General anesthesia significantly decreased good outcomes than conscious sedation (OR, 0.564; 95% confidence interval [CI], 0.354-0.899). However, outcomes did not differ significantly in randomized controlled trials (RCTs; OR, 1.101; 95% CI, 0.395-3.071). Anesthesia type was not associated with successful recanalization (OR, 0.985; 95% CI, 0.787-1.233). General anesthesia increased the risk of mortality (OR, 1.532; 95% CI, 1.187-1.976) and pneumonia (OR, 1.613; 95% CI, 1.172-2.221), but not symptomatic intracranial hemorrhage (OR, 1.125; 95% CI, 0.767-1.652). The meta-regression analysis showed no linear relationship between OTP differences and log OR of good outcome (coefficient, 0.0004; P=0.95) or successful recanalization (coefficient, 0.0005; P=0.94), respectively.
CONCLUSION
General anesthesia seemed to be associated with adverse clinical outcome after EVT. However, its efficacy was not demonstrated in RCTs. Successful recanalization did not differ according to anesthesia type. Studies using individual patient data based on further RCTs are necessary to elucidate anesthesia effect on procedural and clinical outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Löwhagen Hendén P, Rentzos A, Karlsson JE, Rosengren L, Leiram B, Sundeman H, et al. General anesthesia versus conscious sedation for endovascular treatment of acute ischemic stroke: the AnStroke trial (anesthesia during stroke). Stroke. 2017; 48:1601–1607.
Article3. Sugg RM, Jackson AS, Holloway W, Martin CO, Akhtar N, Rymer M. Is mechanical embolectomy performed in nonanesthetized patients effective? AJNR Am J Neuroradiol. 2010; 31:1533–1535.
Article4. Abou-Chebl A, Zaidat OO, Castonguay AC, Gupta R, Sun CH, Martin CO, et al. North American SOLITAIRE stent-retriever acute stroke registry: choice of anesthesia and outcomes. Stroke. 2014; 45:1396–1401.
Article5. Schönenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S, Purrucker JC, et al. Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA. 2016; 316:1986–1996.6. Brinjikji W, Murad MH, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF. Conscious sedation versus general anesthesia during endovascular acute ischemic stroke treatment: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015; 36:525–529.
Article7. Rodrigues FB, Neves JB, Caldeira D, Ferro JM, Ferreira JJ, Costa J. Endovascular treatment versus medical care alone for ischaemic stroke: systematic review and meta-analysis. BMJ. 2016; 353:i1754.
Article8. Jeon JP, Kim JE, Cho WS, Bang JS, Son YJ, Oh CW. Meta-analysis of the surgical outcomes of symptomatic moyamoya disease in adults. J Neurosurg. 2018; 128:793–799.
Article9. Abou-Chebl A, Yeatts SD, Yan B, Cockroft K, Goyal M, Jovin T, et al. Impact of general anesthesia on safety and outcomes in the endovascular arm of interventional management of stroke (IMS) III trial. Stroke. 2015; 46:2142–2148.
Article10. Nichols C, Carrozzella J, Yeatts S, Tomsick T, Broderick J, Khatri P. Is periprocedural sedation during acute stroke therapy associated with poorer functional outcomes? J Neurointerv Surg. 2010; 2:67–70.
Article11. Langner S, Khaw AV, Fretwurst T, Angermaier A, Hosten N, Kirsch M. Endovascular treatment of acute ischemic stroke under conscious sedation compared to general anesthesia - safety, feasibility and clinical and radiological outcome. Rofo. 2013; 185:320–327.12. Almekhlafi MA, Menon BK, Freiheit EA, Demchuk AM, Goyal M. A meta-analysis of observational intra-arterial stroke therapy studies using the merci device, penumbra system, and retrievable stents. AJNR Am J Neuroradiol. 2013; 34:140–145.
Article13. Lapergue B, Blanc R, Guedin P, Decroix JP, Labreuche J, Preda C, et al. A direct aspiration, first pass technique (ADAPT) versus stent retrievers for acute stroke therapy: an observational comparative study. AJNR Am J Neuroradiol. 2016; 37:1860–1865.
Article14. Kim CH, Jeon JP, Kim SE, Choi HJ, Cho YJ. Endovascular treatment with intravenous thrombolysis versus endovascular treatment alone for acute anterior circulation stroke : a meta-analysis of observational studies. J Korean Neurosurg Soc. 2018; 61:467–473.
Article15. Cho YD, Kim SE, Lim JW, Choi HJ, Cho YJ, Jeon JP. Protected versus unprotected carotid artery stenting : meta-analysis of the current literature. J Korean Neurosurg Soc. 2018; 61:458–466.
Article16. Kim SE, Kim BJ, Cho SS, Kim HC, Jeon JP. The incidence of hydrocephalus and shunting in patients with angiogram-negative subarachnoid hemorrhage: an updated meta-analysis. World Neurosurg. 2018; 119:e216. –e227.
Article17. Just C, Rizek P, Tryphonopoulos P, Pelz D, Arango M. Outcomes of general anesthesia and conscious sedation in endovascular treatment for stroke. Can J Neurol Sci. 2016; 43:655–658.
Article18. Slezak A, Kurmann R, Oppliger L, Broeg-Morvay A, Gralla J, Schroth G, et al. Impact of anesthesia on the outcome of acute ischemic stroke after endovascular treatment with the solitaire stent retriever. AJNR Am J Neuroradiol. 2017; 38:1362–1367.
Article19. Berkhemer OA, van den Berg LA, Fransen PS, Beumer D, Yoo AJ, Lingsma HF, et al. The effect of anesthetic management during intra-arterial therapy for acute stroke in MR CLEAN. Neurology. 2016; 87:656–664.
Article20. Janssen H, Buchholz G, Killer M, Ertl L, Bruckmann H, Lutz J. General anesthesia versus conscious sedation in acute stroke treatment: the importance of head immobilization. Cardiovasc Intervent Radiol. 2016; 39:1239–1244.
Article21. Mundiyanapurath S, Schonenberger S, Rosales ML, Carrilho Romeiro AM, Möhlenbruch M, Bendszus M, et al. Circulatory and respiratory parameters during acute endovascular stroke therapy in conscious sedation or general anesthesia. J Stroke Cerebrovasc Dis. 2015; 24:1244–1249.
Article22. van den Berg LA, Koelman DL, Berkhemer OA, Rozeman AD, Fransen PS, Beumer D, et al. Type of anesthesia and differences in clinical outcome after intra-arterial treatment for ischemic stroke. Stroke. 2015; 46:1257–1262.
Article23. John S, Thebo U, Gomes J, Saqqur M, Farag E, Xu J, et al. Intra-arterial therapy for acute ischemic stroke under general anesthesia versus monitored anesthesia care. Cerebrovasc Dis. 2014; 38:262–267.
Article24. Whalin MK, Lopian S, Wyatt K, Sun CH, Nogueira RG, Glenn BA, et al. Dexmedetomidine: a safe alternative to general anesthesia for endovascular stroke treatment. J Neurointerv Surg. 2014; 6:270–275.
Article25. Li F, Deshaies EM, Singla A, Villwock MR, Melnyk V, Gorji R, et al. Impact of anesthesia on mortality during endovascular clot removal for acute ischemic stroke. J Neurosurg Anesthesiol. 2014; 26:286–290.
Article26. Hassan AE, Chaudhry SA, Zacharatos H, Khatri R, Akbar U, Suri MF, et al. Increased rate of aspiration pneumonia and poor discharge outcome among acute ischemic stroke patients following intubation for endovascular treatment. Neurocrit Care. 2012; 16:246–250.
Article27. Davis MJ, Menon BK, Baghirzada LB, Campos-Herrera CR, Goyal M, Hill MD, et al. Anesthetic management and outcome in patients during endovascular therapy for acute stroke. Anesthesiology. 2012; 116:396–405.
Article28. Jumaa MA, Zhang F, Ruiz-Ares G, Gelzinis T, Malik AM, Aleu A, et al. Comparison of safety and clinical and radiographic outcomes in endovascular acute stroke therapy for proximal middle cerebral artery occlusion with intubation and general anesthesia versus the nonintubated state. Stroke. 2010; 41:1180–1184.
Article29. Gupta R. Local is better than general anesthesia during endovascular acute stroke interventions. Stroke. 2010; 41:2718–2719.
Article30. Brekenfeld C, Mattle HP, Schroth G. General is better than local anesthesia during endovascular procedures. Stroke. 2010; 41:2716–2717.
Article31. Melsen WG, Rovers MM, Bonten MJ. Ventilator-associated pneumonia and mortality: a systematic review of observational studies. Crit Care Med. 2009; 37:2709–2718.
Article32. Brinjikji W, Pasternak J, Murad MH, Cloft HJ, Welch TL, Kallmes DF, et al. Anesthesia-related outcomes for endovascular stroke revascularization: a systematic review and meta-analysis. Stroke. 2017; 48:2784–2791.33. Li X, Hu Z, Li Q, Guo Y, Xu S, Wang W, et al. Anesthesia for endovascular treatment in anterior circulation stroke: a systematic review and meta-analysis. Brain Behav. 2019; 9:e01178.
Article34. Weber R, Minnerup J, Nordmeyer H, Eyding J, Krogias C, Hadisurya J, et al. Thrombectomy in posterior circulation stroke: Differences in procedures and outcome compared to anterior circulation stroke in the prospective multicentre REVASK registry. Eur J Neurol. 2019; 26:299–305.
Article35. John S, Somal J, Thebo U, Hussain MS, Farag E, Dupler S, et al. Safety and hemodynamic profile of propofol and dexmedetomidine anesthesia during intra-arterial acute stroke therapy. J Stroke Cerebrovasc Dis. 2015; 24:2397–2403.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Alberta Stroke Program Early CT Score in the Prognostication after Endovascular Treatment for Ischemic Stroke: A Meta-analysis
- Anesthetic management for interventional neuroradiology
- Neuroimaging in Randomized, Multi-Center Clinical Trials of Endovascular Treatment for Acute Ischemic Stroke: A Systematic Review