J Korean Acad Nurs.
2019 Apr;49(2):126-136. 10.4040/jkan.2019.49.2.126.
The Effects of Breast Milk Olfactory Stimulation on Physiological Responses, Oral Feeding Progression and Body Weight in Preterm Infants
- Affiliations
-
- 1Department of Nursing, Wonkwang University, Iksan, Korea. ejlee06@wku.ac.kr
- KMID: 2444828
- DOI: http://doi.org/10.4040/jkan.2019.49.2.126
Abstract
- PURPOSE
This study was conducted to evaluate the effect of breast milk olfactory stimulation on physiological responses, oral feeding progression, and body weight in preterm infants.
METHODS
A repeated measures design with nonequivalent control group was used. The participants were healthy, preterm infants born at a gestational age of 28~32 weeks; 12 in the experimental group and 16 in the control group. Data were collected prospectively in the experimental group, and retrospectively in the control group, by the same methods. Breast milk olfactory stimulation was provided 12 times over 15 days. The data were analyzed using the chi-square test, Mann-Whitney U test, Wilcoxon signed rank test and linear mixed models using SPSS 19.
RESULTS
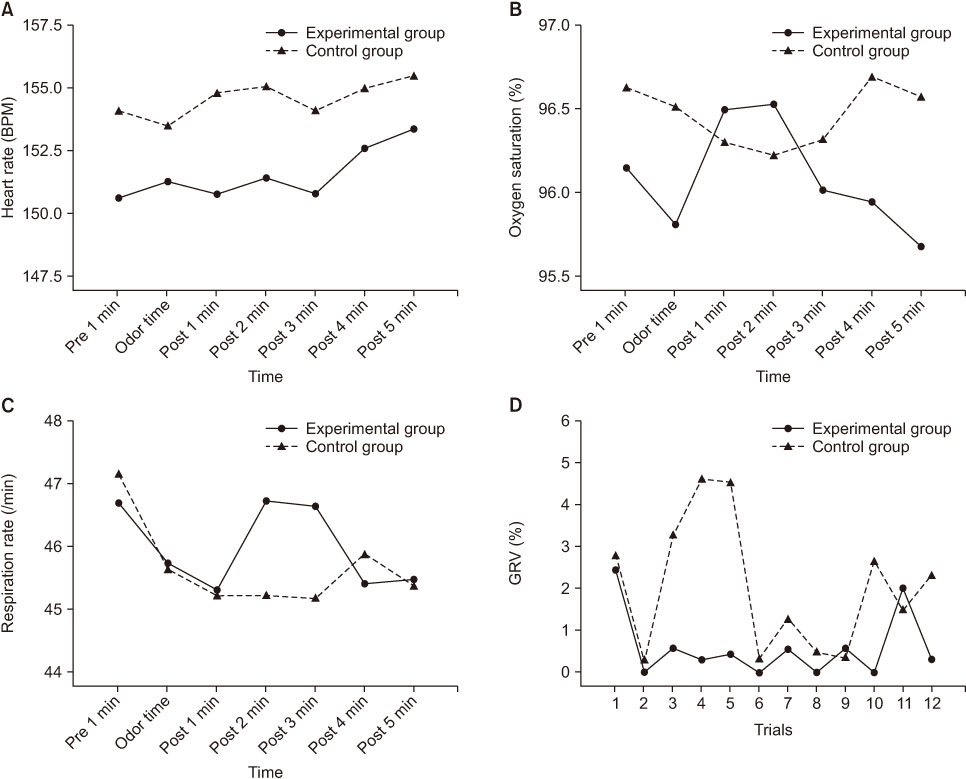
The gastric residual volume (GRV) of the experimental group was significantly less than that of the control group. The heart rate, oxygen saturation, respiration rate, transition time to oral feeding, and body weight were not significantly different between the two groups.
CONCLUSION
These findings indicate that breast milk olfactory stimulation reduces GRV and improves digestive function in preterm infants without inducing distress.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization (WHO). Preterm birth [Internet]. Geneva: WHO;c2018. cited 2018 Jul 18. Available from: http://www.who.int/en/news-room/fact-sheets/detail/preterm-birth.2. Statistics Korea. Birth statistics by gestational age [Internet]. Daejeon: Statistics Korea;c2018. Updated 2018 Aug 22. cited 2015 Dec 14. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B81A15&conn_path=I2\.3. Ministry of Health and Welfare. Preterm infants [Internet]. Sejong: Ministry of Health and Welfare;c2016. cited 2018 Jul 18. Available from: http://health.mw.go.kr/HealthInfoArea/HealthInfo/View.do?idx=3170&subIdx=4&searchCate=&-searchType=&searchKey=&pageNo=&category=&category_code=&dept=&sortType=viewcount&page=1&search-Field=&searchWord=.4. Bang KS, Park JS, Kim JY, Park JY, An HS, Yun BH. Literature review on nursing intervention for premature infants in Korea. Journal of the Korean Society of Maternal and Child Health. 2013; 17(1):49–61. DOI: 10.21896/jksmch.2013.17.1.49.5. Pinelli J, Symington AJ. Cochrane review: Non-nutritive sucking for promoting physiologic stability and nutrition in preterm infants. Evidence-Based Child Health: A Cochrane Review Journal. 2011; 6(4):1134–1169. DOI: 10.1002/ebch.808.
Article6. Dodd VL. Implications of kangaroo care for growth and development in preterm infants. Journal of obstetric, gynecologic, and neonatal nursing. 2005; 34(2):218–232. DOI: 10.1177/0884217505274698.
Article7. Blomqvist YT, Frölund L, Rubertsson C, Nyqvist KH. Provision of kangaroo mother care: Supportive factors and barriers perceived by parents. Scandinavian Journal of Caring Sciences. 2013; 27(2):345–353. DOI: 10.1111/j.1471-6712.2012.01040.x.
Article8. Kim SN, Kim YA, Jeon MH, Kim DS, Kim HI. A systematic review and meta-analysis on the effects of oral stimulation interventions on the transition from tube to oral feeding in premature infants. Journal of Korean Clinical Nursing Research. 2017; 23(2):151–160. DOI: 10.22650/JKCNR.2017.23.2.151.9. Zhao K, Scherer PW, Hajiloo SA, Dalton P. Effect of anatomy on human nasal air flow and odorant transport patterns: Implications for olfaction. Chemical Senses. 2004; 29(5):365–379. DOI: 10.1093/chemse/bjh033.
Article10. Sullivan RM, Toubas P. Clinical usefulness of maternal odor in newborns: Soothing and feeding preparatory responses. Biology of the neonate. 1998; 74(6):402–408. DOI: 10.1159/000014061.
Article11. Goubet N, Rattaz C, Pierrat V, Bullinger A, Lequien P. Olfactory experience mediates response to pain in preterm newborns. Developmental Psychobiology. 2003; 42(2):171–180. DOI: 10.1002/dev.10085.
Article12. Makin JW, Porter RH. Attractiveness of lactating females' breast odors to neonates. Child Development. 1989; 60(4):803–810. DOI: 10.2307/1131020.
Article13. Varendi H, Porter RH, Winberg J. Natural odour preferences of newborn infants change over time. Acta Paediatrica. 1997; 86(9):985–990. DOI: 10.1111/j.1651-2227.1997.tb15184.x.
Article14. Soussignan R, Schaal B, Marlier L, Jiang T. Facial and autonomic responses to biological and artificial olfactory stimuli in human neonates: Re-examining early hedonic discrimination of odors. Physiology & Behavior. 1997; 62(4):745–758. DOI: 10.1016/s0031-9384(97)00187-x.15. Aoyama S, Toshima T, Saito Y, Konishi N, Motoshige K, Ishikawa N, et al. Maternal breast milk odour induces frontal lobe activation in neonates: A NIRS study. Early Human Development. 2010; 86(9):541–545. DOI: 10.1016/j.earlhumdev.2010.07.003.
Article16. Bartocci M, Winberg J, Ruggiero C, Bergqvist LL, Serra G, Lagercrantz H. Activation of olfactory cortex in newborn infants after odor stimulation: A functional near-infrared spectroscopy study. Pediatric Research. 2000; 48(1):18–23. DOI: 10.1203/00006450-200007000-00006.
Article17. Marlier L, Gaugler C, Messer J. Olfactory stimulation prevents apnea in premature newborns. Pediatrics. 2005; 115(1):83–88. DOI: 10.1542/peds.2004-0865.
Article18. Yaghoubi S, Salmani N, Dehghani K, DavoodiZadehJolgeh H. Investigating effect of olfactory stimulation by vanilla on the rate of apnea attacks in neonates with apnea of prematurity: A randomized clinical trial. International Journal of Pediatrics. 2017; 5(12):6221–6229. DOI: 10.22038/ijp.2017.24906.2103.19. Soussignan R, Schaal B, Marlier L. Olfactory alliesthesia in human neonates: Prandial state and stimulus familiarity modulate facial and autonomic responses to milk odors. Developmental Psychobiology. 1999; 35(1):3–14. DOI: 10.1002/(sici)1098-2302(199907)35:1<3::aiddev2>3.0.co;2-f.
Article20. Schriever VA, Gellrich J, Rochor N, Croy I, Cao-Van H, Rüdiger M, et al. Sniffin' away the feeding tube: The influence of olfactory stimulation on oral food intake in newborns and premature infants. Chemical Senses. 2018; 43(7):469–474. DOI: 10.1093/chemse/bjy034.
Article21. Griffin MP, Hansen JW. Can the elimination of lactose from formula improve feeding tolerance in premature infants? The Journal of Pediatrics. 1999; 135(5):587–592. DOI: 10.1016/s0022-3476(99)70057-0.
Article22. Bertino E, Giuliani F, Prandi G, Coscia A, Martano C, Fabris C. Necrotizing enterocolitis: Risk factor analysis and role of gastric residuals in very low birth weight infants. Journal of Pediatric Gastroenterology and Nutrition. 2009; 48(4):437–442. DOI: 10.1097/mpg.0b013e31817b6dbe.
Article23. Armanian AM, Sadeghnia A, Hoseinzadeh M, Mirlohi M, Feizi A, Salehimehr N, et al. The effect of neutral oligosaccharides on reducing the incidence of necrotizing enterocolitis in preterm infants: A randomized clinical trial. International Journal of Preventive Medicine. 2014; 5(11):1387–1395.24. Yildiz A, Arikan D, Gözüm S, Taştekın A, Budancamanak İ. The effect of the odor of breast milk on the time needed for transition from gavage to total oral feeding in preterm infants. Journal of Nursing Scholarship. 2011; 43(3):265–273. DOI: 10.1111/j.1547-5069.2011.01410.x.
Article25. Engle WA. American Academy of Pediatrics Committee on Fetus and Newborn. Age terminology during the perinatal period. Pediatrics. 2004; 114(5):1362–1364. DOI: 10.1542/peds.2004-1915.
Article26. Varendi H, Christensson K, Porter RH, Winberg J. Soothing effect of amniotic fluid smell in newborn infants. Early Human Development. 1998; 51(1):47–55. DOI: 10.1016/S0378-3782(97)00082-0.
Article27. Dorri Y, Sabeghi M, Kurien BT. Awaken olfactory receptors of humans and experimental animals by coffee odourants to induce appetite. Medical Hypotheses. 2007; 69(3):508–509. DOI: 10.1016/j.mehy.2006.12.048.
Article28. Chen SS, Tzeng YL, Gau BS, Kuo PC, Chen JY. Effects of prone and supine positioning on gastric residuals in preterm infants: A time series with cross-over study. International Journal of Nursing Studies. 2013; 50(11):1459–1467. DOI: 10.1016/j.ijnurstu.2013.02.009.
Article29. Hung HY, Hsu YY, Chang YJ. Comparison of physiological and behavioral responses to fresh and thawed breastmilk in premature infants: A preliminary study. Breastfeeding Medicine. 2013; 8(1):92–98. DOI: 10.1089/bfm.2012.0026.30. Van Reempts PJ, Wouters A, De Cock W, Van Acker KJ. Stress responses to tilting and odor stimulus in preterm neonates after intrauterine conditions associated with chronic stress. Physiology & Behavior. 1997; 61(3):419–424. DOI: 10.1016/S0031-9384(96)00453-2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Enteral Feeding for Preterm Infants-Benefits and Risks
- Incidence of Postnatal CMV Infection among Breastfed Preterm Infants: a Systematic Review and Meta-analysis
- Breast Feeding Rates and Factors Influencing Breast Feeding Practice in Late Preterm Infants: Comparison with Preterm Born at Less than 34 Weeks of Gestational Age
- The Research on the Breast Feeding and its Related Factors of Premature Infant
- Analysis of the Macronutrient Composition of Breast Milk from Korean Women and Growth of Infants