J Korean Orthop Assoc.
2019 Apr;54(2):182-186. 10.4055/jkoa.2019.54.2.182.
Surgical Treatment of Recurrent Giant Cell Tumor Occurring at the First Metatarsal
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Eulji University, Daejeon, Korea. oskkj@eulji.ac.kr
- KMID: 2444785
- DOI: http://doi.org/10.4055/jkoa.2019.54.2.182
Abstract
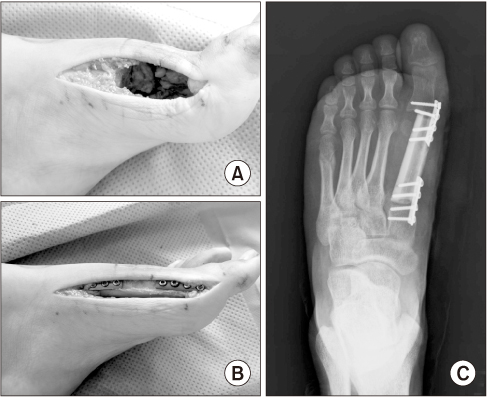
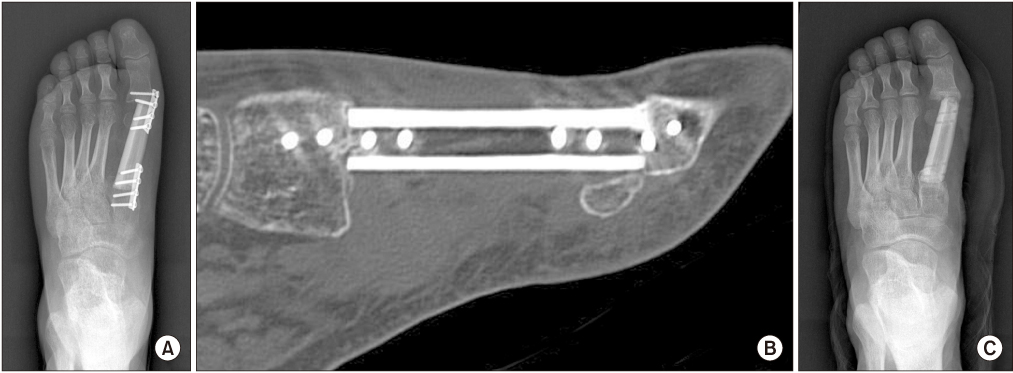
- Giant cell tumor is a benign but locally aggressive tumor with common recurrence. Most cases occur around the knee joint. Giant cell tumor of the foot is rare and very few cases involving the first metatarsal have been reported. Its characteristics and treatment in adult patients remain unclear. This paper reports a case of recurrent giant cell tumor at the first metatarsal that was excised surgically and subsequently reconstructed with non-vascularized fibula graft.
Keyword
MeSH Terms
Figure
Reference
-
1. Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg Am. 1987; 69:106–114.
Article2. Rajani R, Schaefer L, Scarborough MT, Gibbs CP. Giant cell tumors of the foot and ankle bones: high recurrence rates after surgical treatment. J Foot Ankle Surg. 2015; 54:1141–1145.
Article3. Siddiqui YS, Zahid M, Bin Sabir. Giant cell tumor of the first metatarsal. J Cancer Res Ther. 2011; 7:208–210.
Article4. Ly JQ, Arnett GW, Beall DP. Case 122: giant cell tumor of the second metatarsal. Radiology. 2007; 245:288–291.
Article5. Turcotte RE. Giant cell tumor of bone. Orthop Clin North Am. 2006; 37:35–51.
Article6. Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ. From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: radiologic-pathologic correlation. Radiographics. 2001; 21:1283–1309.7. O'Keefe RJ, O'Donnell RJ, Temple HT, Scully SP, Mankin HJ. Giant cell tumor of bone in the foot and ankle. Foot Ankle Int. 1995; 16:617–623.8. Unni KK, Dahlin DC. Dahlin's bone tumors: general aspects and data on 11,087 cases. 5th ed. Philadelphia: Lippincott-Raven;1996. p. 263–283.9. Balaji GG, Roy AC, Justin SV. Techniques in recurrent giant cell tumour of the first metatarsal in adolescents - A rare report of 2 cases. Foot Ankle Surg. 2013; 19:e1–e4.
Article