Investig Clin Urol.
2019 May;60(3):184-194. 10.4111/icu.2019.60.3.184.
Trends in clinical, operative, and pathologic characteristics of surgically treated renal mass in a Korean center: A surgical series from 1988 through 2015
- Affiliations
-
- 1Department of Urology, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea. urokyj@cbnu.ac.kr
- 2Department of Urology, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 3Department of Urology, Korea University School of Medicine, Seoul, Korea.
- 4Department of Urology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 5Department of Urology, National Cancer Center, Goyang, Korea.
- 6Department of Urology, Kyungpook National University College of Medicine, Daegu, Korea.
- 7Department of Urology, Seoul National University College of Medicine, Seoul, Korea.
- 8Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2444273
- DOI: http://doi.org/10.4111/icu.2019.60.3.184
Abstract
- PURPOSE
To analyze trends over a period of 28 years in the clinical, operative, and pathologic characteristics of patients with a renal mass who underwent surgical resection in Korea.
MATERIALS AND METHODS
Consecutive patients (n=6,231) with a renal mass who underwent surgical resection at eight Korean institutions between 1988 and 2015 were reviewed. Patients were assigned to one of three groups according to the date of surgery: group 1, 1988-1999; group 2, 2000-2009; and group 3, 2010-2015.
RESULTS
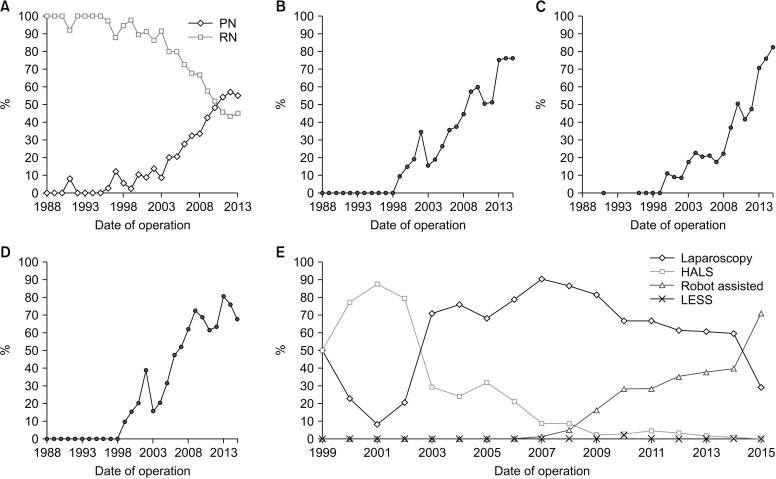
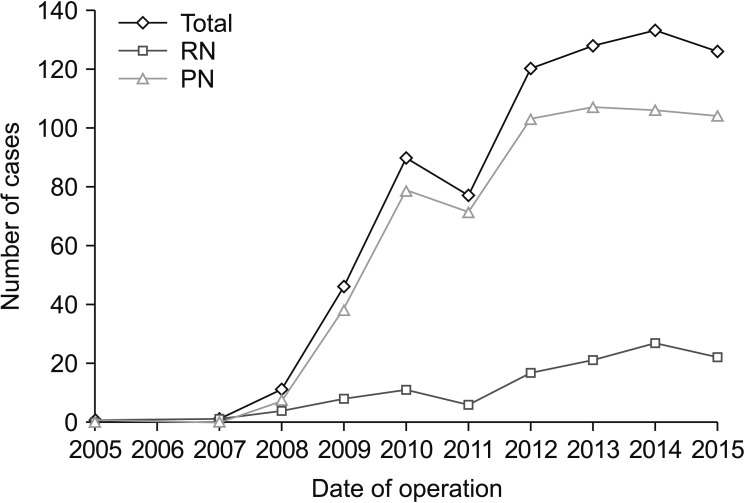
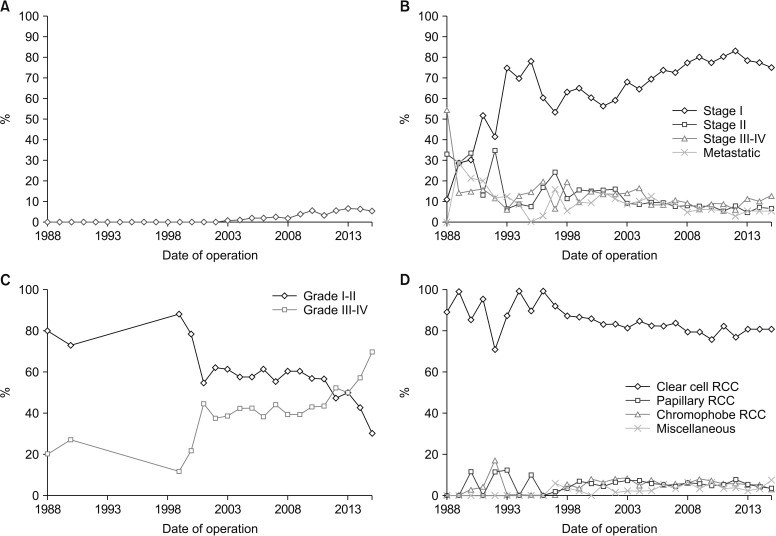
Age at the time of surgery, body mass index, smoking status, incidence of diabetes and hypertension, and the number of incidentally identified renal masses increased significantly over time. The proportion of patients undergoing partial nephrectomy (PN) or minimally invasive surgery (MIS) increased sharply during the last two time periods. From 2010, the rate of robot-assisted nephrectomy rose sharply, occurring in 37.8% of MIS cases. Benign pathology was identified in 1.8% and 5.2% of cases in the middle and last periods, respectively; angiomyolipoma was the most common pathology. In later years, tumors were more often localized, although tumor grade increased. Sub-group analysis of small renal masses ≤4 cm revealed similar trends in operative and pathologic characteristics over time.
CONCLUSIONS
Between 1988 and 2015, there was a substantial change in the clinical, operative, and histological characteristics of patients who underwent resection of a renal mass in Korea. The most notable changes were stage migration towards localized disease and widespread use of PN and MIS.
Keyword
MeSH Terms
Figure
Reference
-
1. Byun SS, Hong SK, Lee S, Kook HR, Lee E, Kim HH, et al. The establishment of KORCC (Korean renal cell carcinoma) database. Investig Clin Urol. 2016; 57:50–57.
Article2. Stafford HS, Saltzstein SL, Shimasaki S, Sanders C, Downs TM, Sadler GR. Racial/ethnic and gender disparities in renal cell carcinoma incidence and survival. J Urol. 2008; 179:1704–1708. PMID: 18343443.
Article3. Kane CJ, Mallin K, Ritchey J, Cooperberg MR, Carroll PR. Renal cell cancer stage migration: analysis of the National Cancer Data Base. Cancer. 2008; 113:78–83. PMID: 18491376.4. Mir MC, Derweesh I, Porpiglia F, Zargar H, Mottrie A, Autorino R. Partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: a systematic review and meta-analysis of comparative studies. Eur Urol. 2017; 71:606–617. PMID: 27614693.
Article5. Patel HD, Mullins JK, Pierorazio PM, Jayram G, Cohen JE, Matlaga BR, et al. Trends in renal surgery: robotic technology is associated with increased use of partial nephrectomy. J Urol. 2013; 189:1229–1235. PMID: 23085300.
Article6. Weise ES, Winfield HN. Laparoscopic partial nephrectomy. J Endourol. 2005; 19:634–642. PMID: 16053351.
Article7. Gill IS, Desai MM, Kaouk JH, Meraney AM, Murphy DP, Sung GT, et al. Laparoscopic partial nephrectomy for renal tumor: duplicating open surgical techniques. J Urol. 2002; 167:469–467. discussion 475–6. PMID: 11792899.
Article8. Gill IS, Kavoussi LR, Lane BR, Blute ML, Babineau D, Colombo JR Jr, et al. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol. 2007; 178:41–46. PMID: 17574056.
Article9. Benway BM, Bhayani SB, Rogers CG, Dulabon LM, Patel MN, Lipkin M, et al. Robot assisted partial nephrectomy versus laparoscopic partial nephrectomy for renal tumors: a multi-institutional analysis of perioperative outcomes. J Urol. 2009; 182:866–872. PMID: 19616229.
Article10. Rogers CG, Singh A, Blatt AM, Linehan WM, Pinto PA. Robotic partial nephrectomy for complex renal tumors: surgical technique. Eur Urol. 2008; 53:514–521. PMID: 17961910.
Article11. Miller DC, Ruterbusch J, Colt JS, Davis FG, Linehan WM, Chow WH, et al. Contemporary clinical epidemiology of renal cell carcinoma: insight from a population based case-control study. J Urol. 2010; 184:2254–2258. PMID: 20952033.
Article12. Johnson DC, Vukina J, Smith AB, Meyer AM, Wheeler SB, Kuo TM, et al. Preoperatively misclassified, surgically removed benign renal masses: a systematic review of surgical series and United States population level burden estimate. J Urol. 2015; 193:30–35. PMID: 25072182.
Article13. Kang HW, Seo SP, Kim WT, Yun SJ, Lee SC, Kim WJ, et al. Impact of young age at diagnosis on survival in patients with surgically treated renal cell carcinoma: a multicenter study. J Korean Med Sci. 2016; 31:1976–1982. PMID: 27822938.
Article14. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474. PMID: 20180029.
Article15. Fuhrman SA, Lasky LC, Limas C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol. 1982; 6:655–663. PMID: 7180965.
Article16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.17. King SC, Pollack LA, Li J, King JB, Master VA. Continued increase in incidence of renal cell carcinoma, especially in young patients and high grade disease: United States 2001 to 2010. J Urol. 2014; 191:1665–1670. PMID: 24423441.
Article18. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–E386. PMID: 25220842.
Article19. Joung JY, Lim J, Oh CM, Jung KW, Cho H, Kim SH, et al. Current trends in the incidence and survival rate of urological cancers in Korea. Cancer Res Treat. 2017; 49:607–615. PMID: 27658388.
Article20. Dulabon LM, Lowrance WT, Russo P, Huang WC. Trends in renal tumor surgery delivery within the United States. Cancer. 2010; 116:2316–2321. PMID: 20225227.
Article21. Golombos DM, Chughtai B, Trinh QD, Thomas D, Mao J, Te A, et al. Minimally invasive vs open nephrectomy in the modern era: does approach matter? World J Urol. 2017; 35:1557–1568. PMID: 28477204.
Article22. Banegas MP, Harlan LC, Mann B, Yabroff KR. Toward greater adoption of minimally invasive and nephron-sparing surgical techniques for renal cell cancer in the United States. Urol Oncol. 2016; 34:433.e9–433.e17.
Article23. Ghani KR, Sukumar S, Sammon JD, Rogers CG, Trinh QD, Menon M. Practice patterns and outcomes of open and minimally invasive partial nephrectomy since the introduction of robotic partial nephrectomy: results from the nationwide inpatient sample. J Urol. 2014; 191:907–912. PMID: 24184365.
Article24. Pignot G, Méjean A, Bernhard JC, Bigot P, Timsit MO, Ferriere JM, et al. CCAFU members. The use of partial nephrectomy: results from a contemporary national prospective multicenter study. World J Urol. 2015; 33:33–40. PMID: 24663965.
Article25. Thompson RH, Kaag M, Vickers A, Kundu S, Bernstein M, Lowrance W, et al. Contemporary use of partial nephrectomy at a tertiary care center in the United States. J Urol. 2009; 181:993–997. PMID: 19150552.
Article26. Jeon HG, Lee SR, Kim KH, Oh YT, Cho NH, Rha KH, et al. Benign lesions after partial nephrectomy for presumed renal cell carcinoma in masses 4 cm or less: prevalence and predictors in Korean patients. Urology. 2010; 76:574–579. PMID: 20303148.
Article27. Corcoran AT, Russo P, Lowrance WT, Asnis-Alibozek A, Libertino JA, Pryma DA, et al. A review of contemporary data on surgically resected renal masses--benign or malignant? Urology. 2013; 81:707–713. PMID: 23453080.
Article28. Leibovich BC, Lohse CM, Crispen PL, Boorjian SA, Thompson RH, Blute ML, et al. Histological subtype is an independent predictor of outcome for patients with renal cell carcinoma. J Urol. 2010; 183:1309–1315. PMID: 20171681.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Renal Cell Carcinoma: Clinical, Radiologic and Pathologic Characteristics
- A Clinical Analysis of 81 Cases of Arseriovenous Malformations
- The Characteristics of Renal Trauma Patients Who Needed Surgical Management
- Clinical Characteristics of Incidentally Detected Renal Cell Carcinoma
- Current Status of Renal Biopsy for Small Renal Masses