Brain Tumor Res Treat.
2019 Apr;7(1):57-61. 10.14791/btrt.2019.7.e22.
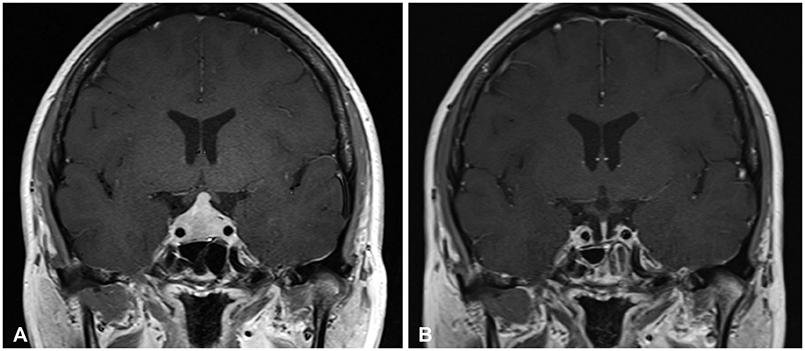
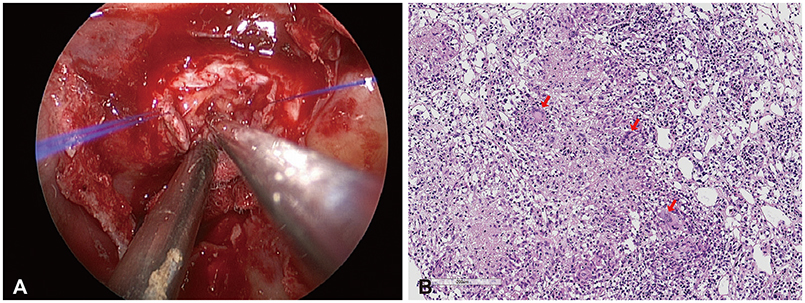
Idiopathic Granulomatous Hypophysitis with Rapid Onset: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea. kimyh96@snu.ac.kr
- 2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 3Pituitary Center, Seoul National University College of Medicine, Seoul, Korea.
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2444798
- DOI: http://doi.org/10.14791/btrt.2019.7.e22
Abstract
- Idiopathic granulomatous hypophysitis (IGH), a rare disease, requires differentiation from more common mass lesions of the sella such as pituitary adenoma, craniopharyngioma, Rathke's cleft cyst, or pituitary tuberculoma. IGH usually presents with an insidious onset of visual defects and headaches. On the other hand, rapid onset of neurologic and visual symptoms in an IGH patient is exceptionally rare. Here, we present a biopsy-proven case of IGH with rapid onset and satisfactory outcome after high dose steroid treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Srisukh S, Tanpaibule T, Kiertiburanakul S, et al. Pituitary tuberculoma: a consideration in the differential diagnosis in a patient manifesting with pituitary apoplexy-like syndrome. IDCases. 2016; 5:63–66.
Article2. Majumdar K, Barnard M, Ramachandra S, Berovic M, Powell M. Tuberculosis in the pituitary fossa: a common pathology in an uncommon site. Endocrinol Diabetes Metab Case Rep. 2014; 2014:140091.
Article3. Faje A. Hypophysitis: evaluation and management. Clin Diabetes Endocrinol. 2016; 2:15.
Article4. Hunn BH, Martin WG, Simpson S Jr, Mclean CA. Idiopathic granulomatous hypophysitis: a systematic review of 82 cases in the literature. Pituitary. 2014; 17:357–365.
Article5. Husain Q, Zouzias A, Kanumuri VV, Eloy JA, Liu JK. Idiopathic granulomatous hypophysitis presenting as pituitary apoplexy. J Clin Neurosci. 2014; 21:510–512.
Article6. Rickards AG, Barrett GM. Nontuberculous Addison’s disease and its relationship to giant-cell granuloma and multiple glandular disease. Q J Med. 1954; 23:403–423.7. Osawa S, Ogawa Y, Watanabe M, Tominaga T. Hypophysitis presenting with atypical rapid deterioration: with special reference to immunoglobulin G4-related disease-case report. Neurol Med Chir (Tokyo). 2009; 49:622–625.
Article8. Alam T, Thomas S. Diabetes insipidus secondary to sarcoidosis presenting with caseating granuloma. BMJ Case Rep. 2011; 2011:bcr0120113702.
Article9. Al-Haddad S, Fandino R, Scheithauer BW, Galvis L, Syro LV, Kovacs K. Necrotizing granulomatous hypophysitis presenting as a sellar mass. Endocr Pathol. 2011; 22:6–9.
Article10. Ben Abid F, Abukhattab M, Karim H, Agab M, Al-Bozom I, Ibrahim WH. Primary pituitary tuberculosis revisited. Am J Case Rep. 2017; 18:391–394.
Article11. Antony G, Dasgupta R, Chacko G, Thomas N. Pituitary tuberculoma with subsequent drug-resistant tuberculous lymphadenopathy: an uncommon presentation of a common disease. BMJ Case Rep. 2017; 2017:bcr2016218330.
Article12. Shukla S, Trivedi A, Singh K, Sharma V. Pituitary tuberculoma. J Neurosci Rural Pract. 2010; 1:30–31.
Article13. Tanimoto K, Imbe A, Shishikura K, et al. Reversible hypopituitarism with pituitary tuberculoma. Intern Med. 2015; 54:1247–1251.
Article14. Saito K, Toda M, Shido S, Tomita T, Ogawa K, Yoshida K. Isolated pituitary tuberculoma. NMC Case Rep J. 2014; 1:33–36.
Article15. Kong X, Wang R, Yang Y, et al. Idiopathic granulomatous hypophysitis mimicking pituitary abscess. Medicine (Baltimore). 2015; 94:e1099.
Article16. Çavuşoğlu M, Elverici E, Duran S, Komut E, Güreşçi S, Sakman B. Idiopathic granulomatous hypophysitis: a rare cystic lesion of the pituitary. Intern Med. 2015; 54:1407–1410.
Article17. Iseda I, Hida K, Tone A, et al. Prednisolone markedly reduced serum IgG4 levels along with the improvement of pituitary mass and anterior pituitary function in a patient with IgG4-related infundibulo-hypophysitis. Endocr J. 2014; 61:195–203.
Article18. Leung GK, Lopes MB, Thorner MO, Vance ML, Laws ER Jr. Primary hypophysitis: a single-center experience in 16 cases. J Neurosurg. 2004; 101:262–271.
Article19. Wan Muhamad Hatta SF, Hamdan MF, Md Ali SA, Abdul Ghani R. Granulomatous hypophysitis: a case of severe headache. BMJ Case Rep. 2016; 2016:bcr2016216395.
Article20. Kristof RA, van Roost D, Schramm J, Wichers M. Primary granulomatous hypophysitis not responsive to pulsed high dose prednisolone therapy: case report. J Neurol Neurosurg Psychiatry. 1998; 64:693–694.
Article21. Ved R, Logier N, Leach P, Davies JS, Hayhurst C. Pituitary xanthogranulomas: clinical features, radiological appearances and post-operative outcomes. Pituitary. 2018; 21:256–265.
Article22. Su SB, Zhang DJ, Yue SY, Zhang JN. Primary granulomatous hypophysitis: a case report and literature review. Endocr J. 2011; 58:467–473.
Article23. Scanarini M, d'Avella D, Rotilio A, Kitromilis N, Mingrino S. Giantcell granulomatous hypophysitis: a distinct clinicopathological entity. J Neurosurg. 1989; 71(5 Pt 1):681–686.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Granulomatous Hypophysitis
- Primary Granulomatous Hypophysitis Presenting with Panhypopituitarism and Central Diabetes Insipidus
- A Case of Idiopathic Granulomatous Hypophysitis
- Lymphocytic Hypophysitis Presenting with Diabetes Insipidus in a Man: Report of a case
- Lymphocytic Hypophysitis: A Cases Report