Investig Clin Urol.
2019 May;60(3):216-221. 10.4111/icu.2019.60.3.216.
Friction underwear for ease of pulling down in elderly patients with overactive bladder: A prospective randomized control trial
- Affiliations
-
- 1Department of Urology, Chonbuk National University Medical School, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute and Clinical Trial Center of Medical Device of Chonbuk National University Hospital, Jeonju, Korea. rain@chonbuk.ac.kr
- 2Department of Physical Medicine and Rehabilitation, Chonbuk National University Medical School, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute and Clinical Trial Center of Medical Device of Chonbuk National University Hospital, Jeonju, Korea.
- 3Department of Industrial and Management Engineering, Pohang University of Science and Technology, Pohang, Korea.
- KMID: 2444277
- DOI: http://doi.org/10.4111/icu.2019.60.3.216
Abstract
- PURPOSE
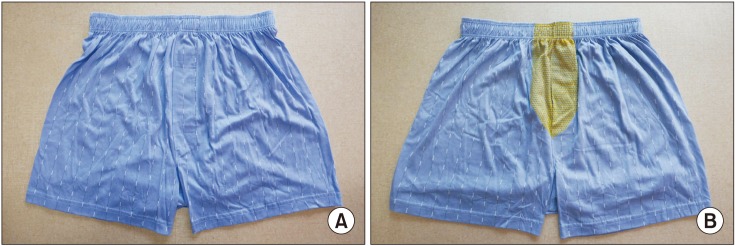
Friction underwear was developed by adding small silicon dots in front of the underwear to decrease the time for pulling down underwear in elderly patients with urge incontinence. We studied about the effects of the friction underwear for elderly overactive bladder (OAB) patients.
MATERIALS AND METHODS
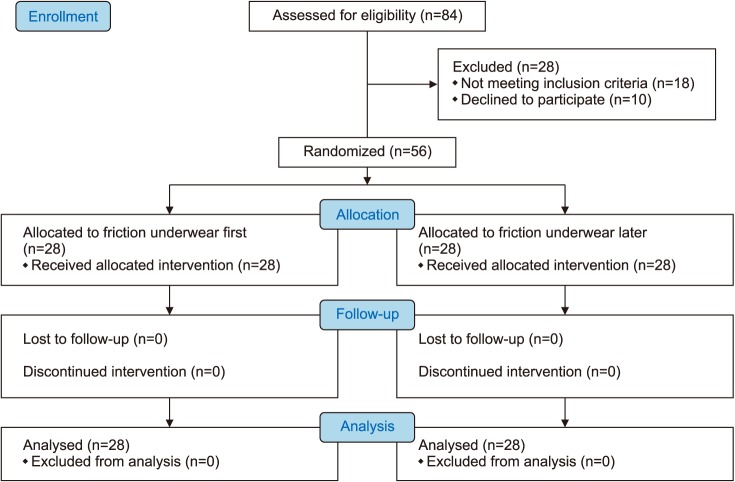
Male patients over 60 years of age diagnosed with OAB were prospectively enrolled and randomized to either the friction underwear first group (measuring for the time taken to pull down the friction underwear first and the non-friction underwear second) or the friction underwear later group (non-friction underwear first and the friction underwear second). An investigator measured the time to pulling down the underwear. And we measured the coefficient of friction of underwear.
RESULTS
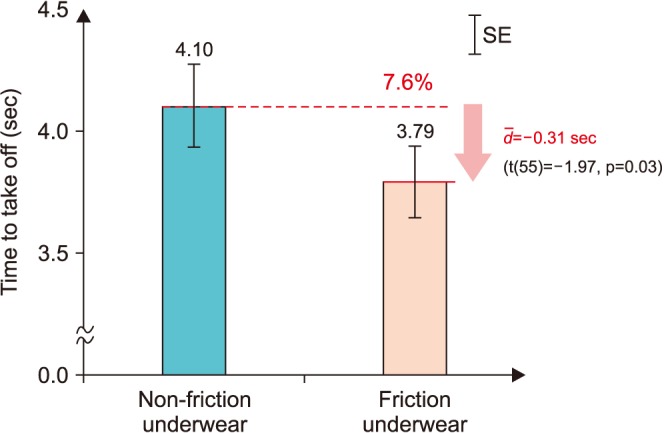
A total of 56 male patients were randomly divided into two groups using a random number table envelope method. There were no significant differences in demographics and clinical characteristics between the two groups. Of the total 56 patients, the time taken to pull down underwear for the friction underwear (3.79±0.15 seconds) was found significantly shorter than that for the non-friction underwear (4.10±0.17 seconds) (p=0.03). The static and dynamic coefficients of friction of the friction were 4.21 and 2.88, respectively, while those of the non-friction underwear were 0.64 and 0.45, respectively.
CONCLUSIONS
Our study demonstrates that friction underwear significantly shortened the time to pull down underwear. This functional underwear may be effective in preventing the underwear from getting wet in patients who suffer from urge incontinence.
MeSH Terms
Figure
Reference
-
1. Abrams P, Artibani W, Cardozo L, Dmochowski R, van Kerrebroeck P, Sand P. International Continence Society. Reviewing the ICS 2002 terminology report: the ongoing debate. Neurourol Urodyn. 2009; 28:287. PMID: 19350662.
Article2. Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012; 80:90–96. PMID: 22748867.
Article3. Sexton CC, Coyne KS, Kopp ZS, Irwin DE, Milsom I, Aiyer LP, et al. EpiLUTS Team. The overlap of storage, voiding and post-micturition symptoms and implications for treatment seeking in the USA, UK and Sweden: EpiLUTS. BJU Int. 2009; 103(Suppl 3):12–23. PMID: 19302498.
Article4. Irwin DE, Milsom I, Chancellor MB, Kopp Z, Guan Z. Dynamic progression of overactive bladder and urinary incontinence symptoms: a systematic review. Eur Urol. 2010; 58:532–543. PMID: 20573443.
Article5. Carmeli E, Patish H, Coleman R. The aging hand. J Gerontol A Biol Sci Med Sci. 2003; 58:146–152. PMID: 12586852.
Article6. White-Chu EF, Reddy M. Dry skin in the elderly: complexities of a common problem. Clin Dermatol. 2011; 29:37–42. PMID: 21146730.
Article7. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–191. PMID: 17695343.8. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314. PMID: 17049716.
Article9. Huh JS, Kim YJ, Kim SD. Prevalence of benign prostatic hyperplasia on Jeju Island: analysis from a cross-sectional community-based survey. World J Mens Health. 2012; 30:131–137. PMID: 23596600.
Article10. Choi HC, Kwon JK, Lee JY, Han JH, Jung HD, Cho KS. Seasonal variation of urinary symptoms in korean men with lower urinary tract symptoms and benign prostatic hyperplasia. World J Mens Health. 2015; 33:81–87. PMID: 26331124.
Article11. Coyne KS, Sexton CC, Bell JA, Thompson CL, Dmochowski R, Bavendam T, et al. The prevalence of lower urinary tract symptoms (LUTS) and overactive bladder (OAB) by racial/ethnic group and age: results from OAB-POLL. Neurourol Urodyn. 2013; 32:230–237. PMID: 22847394.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Bladder Training, Tolterodine and Bladder Training with Tolterodine in Female Patients with Overactive Bladder: Prospective, Randomized Study
- A Case of Keratosis Follicularis Squamosa Occurring on the Underwear Friction Area
- Overactive Bladder
- Therapeutic Effects of Prolonged Release Melatonin (Circadin® ) in Patients with Overactive Bladder and Chronic Insomnia in More Than 55 Years Old
- Evaluation of the Wearing Characteristics of Hip Protectors Based on Draping Pattern Design and Body Shape in Korean Elderly People